Abstract
Objective
To evaluate the safety and efficacy of gonioscopy-assisted transluminal trabeculotomy (GATT) using a marker suture which could be a viable low cost alternative to an illuminated micro catheter, by helping the surgeon identify obstruction to suture passage, and estimate the degree of Schlemm’s canal cannulated.
Subject/Methods
Thirty four eyes with 360° of open angles with uncontrolled IOP despite maximal medical therapy, non-compliant to medical therapy or failed incisional glaucoma surgery underwent GATT. 5-0 or 6-0 Prolene® suture was used to cannulate Schlemm’s canal. An 8-0 Vicryl® suture was tied around the trailing portion of the Prolene® suture and acted as a guide to estimate the length of Schlemm’s canal negotiated. The degree of trabecular shelf seen was noted postoperatively.
Results
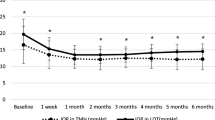
Mean baseline IOP was 24.7 ± 8.8 mm Hg (range 13–54 mmHg). Six patients had appositional angle closure and the rest had open angles. Patients were followed up for a period of 45.0 ± 14.6weeks (range 6 weeks-2 years). The mean IOP 6 weeks after surgery was 13 ± 3.3 mm Hg, and at 1 year was 13.5 ± 2.6 mm Hg. Mean degrees of cannulation achieved was 264.5 ± 84.0˚ (90-360˚). The mean number of medications prior to surgery was 2.1 ± 1.0 and at 6 months review was 0.15 ± 0.3. The absolute success was 92.6% 1 year after surgery. Nine patients lost some of their trabecular shelf in the postoperative period, but this did not seem to affect the short term success rate.
Discussion
Suture GATT is a safe and effective procedure to lower IOP even in patients with partial cannulation. Adding a marker suture is a useful adjunct to help identify the length of Schlemm’s canal successfully cannulated and monitor progress of the Prolene® suture.
Similar content being viewed by others
Introduction
There has been a recent surge in interest for the Gonioscopy-assisted Transluminal Trabeculotomy (GATT) technique. GATT is a conjunctiva sparing micro-invasive procedure which aims to create a direct conduit for aqueous outflow from the anterior chamber to the collector channels by cleaving the trabecular meshwork and the inner wall of Schlemm’s canal. Grant WM [1] found that much of the resistance to aqueous outflow is in the trabecular meshwork-canal area and he reported a 75% reduction in resistance after trabeculotomy. High success rates have been reported in previous studies [1,2,3,4,5].
Grover et al. [2] described the use of a lighted microcatheter to cannulate and negotiate Schlemm’s canal in adult patients with open angle glaucoma. He also reported GATT as a successful method that revives the downstream collector system in eyes that have undergone prior incisional surgeries [3]. The use of an illuminated micro-catheter is advantageous as the surgeon can monitor location of the tip in real time. Misdirection posteriorly, extrusion into the anterior chamber or into the collector channels can be easily identified. However, fibre optic micro-catheters are expensive. The use of a suture to cannulate Schlemm’s canal (4-0 Nylon/5-0 or 6-0 Prolene®) is cost effective, but it is difficult to monitor the progress. Grover et al. [4] suggested the use of a 4-0 clear nylon suture after marking its tip with dye in a single patient. The suture tip marked with dye could be seen through the sclera. The suture is not widely available and its visibility through sclera has not been confirmed in a large series or in highly pigmented eyes. We propose adding a marker suture with 8-0 Vicryl® to the Prolene® suture used for cannulation. This could potentially help the surgeon/assistant monitor the advancement of the Prolene® suture, help identify obstruction to suture movement and serve as a guide to the length of the Schlemm’s canal cannulated, so that a site for goniotomy (to retrieve the distal end of the Prolene® suture) can be identified.
We tried GATT with the use of 5-0/6-0 Prolene® suture. An 8-0 Vicryl® suture was tied around the trailing portion of the Prolene® suture and served as a guide to the length that was cannulated.
Material and methods
Patients with open angle glaucoma who underwent GATT alone or GATT combined with phacoemulsification with IOL implantation from February 2019 to August 2020 were retrospectively analysed. Patients with uncontrolled IOP despite maximal medical therapy (four or more topical medications—typically a prostaglandin, timolol, brimonidine, and carbonic anhydrase inhibitor were used, beta blockers were avoided in patients with cardiac ailment or severe respiratory insufficiency), significant progression in visual fields and those who could not tolerate or were non-compliant to medical therapy were scheduled for GATT.A preoperative gonioscopy was done in all patients with a four mirror indirect Goniolens. Only those with clearly visible landmarks (trabecular meshwork and scleral spur) in all four quadrants were included. Patients with glaucoma and narrow anterior chamber angle were included when the angle opened 360° on indentation (with occasional peripheral anterior synechiae if any) and clear identifiable landmarks were present. Phacoemulsification with IOL implantation was combined when a visually significant cataract was present. Patients with bleeding tendencies, anticoagulants/antiplatelet drugs (when these could not be stopped prior to surgery) and conditions that precluded positioning of the patient for GATT (e.g. cervical spondylosis) were excluded.
All patients underwent a comprehensive ophthalmic examination which included visual acuity, refraction, anterior and posterior segment examination, perimetry, and optical coherence tomography. The staging of glaucoma was based on visual fields (Hoddap –Parrish –Anderson criteria [6]), a mean deviation of >-12 dB was taken as advanced glaucoma, between -6 and -12 dB as moderate glaucoma and <-6 dB as mild glaucoma.
The study was approved by the institutional review board of our hospital and adhered to the tenets of declaration of Helsinki. All surgeries were done under topical anaesthesia with surgical asepsis by the second author. The patient continued anti-glaucoma medications till the day before surgery. The surgeon sat on the temporal side. Two side ports were placed, one on the left side two clock hours away for passing the suture and the other on the right side for micro-rhexis forceps (Video 1). When phacoemulsification with IOL implantation was needed, it was done through a temporal clear corneal incision before attempting GATT. 0.5 cc of intracameral preservative free lignocaine was injected and the anterior chamber inflated with ophthalmic viscosurgical device (OVD). The patient’s head was tilted to the opposite side, the patient asked to look towards the opposite side and the microscope tilted towards the surgeon. Of, 2% hydroxypropylmethylcellulose was placed on the cornea as a coupling agent along with a Hill goniolens. The tip of 5-0/6-0 Prolene® was blunted with light cautery and inserted through the left side port till it was close to the angle. Under gonioscopic guidance, a microvitreoretinal(MVR) blade was advanced through the right side port and the trabecular meshwork incised to expose Schlemm’s canal. A micro-rhexis forceps was inserted through the right side port to grasp the 6-0 Prolene® suture and insert it into Schlemm’s canal. After insertion, an 8-0 vicryl was tied around the trailing portion of the Prolene® suture and placed at a distance corresponding to 360° cannulation by superimposing the suture over the cornea (Video 1). Under gonioscopic control, the 6-0 Prolene® suture was grasped near the incision on the trabecular meshwork and advanced by small controlled movements. The assisting nurse monitored the movement of the Vicryl® suture. When the movement of the Prolene® suture stopped, an attempt was made to advance it by grasping it close to the goniotomy site. If further advancement could not be made, the approximate distance of cannulation was judged by noting the distance of the marker suture from the side port. If more than half of Schlemm’s canal had been cannulated, a goniotomy was done 180° away to retrieve the suture. The blunted tip of the Prolene® suture helped anchor it in Schlemm’s canal so that trabeculotomy was done for the entire distance cannulated (Video 2, 3). When the marker suture was near the side port and the tip of the Prolene® was not seen, a gonioscopy was done to locate the position of the Prolene suture. If 360° cannulation was successful and the suture tip was seen, it was retrieved and the two suture ends pulled in opposite direction to complete the trabeculotomy. If the suture tip extruded out into the anterior chamber, it was pulled to complete a partial trabeculotomy. The blood and OVD was washed from the anterior chamber and behind the IOL. The side ports were hydrated. 0.1 cc of preservative free moxifloxacin was injected into the anterior chamber. An air bubble was placed in the anterior chamber along with a 25% fill of 1% sodium hyaluronate OVD. The eye was padded for a couple of hours. Postoperatively, patients were placed on topical loteprednol starting 8 times a day and tapered over 8 weeks, pilocarpine 2% four times a day for 1 month and topical moxifloxacin 4 times a day for 1 week. Patients were reviewed on the first postoperative day, first postoperative week, and at six weeks post-operatively. At each visit, the visual acuity, applanation IOP, anterior chamber details and fundus findings were recorded. Gonioscopy was done at three months to check the extent of the trabecular shelf. Subsequent reviews were timed based on the extent of glaucomatous damage. An IOP drop >20% post operatively from the baseline without the need for anti-glaucoma medications was considered as absolute success. Attainment of the same with a maximum of two topical medications was considered as qualified success. Patients who achieved less than 20% drop or needed additional surgery to control the IOP were considered as failures.
Descriptive analysis was carried out by mean and standard deviation for quantitative variables, frequency and proportion for categorical variables. For normally distributed data, the change in the quantitative parameters before and after the intervention was assessed by paired t-test and by Wilcoxon signed rank test. A P value < 0.05 was considered statistically significant. IBM SPSS version 22 (IBM Corp, NY) was used for statistical analysis
Results
GATT was done in 34 eyes (32patients) between February2019 and August 2020.Patient characteristics are mentioned in Table 1. The mean age was 64.9 ± 8.2 years. The mean baseline IOP was 24.7 ± 8.8 mm Hg (range 13-54 mm Hg). Six patients had appositional angle closure and the rest had open angles. Mild visual field damage was noted in 20patients (58.8%), moderate damage in 9patients (26.5%), and severe damage in 5patients (14.7%). Thirty eyes underwent combined phacoemulsification with IOL implantation and GATT, while 4 eyes underwent GATT alone. One patient had a failed trabeculectomy, and another patient had uncontrolled IOP after a failed trabeculectomy and implantation of Aurolab Aqueous Drainage Implant® two years later. In the third patient, trabeculectomy was abandoned by a trainee surgeon because of premature entry into the anterior chamber while dissecting the scleral flap. In the first 6 patients in the series, 5-0 Prolene® was used. Then we switched to 6-0 Prolene® as it was less stiff.
360° cannulation was achieved in 12 patients (35.3%), between 180 and 270° in 20 patients (58.8%) and 90° in two patients (5.9%) (Mean cannulation: 264.5 ± 84.0˚).The position of the marker suture helped locate the distal tip and guide the goniotomy–Video 2 & 3.In the two patients with 90° GATT, obstruction was noted shortly after cannulating Schlemm’s canal and cannulation in the reverse direction also met with resistance. Reverse cannulation was not attempted in other patients. Spontaneous extrusion of the suture into the anterior chamber during cannulation occurred in two patients with narrow anterior chamber angle. This occurred at the site of peripheral anterior synechiae with a 5-0 Prolene suture in one patient. Another patient did not have any goniosynechiae and a 6-0 Prolene® suture was used.
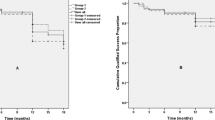
Patients were followed up for a mean period of 45.0 ± 14.6weeks (range 6 weeks – 2 years). The mean IOP 6 weeks after surgery was 13.3 ± 3.3 mm Hg and the mean IOP at 1 year was 13.5 ± 2.6 mm Hg. Mean drop in IOP was 11.3 ± 9.1 mm Hg (percentage drop 39%) at six weeks and 13.9 ± 9.6 mm Hg (percentage drop 40.9%) at one year. The overall success was 93.5%(n = 32), 90%(n = 30) and 96.3% (n = 27) respectively at 3 months, 6 months and 1 year after surgery. The absolute success rate was 80.7%, 80%, and 92.6 % at 3months, 6 months and 1 year respectively. The mean number of medications prior to surgery was 2.1 ± 1.0 and this reduced to 0.15 ± 0.3 at 6 months. The difference in success rates between patients who underwent <180° of GATT and >180° of GATT was not statistically significant. The IOP at different time intervals is given in Supplementary Fig. 1. The Kaplan Meier survival analysis is given in Supplementary Fig. 2.
At three months, the trabecular shelf seen was less than the degrees of cannulation done in nine patients (28.1%). The mean post op trabecular shelf seen on gonioscopy was 214.4 ± 91.3°. In two patients (5.9%), only 90° of trabecular shelf was seen, though 360° cannulation had been achieved. In the remaining 270°, slight pigmentation was seen and no shelf could be appreciated. An example is shown in Supplementary Fig. 3. The success rates were not significantly different between those who had <180° shelf remaining and those who had ->180° shelf remaining or between those who had an intact trabecular shelf (for the entire length cannulated) vs. those who had lesser degrees of trabecular shelf. The data is summed up in Tables 2, 3 and 4.
Complications
Complications were noted in 6/34 eyes (17.6%). In one patient, blood was noted in the Schlemm’s canal. After incising the trabecular meshwork, severe bleeding resulted in media haze. And in another patient corneal stromal hydration resulted in media haze. Cannulation could be done only for 90° in these two patients.3 patients(8.8%) were noted to have a hyphema in the first week. One patient had a total hyphema (2.9%)and needed an anterior chamber wash. This patient was not on anticoagulants or blood thinners. One patient (2.9%) had a localized Descemet’s membrane detachment, while retrieving the distal end of the Prolene® suture. The Descemet’s membrane was attached back by air bubble injection into the anterior chamber on the first postoperative day. Another patient had high IOP and shallow anterior chamber due to migration of air bubble behind the pupil causing pupillary block. Air bubble release was done in the operating room under surgical asepsis.
Three patients (8.8%) had multiple peripheral anterior synechiae of which 2 patients had IOP < 18 mm hg at all visits and the third patient needed two anti-glaucoma medications for IOP control. One patient(2.9%) had heavy pigment deposition on the IOL and was advised Nd:Yag pigmentolysis.
Discussion
A summary of published literature on GATT is presented in Table 5. It is generally held that 360° circumferential trabeculotomy yields a higher success rate than partial trabeculotomy. Grover et al. [2] initially reported successful 360° cannulation with the use of a fibre optic micro-catheter/suture (suture was used in <10% of patients). He did mention that some cannulations met with an obstruction between 180 and 270°. This was managed by reverse cannulation—the exact number was not specified. In patients with prior incisional surgery, the Grover et al. [3] mentioned that >270° cannulation was achieved with the use of an illuminated micro-catheter or suture. The authors mentioned resistance and extrusion at the site of trabeculectomy ostium/tube entry site. In another paper, Grover et al. [5] mentioned that 4.5% of patients had between 180 and 280° treated with GATT in a series of 198 patients. Reverse cannulation to counter any obstruction to passage of the micro-catheter was also reported by Kamran et al. [7], but the exact proportion of patients who had this problem was not specified. In four (of 66 patients) further passage was not possible and this was attributed to scarring of the trabecular meshwork probably caused by cataract surgery. The outcome in these patients was not substantially different.
Baykara et al. [8] reported 360° cannulation in 20/32 patients with the use of a 6-0 Prolene® suture. The remaining patients had >180° cannulation. The exact difficulty encountered was not reported. The authors did not attempt reverse cannulation and difference in success rates between the two groups was not analysed. The IOP dropped by65.9 ± 10.7% at the 6th month review. Keeping the above studies [2,3,4,5, 7] and our results in perspective, it is evident that 360° trabeculotomy may not be possible in all patients. A lesser degree of cannulation may still be successful. Hirabayashi et al. [9] reported that 90–120° of excisional goniotomy with the Kahook Dual Blade® was at least as successful as 360° GATT. In cadaveric eyes, it has been shown that there is a 30% reduction in outflow resistance with 30° trabeculotomy compared to 71% reduction when 360° of the angle was treated. [10] Baoet al. [11] reported that 120° trabeculotomy was successful in lowering intraocular pressure, though the results were inferior to conventional trabeculectomy in terms of IOP reduction and progression of visual field damage. Hirabayeshi et al. [9] reported that a full 360° cannulation may not be necessary to attain maximal efficacy as they postulated a dose–response threshold effect such that trabecular meshwork incision/excision beyond 120° provides no additional aqueous humour outflow or IOP reduction. This seems plausible as success rates in our study did not differ significantly between patients who had <180° of cannulation vs. those who had >180° of cannulation. The number of patients in our study was small and the aforementioned results need confirmation in a larger series of patients.
Many studies report good one year success rates with GATT [2,3,4,5, 7, 12,13,14,15]. Our overall success rate of 96.3% at one year must however be interpreted with caution as one year data was available only for 27 out of 34 study eyes. Also, most of the patients in our series had mild/moderate glaucoma. Grover et al. [5] has suggested that the success rate may be lower in patients with advanced glaucoma and attributed it to a greater degree of collector channel atrophy.
Adding a “marker suture” helps the surgeon identify the approximate the distance traversed by the Prolene® suture and choose an approximate site for goniotomy should the progress stop. An indirect gonioscope may also be used to locate the suture tip (without having to manipulate patient head or the microscope), but the suture may be difficult to view in a heavily pigmented trabecular meshwork. Cutting the suture to appropriate length was another alternative, but we were apprehensive that we would be left with insufficient suture length.
One patient (2.9%) in our study had severe bleeding into the anterior chamber needing a surgical wash. Severe bleeding postoperatively has been reported only in patients on anti-coagulants by Grover et al. study [2]. Yalinbas [16] reported intra-capsular haematoma needing a secondary intervention (surgical wash/YAG) in two patients. These patients were not on anticoagulants or blood thinners. Other reported complications of GATT include detachment of Descemet’s membrane, corneal oedema, iridodialysis, and cystoid macular edema [2,3,4,5, 7]. None of our patients had a loss of best corrected visual acuity.
We noted that the trabecular shelf partially disappeared and was replaced by a lightly pigmented area in the region of the trabecular meshwork. An example is shown in Supplementary Fig. 3. This did not seem to have a bearing on the short term success rates (Tables 2–4). Grover et al. [5] mentioned that the trabecular shelf may get partially obscured during subsequent reviews, but did not comment on the clinical impact of this finding. Other studies have not reported on the gonioscopy findings during reviews.
Most authors performed GATT prior to cataract extraction and suggested that this may help flush Schlemm’s canal and collector channels thereby improving success [2,3,4,5, 7, 8]. We feel that performing cataract surgery prior to GATT deepens the anterior chamber and enables a better view of the angle. We washed the anterior chamber at the conclusion of surgery (to remove blood, excess viscoelastic in the anterior chamber and viscoelastic behind the IOL) and this may yield a similar benefit. Spontaneous extrusion of the suture tip into the anterior chamber has not been reported in other studies. We noted this during surgery in two of our patients. While one of these patients had peripheral anterior synechiae that may have caused this, the reason for extrusion in the other patient is not clear.
The limitations of our study include its retrospective nature, small number of patients and limited follow-up. We included six patients with appositional angle closure. It is possible therefore that some IOP reduction may have been obtained by widening of the anterior chamber angle after cataract surgery. Pandav et al [17] reported a median IOP reduction of 19.1% in primary angle closure suspects after cataract surgery alone but there was a wide variation (± 18.0%) in the IOP drop. It is difficult to separate the benefits of GATT vs Cataract surgery in the six primary angle closure suspects in our series. Adding a “marker suture” may help surgeons and their assistants identify the approximate length of Schlemm’s canal cannulated. Obstruction of the suture in the Schlemm’s canal may be more frequent than previously thought. The long-term impact of partial trabeculotomy in adult patients with glaucoma and the relative role of GATT in primary angle closure suspects need to be studied in a larger series of patients with longer follow-ups.
Summary
What was known before
-
360° of GATT successfully lowers IOP in patients with open angle glaucoma.
-
The use of a fibre optic light pipe helps locate the position of the tip and obstruction to cannulation.
-
Severe hyphema can occur postoperatively in patients who are on blood thinners.
-
Partial closure of the trabecular shelf can occur.
What this study adds
-
360° cannulation may not always be feasible because of obstruction/extrusion of suture into the anterior chamber. Partial cannulation may still be successful in lowering IOP. GATT after phacoemulsification permits a better view of the angle. A “marker suture” may be added to estimate the distance cannulated.
-
Postoperative gonioscopy shows obscuration of the trabecular shelf in some patients. This does not seem to impact success rates in the short term.
-
Peripheral anterior synechiae may occur despite the use of postoperative pilocarpine.
References
Grant WM. Further studies on facility of flow through the trabecular meshwork AMA Arch Ophthalmol. 1958;60:523–33.
Grover DS, Godfrey DG, Smith O, Feuer WJ, Montes de Oca I, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy, Ab interno trabeculotomy technique report and preliminary results. Ophthalmology. 2014;121:855–61.
Grover DS, Godfrey DG, Smith O, et al. Outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in eyes with prior incisional glaucoma surgery. J Glaucoma. 2017;26:41–45.
Grover DS, Fellman RL. Gonioscopy-assisted transluminal trabeculotomy (GATT): thermal suture modification with a dye-stained rounded tip. J Glaucoma. 2016;25:501–4.
Grover DS, Smith O, Fellman RL, Godfrey DG, Gupta A, Montes de Oca I, et al. Gonioscopy-assisted transluminal trabeculotomy: an ab interno circumferential trabeculotomy 24 months follow-up. J Glaucoma. 2018;27:393–401.
Hodapp E, Parrish RK II, Anderson DR (eds). Clinical decisions in glaucoma. 1st edition (St. Louis: The CV Mosby Co. 1993) 52–61.
Rahmatnejad K, Pruzan NL, Amanullah S, Shaukat BA, Resende AF, Waisbourd M, et al. Surgical outcomes of gonioscopy-assisted transluminal trabeculotomy in patients with open angle glaucoma. J Glaucoma. 2017;26:1137–1143.
Baykara M, Poroy C, Erseven C. Surgical outcomes of combined gonioscopy ‑ assisted transluminal trabeculotomy and cataract surgery. Indian J Ophthalmol. 2019;67:505–8.
Hirabayashi LeeD, King JT, Thomsen S, An JA. Comparison of surgical outcomes of 360 ° circumferential trabeculotomy versus sectoral excisional goniotomy with the kahook dual blade at 6 months. clinical. Ophthalmology. 2019;13:2017–24.
Rosenquist R, Epstein D, Melamed S, Johnson M. Outflow resistance of enucleated human eyes at two different perfusion pressures and different extents of trabeculotomy. Curr Eye Res. 1989;8:1233–40.
Bao W, Kawase K, Huang H, Sawada A, Yamamoto T. The long-term outcome of trabeculotomy: comparison with filtering surgery in Japan. BMC Ophthalmol. 2019;19:1–8.
Guo CY, Qi XH, Qi JM. Systematic review and Meta-analysis of treating open angle glaucoma with gonioscopy-assisted transluminal trabeculotomy. Int J Ophthalmol. 2020;13:317–24.
Grover DS, Smith O, Fellman RL, Godfrey DG, Butler MR, Montes de Oca I, et al. Gonioscopy assisted transluminal trabeculotomy: an ab interno circumferential trabeculotomy for the treatment of primary congenital glaucoma and juvenile open angle glaucoma. Br J Ophthalmol. 2015;99:1092–1096.
Sato T, Hirata A, Mizoguchi T. Prospective, noncomparative, nonrandomized case study of short-term outcomes of 360° suture trabeculotomy ab interno in patients with open-angle glaucoma. Clin Ophthalmol. 2015;9:63–68.
Smith BL, Ellyson AC, Kim WI Trabectome-initiated gonioscopy-assisted transluminal trabeculotomy. Mil Med. 2018;183 (Suppl 1), 146–9.
Yalinbas Duygu, Aktas Zeynep, Hepsen Ibrahim, An NilayDilekmen. unusual complication of combined gonioscopy-assisted transluminal trabeculotomy and phacoemulsification: vision loss due to intracapsular hematoma. Int Ophthalmol. 2018;38:2223–6.
Pandav SS, Seth NG, Arora A, Thattaruthody F, Jurangal A, Kaushik S, et al. Intraocular pressure reduction in a spectrum of angle closure disease following cataract extraction. Indian J Ophthalmol. 2019;67:1433–8.
Acknowledgements
We thank statisticians from beyond p value for the statistical analysis. Dr. Craig J Chaya supported in part by an Unrestricted Grant from Research to Prevent Blindness, Inc., New York, NY, to the Department of Ophthalmology & Visual Sciences, University of Utah. This study has not been funded by anyone.
Author information
Authors and Affiliations
Contributions
FA was responsible extracting and analysing data, interpreting results, updating reference lists and creating “Summary of findings” tables. MR contributed to interpreting results, designing the review protocol, screening potentially eligible studies, extracting and analysing data, interpreting results and writing the report. CR was responsible for data extraction, designing the review protocol and providing feedback on the report. CJC helped interpret the results, design the study protocol and provided feedback on the report. VM contributed to extracting and analysing data and interpreting results.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Asafali, F., Rajamani, M., Ramamurthy, C. et al. Relationship of degrees of gonioscopy assisted transluminal trabeculotomy and trabecular shelf to success using a marker suture technique. Eye 37, 132–138 (2023). https://doi.org/10.1038/s41433-021-01838-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01838-x