Abstract
A significant proportion of the astronauts who spend extended periods in microgravity develop ophthalmic abnormalities including optic disc edema, globe flattening, chorioretinal folds, and hyperopic refractive error shifts. A constellation of these neuro-ophthalmic findings has been termed “spaceflight-associated neuro-ocular syndrome”. Understanding this syndrome is currently a top priority for NASA, especially in view of future long-duration missions (e.g., Mars missions). The recent discovery of an “ocular glymphatic system” can potentially help to unlock mechanisms underlying microgravity-induced optic disc edema. Indeed, a major paradigm shift is currently occurring in our understanding of transport of fluids and solutes through the optic nerve following the recent discovery of an optic nerve glymphatic pathway for influx of cerebrospinal fluid. In addition, the recent identification of an entirely new glymphatic pathway for efflux of ocular fluid may have profound implications for fluid dynamics in the eye. Observations pertaining to this ocular glymphatic pathway provide critical new insights into how intracranial pressure can alter basic fluid transport in the eye. We believe that these novel findings have the potential to be game changers in our understanding of the pathogenesis of optic disc edema in astronauts. In the present review, we integrate these new insights with findings on the intracranial and neuro-ophthalmologic effects of microgravity in one coherent conceptual framework. Further studies in this area of investigation could not only provide exciting new insights into the mechanisms underlying microgravity-induced optic disc edema but also offer opportunities to develop countermeasure strategies.
摘要
在长时间处于微重力状态的宇航员中, 大部分人会出现视力异常, 包括视盘水肿、眼球扁平、脉膜视网膜皱褶和远视屈光不正。这些神经眼科的发现被称为“太空飞行相关神经眼综合征”。了解这一综合征目前是美国宇航局的首要任务, 特别是考虑到未来的长期任务 (如火星任务等) 。最近发现的“眼淋巴系统”可能有助于解开微重力引起视盘水肿的潜在机制。事实上, 随着最近发现了视神经-淋巴通道, 我们对液体和溶质通过视神经传输的理解正在发生重大的范式转变。此外, 最近发现了一种全新的眼内液体流出的淋巴途径可能对眼液动力学有深远的影响。针对眼部淋巴通路的观察为颅内压如何改变眼内基本液体运输提供了重要的新见解。我们相信, 这些新发现有可能改变我们对宇航员视盘水肿发病机制的理解。在目前的综述中, 我们将这些新的见解与微重力对颅内和神经眼科影响的研究结果整合在一个续贯的概念框架中。该领域的后续研究不仅可以为微重力诱导视盘水肿的机制提供令人兴奋的新见解, 而且也为制定相应的对策提供了机会。
Similar content being viewed by others
Introduction
Although ophthalmic changes have been described in some astronauts since the early years of human spaceflight in the 1960s, these changes were thought to be transient or minor, having little impact on the space crew [1]. However, missions to the International Space Station (ISS) have highlighted concern over potentially harmful neuro-ocular changes for crew members who spend prolonged time in microgravity [1]. It has been reported that a significant proportion of the astronauts who have flown on long-duration missions (~6 months) aboard the ISS are experiencing ophthalmic abnormalities collectively referred to as “spaceflight-associated neuro-ocular syndrome” (SANS), some of which appear to persist after return to Earth [1,2,3,4,5]. SANS is currently defined as having one or more of the following new findings during or immediately after spaceflight: clinically significant optic disc edema (ODE) (Fig. 1); retinal and choroidal folds (Fig. 1); globe flattening; and hyperopic refractive error shifts (approved by the NASA JSC Human System Risk Board, Houston, Texas). These neuro-ocular changes may be associated with varying degrees of symmetrical and asymmetrical optic nerve sheath distension [2]. The earliest signs of SANS are detected in roughly 70% of astronauts during or following long-duration spaceflight. Clinically significant ODE has been diagnosed during or after long-duration spaceflight in ~16–19% of astronauts as determined by fundoscopy or as measured by increased peripapillary total retinal thickness on optical coherence tomography (OCT) [6]. Currently, the exact mechanisms causing SANS are not fully understood [3, 4]. As the United States prepares for even longer duration spaceflight missions, including continued trips to the ISS, a return to the moon, or a future human mission to Mars, the National Aeronautics and Space Administration (NASA) has made it a high priority to understand SANS and to develop countermeasure strategies [3, 4].
Figure reproduced from [5] with permission.
A major paradigm shift is currently occurring in our understanding of transport of fluids and solutes through the optic nerve following the recent discovery of an optic nerve glymphatic cerebrospinal fluid (CSF) transport system [7, 8]. Additionally, the recent identification of an entirely new glymphatic pathway for efflux of ocular fluid may have profound implications for fluid dynamics in the eye [8, 9]. Although both above studies [7, 8] were performed in rodents, we believe that these novel findings have the potential to be game changers in our understanding of the pathogenesis of ODE in astronauts. In the present review, we integrate these new insights with findings on the intracranial and neuro-ophthalmologic effects of microgravity in one coherent conceptual framework.
Discussion
Potential mechanisms underlying SANS-associated optic disc edema
Elevated intracranial pressure
SANS was initially called “visual impairment and intracranial pressure syndrome” as it was thought to be caused by elevated intracranial pressure (ICP) resulting from weightlessness-induced cephalad fluid shifts leading to venous stasis in the head and neck [2]. This stasis could cause cerebral venous congestion and impairment of CSF drainage into the venous system, both of which could lead to a rise in ICP [2]. This increased cerebral subarachnoid CSF pressure could be transmitted directly from the intracranial compartment to the intraorbital compartment through the perioptic subarachnoid space (SAS) [2]. The elevated CSF pressure at eye level could then result in optic nerve sheath distension and anteriorly directed forces that indent the posterior sclera resulting in posterior globe flattening [2]. In addition, this elevated CSF pressure within the optic nerve sheath could result in optic nerve compression and stasis of axoplasmic flow with resultant ODE similar to what occurs in patients with terrestrial idiopathic intracranial hypertension (IIH) [10].
However, it should be noted that the role of high ICP in astronauts is now being challenged and it remains unclear whether SANS-associated ODE represents true papilledema (i.e., ODE due to increased ICP) [3, 4]. Postmission lumbar puncture opening pressures measured thus far were only mildly elevated [3, 4]. Furthermore, although some similarities between SANS and terrestrial IIH were noted, astronauts did not report typical symptoms of increased ICP commonly seen in patients with IIH, such as chronic headache, pulsatile tinnitus, or diplopia [3, 4]. This lack of findings commonly associated with IIH suggests that increased ICP might not be the sole or even primary cause of ODE in astronauts and that other mechanisms should be considered [3, 4]. Recent data from parabolic flights (acute zero gravity) provided further evidence against the hypothesis that ICP is pathologically elevated in 0 g [11]. In fact, the transient removal of gravity during parabolic flight reduced the ICP compared to the supine posture [11]. However, ICP was not reduced to the levels observed in the 90 deg seated upright posture on Earth [11]. These findings suggested that the absence of diurnal, postural reductions in ICP relative to intraocular pressure (IOP) in microgravity creates a persistently lower pressure gradient at the posterior aspect of the eye, which may explain remodeling of the eye in astronauts [11]. It should be noted, however, that these measurements during parabolic flights are for brief periods of zero gravity and that considerable caution is warranted in extrapolating these findings to long-duration spaceflight. Further studies are needed to determine whether short-term measurements during parabolic flights reflect long-term measurements in space.
Optic nerve compartment syndrome
SANS-related compartmentalization of CSF in the orbital SAS with locally elevated optic nerve sheath pressures has been proposed as an additional alternate mechanism for explaining ODE in astronauts [2,3,4]. The SAS surrounding the optic nerve is a septated, tightly confined, trabeculated, blind-ending (cul-de-sac) space, which is in communication with the intracranial SAS in a normal terrestrial population [10, 12]. The arachnoid and the pia mater, as well as the arachnoid trabeculae and septa traversing the SAS, are lined with meningothelial cells (MECs) [13]. The cul-de-sac anatomy of the confined perioptic SAS, which is further constricted through numerous trabeculae and septa, coupled with the cephalad fluid shifts of prolonged microgravity, may result in a fragile flow equilibrium that may lead to the sequestration of CSF within the orbital SAS with locally elevated optic nerve sheath pressures [10]. Unlike on Earth, where changing from supine to an upright posture reduces intracranial CSF volume due to a shift of CSF from the cranium to the spinal canal, in space, there is no force that intermittently reduces the cranial CSF volume and, thereby, allows reversed movement of CSF from the orbit back into the cranium [14]. Therefore, during long-duration spaceflight, it is highly unlikely that the CSF, once in the orbital CSF space, can change its direction of flow from the SAS of the optic nerve toward the intracranial SAS [2]. In addition, the arrangement of trabeculae and septa in the SAS of the optic nerve offers the possibility that a one-way valve-like mechanism may cause local CSF entrapment within the SAS of the optic nerve [15], given that it may still allow unidirectional CSF inflow while further preventing outflow.
Furthermore, it is possible that MECs may also play a role in further narrowing the SAS of the optic nerve. Indeed, MECs have been shown to react with swelling and cellular proliferation to biological and mechanical stimuli such as elevated pressure [13, 16]. A marked swelling of MECs of the arachnoid as well as the trabeculae and septa in the SAS of the optic nerve has been documented following experimental compartmentalization in sheep [16]. Such swelling and proliferation of MECs may further narrow the SAS surrounding the optic nerve, eventually leading to obstruction of CSF influx [13].
A CSF outflow pathway from the SAS of the optic nerve is therefore of critical importance to prevent CSF accumulation and pressure build-up in this small anatomical compartment that ends blindly behind the globe [15]. The mechanism by which CSF is reabsorbed out of the SAS of the optic nerve is not fully understood [17]. In addition to arachnoid villi in the meninges of the optic nerve [18], lymphatics in the dura mater of the human optic nerve have been proposed as another possible outflow pathway for CSF from the optic nerve SAS [17, 19]. However, these orbital optic nerve venous and lymphatic drainage systems may be affected by microgravity-induced cephalad fluid shifts, further impeding CSF outflow and producing increased optic nerve sheath pressures [2].
The end result of either mechanism, increased ICP or sequestration of CSF within the SAS of the optic nerve, is a rise in CSF pressure within the SAS surrounding the optic nerve that may influence the trans-lamina cribrosa pressure difference (TLCPD). The TLCPD is defined as the difference between IOP minus optic nerve SAS pressure.
Ocular glymphatic flow imbalance mechanism
Retrograde glymphatic CSF influx
A more novel mechanism proposed by our group [20,21,22,23,24,25] for microgravity-induced ODE pertains to the “ocular glymphatic system” concept. We proposed that ODE in astronauts may result, at least partly, from a glymphatic flow imbalance mechanism at the optic nerve head [20,21,22,23,24,25]. In 2012, the “glymphatic system” was first described in mice by a team of researchers headed by Iliff and Nedergaard [26]. Their findings suggested a brain-wide network of perivascular pathways along which a large proportion of subarachnoid CSF recirculates through the brain parenchyma, facilitating the clearance of interstitial solutes, including amyloid-β (Aβ), from the brain [26]. CSF enters the brain along periarterial channels to exchange with interstitial fluid, which is in turn cleared from the brain along perivenous pathways for ultimate clearance via cervical lymphatic vessels (Fig. 2) [9, 26]. From the SAS, CSF is driven into the Virchow-Robin spaces by a combination of arterial pulsatility, respiration, slow vasomotion, and CSF pressure gradients [27, 28]. The subsequent transport of CSF into the dense and complex brain parenchyma is facilitated by aquaporin-4 (AQP4) water channels which are expressed in a highly polarized manner in astrocytic endfeet ensheathing the cerebral vasculature [27].
ICP intracranial pressure, IOP intraocular pressure. Figure reproduced and modified from [9].
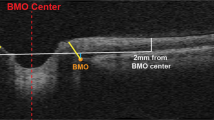
In 2015, Wostyn et al. [29] published a hypothesis-driven report, providing key arguments for the necessity of a glymphatic system in the optic nerve. The authors further provided the first histologic evidence to support the existence of a perivascular pathway within the human optic nerve following post-mortem administration of India ink into the SAS of the optic nerve [30, 31]. Intriguingly, more recent studies have further provided evidence for CSF entry into the optic nerve via a glymphatic pathway [7, 8, 32, 33]. After fluorescent tracer injection into the CSF of live mice, Mathieu et al. [7] found CSF entry into the optic nerve along small perforating pial vessels in a size-dependent manner through sleeve-like paravascular spaces between vessel walls and AQP4-positive astrocytic endfeet. Very recently, Wang et al. [8] confirmed and extended these findings by showing that CSF tracer influx occurs along the periarterial and pericapillary spaces in the optic nerve in mice. Jacobsen et al. [33] recently performed a magnetic resonance imaging (MRI) study of human visual pathway structures following intrathecal administration of gadobutrol serving as a CSF tracer. CSF tracer enrichment was found within the optic nerve, optic chiasm, optic tract, and primary visual cortex. In the vitreous body, only a nonsignificant signal increase was evident [33]. Based on their observations, the authors hypothesized the existence of a glymphatic system in the human visual pathway. Interestingly, substantial gadobutrol enrichment was seen in the retrobulbar part of the optic nerve, as compared to the middle and posterior sections, corresponding to the entrance of the central retinal artery [33]. As noted by the authors, analogous to the main entry routes of CSF tracer molecules into the human brain parenchyma along large artery trunks at the brain surface, this area could function as a major periarterial route facilitating the entry of gadobutrol from the SAS into the optic nerve interstitium.
In line with the above findings, we had previously proposed that ODE in astronauts may result, at least partly, from the forcing of perioptic CSF into the optic nerve and prelaminar optic nerve head along perivascular spaces surrounding the central retinal artery, related to long-standing microgravity fluid shifts and variations in optic nerve sheath anatomy and compliance [20, 21, 24, 25]. Such a CSF-related mechanism may be especially relevant under conditions of prolonged microgravity, where the fluids of the body, including CSF, redistribute cranially, and where CSF outflow routes (venous and lymphatic) from the SAS of the optic nerve may be affected by headward fluid shifts [20]. In this scenario, CSF may be pushed from the SAS of the optic nerve to the perivascular glymphatic pathway within the optic nerve, and further infiltrate into the optic disc [20].
As noted above, simulated microgravity parabolic flight studies have shown that near complete removal of gravitational gradients does not pathologically elevate ICP but does prevent the normal lowering of ICP when standing [11]. In space, the influence of gravity is removed and ICP may fall to an equilibrium point between the upright and supine postures on Earth, assuming short-term measurements during parabolic flight reflect long-term measurements in space [11]. Although ICP does not appear to be pathologically elevated in space, over 24 h, pressure in the brain may be consistently above that observed on Earth [11]. We believe that this could enhance CSF entry into the optic nerve SAS and perivascular spaces. This possibility is supported by the findings in a dog study by Hou et al. [34] showing that the optic canal apparently creates a certain optic canal resistance, and that a minimal ICP is required for the CSF to freely flow through the optic canal. Therefore, over 24 h in microgravity, CSF flow into the perioptic CSF compartment may increase above that on Earth, forcing entry of CSF into the optic nerve.
If CSF would indeed be forced into the optic nerve along the central retinal artery under prolonged microgravity conditions, it would be interesting to investigate whether CSF then can further infiltrate into the optic disc. Of particular interest here is the recent CSF flow study by Mathieu et al. [7]. Following tracer injection into the CSF of normal mice, Mathieu et al. [7] found paravascular CSF entry into the optic nerve up to and including the glial lamina, the mouse equivalent of the human lamina cribrosa. Entry of CSF tracers into the optic nerve head beyond the level of the glial lamina was not observed. A possible explanation for absence of paravascular CSF tracers beyond the lamina could be the presence of a natural occlusion of the paravascular spaces [35]. An additional explanation could be the presence of a functional barrier created at the interface of two opposing sources of pressure [35]. The higher IOP might counteract further fluid movement into the eye along paravascular spaces [35]. Thus, the results of the study by Mathieu et al. [7] do not support the notion of free movement of CSF and constituent cells or solutes along paravascular pathways into the eye under conditions of normal ICP. This does not, however, negate the possibility that elevation of optic nerve sheath pressure, due to a rise in ICP and/or sequestration of CSF within the orbital SAS, may force CSF contents along paravascular pathways into the eye [35]. Although Mathieu et al. [7] did not investigate what happens under conditions of elevated ICP, it is possible that a reversal in the TLCPD may lead to CSF permeating along paravascular spaces into the prelaminar optic nerve, further causing ODE. Further clarification of this issue could be achieved by evaluating whether tracers delivered to the CSF of animals move along paravascular spaces into the eye or at least through the lamina cribrosa under conditions of increased ICP, in the prolonged microgravity environment of space or in animal microgravity ground-based models. In this regard, it should be noted that, due to differences in optic nerve vascular anatomy, a mouse model may be less useful, given that in mice the central retinal artery enters the optic nerve at the level of the sclera and bypasses the SAS (and thus the CSF) [35, 36].
Anterograde ocular glymphatic transport blockage
In addition to the supposed retrograde CSF influx into the optic disc, we further hypothesized that the glymphatic outflow from the eye into the optic nerve might be impeded under prolonged microgravity conditions, leading to fluid stasis within the prelaminar optic nerve head, further causing ODE [21,22,23,24]. Under normal physiological conditions, the TLCPD is directed posteriorly across the lamina cribrosa. We speculated that under microgravity conditions, elevation of optic nerve sheath pressure, due to a rise in ICP and/or sequestration of CSF within the orbital SAS, may lead to a reduction or reversal of the normal posteriorly directed TLCPD, which in turn may block the glymphatic efflux of ocular fluid into the optic nerve, leading to fluid stasis within the prelaminar optic nerve head [22, 24]. Importantly, new research now provides indirect experimental evidence in support of this hypothesis. Indeed, the new study by Nedergaard and colleagues [8] identified a novel ocular glymphatic pathway for removal of fluid and metabolites from the intraocular space in rodents (Fig. 2). The authors found that Aβ was cleared from the retina and vitreous via a pathway dependent on glial water channel AQP4. After traversing the lamina barrier, intra-axonal Aβ was cleared via the perivenous space and subsequently drained to lymphatic vessels. To define the role of the TLCPD in transport of Aβ tracer, the researchers manipulated ICP by either withdrawal or infusion of artificial CSF in the cisterna magna while monitoring ICP. Decreasing ICP was linked to a sharp increase in the total Aβ tracer signal and peak intensity of Aβ tracer transport in the proximal optic nerve 30 min after intravitreal injection. Conversely, increasing ICP was associated with a lack of Aβ tracer in the proximal segment of the optic nerve. The findings did not support that the tracer signal was diluted as a consequence of increased CSF inflow along the periarterial spaces due to CSF infusion, but instead reflected a decreased ocular Aβ tracer clearance into the optic nerve. These data showed that the TLCPD is a major driver of ocular glymphatic outflow [8]. Very interestingly, these data also suggest that a rise in orbital CSF pressure, assumed to occur in microgravity, would directly inhibit this ocular glymphatic outflow [8]. This lends support to the hypothesis, originally proposed by our group [21,22,23,24], that anterograde ocular glymphatic transport blockage may play a role in the development of microgravity-induced ODE.
Interestingly, the recent discovery of an “ocular glymphatic system” may also provide clues to mechanisms behind the reported delay in the recovery of SANS-associated ODE. In a recent OCT study, Macias et al. [37] quantitated ocular structural changes, including peripapillary retinal thickness, that develop in association with long-duration spaceflight and documented how long these changes persist after landing. They found that long-duration spaceflight was associated with ODE and that between 30 and 90 days were required for the peripapillary retinal tissue thickening to return to values similar to those observed before flight. Macias et al. [37] further noted that the lack of a retinal-blood barrier in the prelaminar region of the optic nerve head may be associated with a greater extravasation of fluid due to the headward fluid shift in weightlessness and may be a contributing factor to the retinal thickening quantified at this location. As discussed above, observations pertaining to the recent discovery of an “ocular glymphatic clearance system” provide critical new insights into how increased ICP, and thus a rise in orbital CSF pressure which is assumed to occur in microgravity, can alter basic fluid transport in the eye. These observations, in combination with an increased capillary filtration as proposed by Macias et al. [37], might contribute to the ODE seen in astronauts [22]. Also interestingly, Nedergaard and colleagues [9] noted that the amount of fluid that exits the eye via the posterior ocular glymphatic clearance route is likely to be orders of magnitude lower than clearance via anteriorly located routes. We propose that this could provide one possible explanation for the slow postflight recovery of astronauts from ODE.
Preflight identification of astronauts at risk for developing microgravity-induced optic disc edema
It seems worthwhile to make every effort to identify biomarkers for prediction of SANS-associated ODE, especially given that this medical obstacle could impact the visual health of astronauts during long-duration spaceflight and could interfere with plans for future missions, including trips to Mars. It has been suggested that microgravity-induced ocular changes may be partially determined by the elastic properties of the brain ventricles and optic nerve sheath [21, 38, 39].
Wostyn and De Deyn [21, 39] hypothesized that a greater compliance and elasticity of the optic nerve sheath may result in a larger compensatory reserve capacity in the SAS surrounding the optic nerve, which in turn may protect against signs and symptoms of SANS. The authors speculated that astronauts with less compliant optic nerve sheaths may be more likely to develop ODE, given that a greater degree of optic nerve sheath rigidity that prevents further expansion may result in more CSF pressure build-up in the retroorbital space [21, 39]. As such, optic nerve sheath stiffness might serve as a predictive biomarker for ODE in astronauts.
The view that a larger compensatory reserve capacity in the CSF compartment may protect against SANS is consistent with the smaller change in the percentage of total ventricular volume experienced by astronauts with SANS, as observed in a recent study by Roberts et al. [40]. The authors retrospectively analyzed brain MRI scans of NASA astronauts to quantify pre- to postflight changes in brain structure [40]. Long-duration spaceflights aboard the ISS, but not short-duration Space Shuttle flights, resulted in a significant increase in the percentage of total ventricular volume change (10.7% versus 0%, P < 0.001, n = 12 versus n = 7). The authors also examined post hoc the extent to which pre- to postflight structural brain changes were associated with the development of SANS. Of the 12 long-duration astronauts, the 4 astronauts with ophthalmologic changes had a smaller change in the percentage of total ventricular volume than those without SANS (12.8% versus 6.5%, P = 0.02, n = 8 versus n = 4). This suggests that a reduced compensatory reserve capacity in CSF space, e.g., due to less compliant (stiffer) brain ventricles, may increase the astronaut’s likelihood of developing ophthalmic changes [41]. As such, it would be interesting to investigate the predictive value of MR elastography, as a non-invasive imaging measure of brain stiffness, for the development of ODE in astronauts [42]. If confirmed, identifying the individual brain stiffness in astronauts would be extremely important for predicting the risk of SANS-associated ODE, and for decision making regarding astronaut selection for future long-duration spaceflight missions beyond low Earth orbit.
It has also been questioned whether the optic canal acts as a buffer against the transmission of CSF pressure to the lamina cribrosa [43]. In a retrospective analysis with MRI, Bidot et al. [43] found that larger optic canals were associated with more severe papilledema and poor visual function in 69 patients with IIH. One possible explanation suggested by the authors was that narrower optic canals limit CSF flow into the perioptic CSF compartment, whereas larger optic canals facilitate the transmission of the CSF pressure to the lamina cribrosa resulting in worse papilledema [43]. Accordingly, they demonstrated using MRI that the optic canal was always larger on the side of the worst papilledema in a series of 8 patients with IIH and very asymmetric papilledema [44]. However, it should be noted that a recent study showed that bony optic canal size evaluated by orbital computed tomography scan was not different in very asymmetric papilledema in IIH patients [45]. Anyway, examination of the optic canal size in astronauts would be very informative and could lead to further elucidation of the possible mechanisms underlying SANS [46, 47]. If confirmed, the optic canal size could be used as a predictive biomarker for ODE in astronauts.
Conclusion
The recent discovery of an “ocular glymphatic clearance system” may have profound implications for understanding pathophysiological mechanisms underlying a wide range of ophthalmic diseases. In the present paper, by integrating new insights pertaining to the ocular glymphatic system concept with findings on the intracranial and neuro-ophthalmologic effects of microgravity, we provided a coherent conceptual framework for understanding the pathogenesis of microgravity-induced ODE. According to this hypothesis, ODE in astronauts may ultimately result from a glymphatic flow imbalance mechanism at the optic nerve head, related to long-standing microgravity fluid shifts, variations in optic nerve sheath anatomy and compliance, and the elastic properties of the brain ventricles. Obviously, further research is required to provide additional insight regarding the relative contribution of the ocular glymphatic system to ODE in astronauts. Even though nothing conclusive can yet be said, the recent report providing indirect experimental evidence in support of the glymphatic hypothesis of SANS-associated ODE is encouraging. Continued examination of all spaceflight crew members, including those without clinically apparent optic disc swelling, may provide additional insight regarding the relative contribution of an ocular glymphatic flow imbalance mechanism. Future pre-flight, in-flight and post-flight analysis of the optic nerve head and surrounding structures by OCT as well as ultrasound and MRI examination of the globe, optic nerves and optic nerve sheaths in long-duration ISS crew members could provide important structural information in this respect. Further studies in this area of investigation could not only provide exciting new insights into the mechanisms underlying microgravity-induced ODE but also offer opportunities to develop countermeasure strategies. We therefore wish to encourage further research in this area.
References
Nelson ES, Mulugeta L, Myers JG. Microgravity-induced fluid shift and ophthalmic changes. Life. 2014;4:621–65.
Mader TH, Gibson CR, Pass AF, Kramer LA, Lee AG, Fogarty J, et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology. 2011;118:2058–69.
Lee AG, Mader TH, Gibson CR, Tarver W. Space flight-associated neuro-ocular syndrome. JAMA Ophthalmol. 2017;135:992–4.
Lee AG, Mader TH, Gibson CR, Brunstetter TJ, Tarver WJ. Space flight-associated neuro-ocular syndrome (SANS). Eye. 2018;32:1164–7.
Mader TH, Gibson CR, Pass AF, Lee AG, Killer HE, Hansen HC, et al. Optic disc edema in an astronaut after repeat long-duration space flight. J Neuroophthalmol. 2013;33:249–55.
Stenger MB, Tarver WJ, Brunstetter T, Gibson CR, Laurie SS, Lee SMC, et al. NASA Human Research Program evidence report: human health countermeasures element: risk of spaceflight associated neuro-ocular syndrome (SANS). 2017.
Mathieu E, Gupta N, Ahari A, Zhou X, Hanna J, Yücel YH. Evidence for cerebrospinal fluid entry into the optic nerve via a glymphatic pathway. Invest Ophthalmol Vis Sci. 2017;58:4784–91.
Wang X, Lou N, Eberhardt A, Yang Y, Kusk P, Xu Q, et al. An ocular glymphatic clearance system removes β-amyloid from the rodent eye. Sci Transl Med. 2020;12:eaaw3210.
Rangroo Thrane V, Hynnekleiv L, Wang X, Thrane AS, Krohn J, Nedergaard M. Twists and turns of ocular glymphatic clearance – new study reveals surprising findings in glaucoma [letter]. Acta Ophthalmol. 2021;99:e283–e284.
Mader TH, Gibson CR, Otto CA, Sargsyan AE, Miller NR, Subramanian PS, et al. Persistent asymmetric optic disc swelling after long-duration space flight: implications for pathogenesis. J Neuroophthalmol. 2017;37:133–9.
Lawley JS, Petersen LG, Howden EJ, Sarma S, Cornwell WK, Zhang R, et al. Effect of gravity and microgravity on intracranial pressure. J Physiol. 2017;595:2115–27.
Killer HE, Jaggi GP, Flammer J, Miller NR, Huber AR, Mironov A. Cerebrospinal fluid dynamics between the intracranial and the subarachnoid space of the optic nerve. Is it always bidirectional?. Brain. 2007;130:514–20.
Xin X, Fan B, Flammer J, Miller NR, Jaggi GP, Killer HE, et al. Meningothelial cells react to elevated pressure and oxidative stress. PLoS One. 2011;6:e20142.
Alperin N, Bagci AM. Spaceflight-induced visual impairment and globe deformations in astronauts are linked to orbital cerebrospinal fluid volume increase. Acta Neurochir Suppl. 2018;126:215–9.
Killer HE, Jaggi GP, Flammer J, Miller NR, Huber AR. The optic nerve: a new window into cerebrospinal fluid composition? Brain. 2006;129:1027–30.
Jaggi GP, Harlev M, Ziegler U, Dotan S, Miller NR, Killer HE. Cerebrospinal fluid segregation optic neuropathy: an experimental model and a hypothesis. Br J Ophthalmol. 2010;94:1088–93.
Killer HE. Production and circulation of cerebrospinal fluid with respect to the subarachnoid space of the optic nerve. J Glaucoma. 2013;22:S8–S10.
Shanthaveerappa TR, Bourne GH. Arachnoid villi in the optic nerve of man and monkey. Exp Eye Res. 1964;3:31–35.
Killer HE, Laeng HR, Groscurth P. Lymphatic capillaries in the meninges of the human optic nerve. J Neuroophthalmol. 1999;19:222–8.
Wostyn P. “Houston, we have a problem”: “We are losing our eyesight”. Exp Eye Res. 2019;186:107725.
Wostyn P, De Deyn PP. Intracranial pressure-induced optic nerve sheath response as a predictive biomarker for optic disc edema in astronauts. Biomark Med. 2017;11:1003–8.
Wostyn P, De Winne F, Stern C, De Deyn PP. Dilated prelaminar paravascular spaces as a possible mechanism for optic disc edema in astronauts. Aerosp Med Hum Perform. 2018;89:1089–91.
Wostyn P, De Winne F, Stern C, Mader TH, Gibson CR, De Deyn PP. Potential involvement of the ocular glymphatic system in optic disc edema in astronauts. Aerosp Med Hum Perform. 2020;91:975–7.
Wostyn P, Killer HE, De Deyn PP. Why a one-way ticket to Mars may result in a one-way directional glymphatic flow to the eye. J Neuroophthalmol. 2017;37:462–3.
Wostyn P, Mader TH, Gibson CR, Killer HE. The escape of retrobulbar cerebrospinal fluid in the astronaut’s eye: mission impossible? Eye. 2019;33:1519–24.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147ra111.
Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The glymphatic system: a beginner’s guide. Neurochem Res. 2015;40:2583–99.
Iliff JJ, Wang M, Zeppenfeld DM, Venkataraman A, Plog BA, Liao Y, et al. Cerebral arterial pulsation drives paravascular CSF-interstitial fluid exchange in the murine brain. J Neurosci. 2013;33:18190–9.
Wostyn P, Van Dam D, Audenaert K, Killer HE, De Deyn PP, De Groot V. A new glaucoma hypothesis: a role of glymphatic system dysfunction. Fluids Barriers CNS. 2015;12:16.
Wostyn P, De Groot V, Van Dam D, Audenaert K, De Deyn PP, Killer HE. The glymphatic system: a new player in ocular diseases? Invest Ophthalmol Vis Sci. 2016;57:5426–7.
Wostyn P, Killer HE, De Deyn PP. Glymphatic stasis at the site of the lamina cribrosa as a potential mechanism underlying open-angle glaucoma. Clin Exp Ophthalmol. 2017;45:539–47.
Mathieu E, Gupta N, Paczka-Giorgi LA, Zhou X, Ahari A, Lani R, et al. Reduced cerebrospinal fluid inflow to the optic nerve in glaucoma. Invest Ophthalmol Vis Sci. 2018;59:5876–84.
Jacobsen HH, Ringstad G, Jørstad ØK, Moe MC, Sandell T, Eide PK. The human visual pathway communicates directly with the subarachnoid space. Invest Ophthalmol Vis Sci. 2019;60:2773–80.
Hou R, Zhang Z, Yang D, Wang H, Chen W, Li Z, et al. Intracranial pressure (ICP) and optic nerve subarachnoid space pressure (ONSP) correlation in the optic nerve chamber: the Beijing Intracranial and Intraocular Pressure (iCOP) study. Brain Res. 2016;1635:201–8.
Mathieu E. The relationship of ocular and cerebrospinal fluids to the optic nerve in health and glaucoma [dissertation]. Canada: University of Toronto;2018.
Albrecht May C. Comparative anatomy of the optic nerve head and inner retina in non-primate animal models used for glaucoma. Open Ophthalmol J. 2008;2:94–101.
Macias BR, Patel NB, Gibson CR, Samuels BC, Laurie SS, Otto C, et al. Association of long-duration spaceflight with anterior and posterior ocular structure changes in astronauts and their recovery. JAMA Ophthalmol. 2020;138:553–9.
Van Ombergen A, Jillings S, Jeurissen B, Tomilovskaya E, Rumshiskaya A, Litvinova L, et al. Brain ventricular volume changes induced by long-duration spaceflight. Proc Natl Acad Sci USA. 2019;116:10531–6.
Wostyn P, De Deyn PP. Optic nerve sheath distention as a protective mechanism against the visual impairment and intracranial pressure syndrome in astronauts. Invest Ophthalmol Vis Sci. 2017;58:4601–2.
Roberts DR, Asemani D, Nietert PJ, Eckert MA, Inglesby DC, Bloomberg JJ, et al. Prolonged microgravity affects human brain structure and function. AJNR Am J Neuroradiol. 2019;40:1878–85.
Wostyn P, Mader TH, Gibson CR, Wuyts FL, Van Ombergen A, Zu, Eulenburg P, et al. The possible role of elastic properties of the brain and optic nerve sheath in the development of spaceflight-associated neuro-ocular syndrome. AJNR Am J Neuroradiol. 2020;41:E14–E15.
Roberts DR, Asemani D, Nietert PJ, Eckert MA, Inglesby DC, Bloomberg JJ, et al. Reply. AJNR Am J Neuroradiol. 2020;41:E16.
Bidot S, Clough L, Saindane AM, Newman NJ, Biousse V, Bruce BB. The optic canal size is associated with the severity of papilledema and poor visual function in idiopathic intracranial hypertension. J Neuroophthalmol. 2016;36:120–5.
Bidot S, Bruce BB, Saindane AM, Newman NJ, Biousse V. Asymmetric papilledema in idiopathic intracranial hypertension. J Neuroophthalmol. 2015;35:31–36.
Farrokhi Y, Sharif Kashani S, Aghsaei Fard M, Pakdel F, Yadegari S. Optic canal size in idiopathic intracranial hypertension and asymmetric papilledema. Clin Neurol Neurosurg. 2019;184:105376.
Killer HE. Asymmetric papilledema in idiopathic intracranial hypertension: comment. J Neuroophthalmol. 2015;35:330–1.
Mader TH, Gibson CR, Hart SF, Lee AG. Asymmetric papilledema in idiopathic intracranial hypertension: comment. J Neuroophthalmol. 2016;36:111–2.
Author information
Authors and Affiliations
Contributions
PW drafted and wrote the manuscript. CRG and THM commented and revised the intellectual content of the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Peter Wostyn is the inventor on U.S. Patent No. US 10,980,437 B2 “Biomarkers for visual impairment and intracranial pressure (VIIP) syndrome”. The other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wostyn, P., Gibson, C.R. & Mader, T.H. The odyssey of the ocular and cerebrospinal fluids during a mission to Mars: the “ocular glymphatic system” under pressure. Eye 36, 686–691 (2022). https://doi.org/10.1038/s41433-021-01721-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01721-9