Abstract
Purpose
Primary central nervous system lymphoma (PCNSL) is a non-Hodgkin lymphoma involving the brain with possible leptomeningeal and ocular involvement. This study aimed to evaluate the safety and efficacy of modified intravitreal injection regimen of methotrexate (MTX) for therapeutic management of vitreoretinal lymphoma.
Materials and methods
Forty human immunodeficiency virus (HIV)–negative Chinese patients with primary vitreoretinal lymphoma were included in this retrospective noncomparative interventional case series study. Patients were treated with a modified protocol of intravitreal injection of MTX (400 µg/0.1 ml) according to the Intensive-Consolidation-Maintenance regimen. The Intensive phase of once-weekly intravitreal injections for 1 month, followed by the Consolidation phase of one injection every 2 weeks for 1 month, and then the Maintenance phase of once monthly for 1 month, for a total of 7 injections. The primary main outcome measures were clinical response to intravitreal chemotherapy, number of injections for clinical remission, progression-free survival (PFS), overall survival (OS), visual acuity (VA), complications during the study period, and cause of death were investigated.
Results
The duration of follow-up from the commencement of injection of MTX was 12–73 months (median 28, 30.55 ± 14.73 months). A total of 61 eyes of 40 patients were cleared clinically from malignant cells after a median 6.57 ± 3.12 (median 6, range 1–14) times of injection of MTX. A second remission was induced in 3 patients, who were treated with a further course of intravitreal chemotherapy after tumour recurred in their eyes. The median PFS and OS were 20.82 months (95% CI 14.64–27.01) and 29.29 months (95% CI 16.16–42.41), respectively. Complications that occurred during the period of treatment and follow-up included corneal epitheliopathy (3 of 61 eyes) and cataract (6 of 61 eyes). There were no cases of maculopathy, vitreous haemorrhage, optic atrophy, and sterile endophthalmitis. No patient had an irreversible loss of vision that could be attributed to the intravitreal injection of MTX.
Conclusions
It can be concluded that the modified intravitreal injection regimen of MTX is an effective therapeutic approach in inducing clinical remission of intraocular involvement in PCNSL patients, associated with few complications. However, further study needs to be conducted to indicate whether the proposed approach extends life expectancy.
Highlights
-
Primary central nervous system lymphoma (PCNSL) can involve the vitreous and retina and is associated with a poor clinical outcome, with a survival rate of less than 3 months in absence of undergoing an effective therapeutic strategy. Methotrexate (MTX) is the most efficient cytotoxic drug for patients with vitreoretinal involvement in primary vitreoretinal lymphoma (PVRL), through intravitreal injection of MTX.
-
In our experience, the modified protocol of intravitreal MTX according to the Intensive-Consolidation-Maintenance regimen, was effective in inducing clinical remission of PVRL with few complications. The accumulating clinical results brought us to propose the consideration of this protocol as a good first-line treatment option for PVRL.
Similar content being viewed by others
Introduction
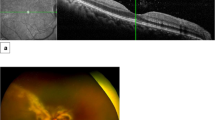
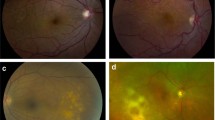
Primary central nervous system lymphoma (PCNSL) is defined as lymphoma restricted in the central nervous system (CNS), as presented in the brain, spinal cord, leptomeninges, or ocular involvement. The incidence of PCNSL is 0.27 per 100,000 person-years in the immunocompetent population, and 4.7 per 1000 person-years among patients with acquired immunodeficiency syndrome (AIDS) [1,2,3,4]. Ocular involvement, generally referred to as primary vitreoretinal lymphoma (PVRL), occurs in approximately one-quarter of patients with PCNSL [5]. The hallmark of intraocular involvement of PCNSL is the presence of vitreous cells (Fig. 1), which is often misdiagnosed as the chronic or non-responsive uveitis [6], and subretinal infiltrates (Fig. 2A–D).
A In patients with intraocular lymphoma, the presence of vitreal cells, mainly in grayish-white clumps, which is often misdiagnosed as chronic or non-responsive uveitis. B Structural OCT images from eyes with intraocular lymphoma for the presence of a double-layer sign (red arrow) to determine if the double-layer sign predicted subclinical intraocular lymphoma.
A Fundus photograph taken at the time of presentation with intraocular lymphoma, showing multiple lesions of subretinal malignant infiltrates. B Post-treatment of fundus photograph showed underwent intravitreal injections, most of the lesions resolved (case 14). C Colour fundus photographs showed yellow-white, like ice-cream retinal infiltrating lesions in the superior temporal quadrants. D Post-treatment of fundus photograph showed underwent intravitreal injections, most of the lesions resolved (case 3).
In patients with PCNSL, an extremely poor prognosis was reported, with a survival rate of less than 3 months in absence of undergoing an effective therapeutic strategy [1, 7]. The treatment protocols, such as orbital irradiation, chemotherapy [8,9,10], and combination of chemotherapy and radiotherapy, were investigated to control tumour growth successfully [11].
External beam radiation has been extensively utilised in different centres for the treatment of vitreoretinal lymphoma. However, although radiotherapy may induce an ocular remission, the lymphoma may recur [4], and further irradiation places the patients at a high risk of irreversible vision loss caused by radiation retinopathy [12]. Radiation therapy to the eye may cause remarkable ocular complications, including optic neuropathy, cataract formation, dry eyes, radiation retinopathy, and prolonged corneal epithelial defects [13]. Besides, with the existence of tumour relapses, there is a theoretical risk of intracranial diffusion, jeopardising the survival of patients. As the blood–ocular barriers may limit the penetration of chemotherapeutic agents into the eye, systemic high-dose intravenous methotrexate (MTX) may lead to recur after an initial response [14]. Due to the above concerns regarding orbital irradiation treatment and systemic chemotherapy, a protocol has been developed to treat vitreoretinal involvement in PCNSL patients through intravitreal injection of MTX at the Oregon Health & Science University (Portland, OR, USA), and that protocol was modified at the Hadassah-Hebrew University Medical Center (Jerusalem, Israel) [13, 15,16,17]. The treatment protocol included injection of 400 µg/0.1 ml MTX intravitreally twice weekly for 4 weeks, once weekly for 8 weeks, and then once monthly for 9 months, for a total of 25 injections. This management was proved effective in terms of inducing clinical remission of ocular involvement in PCNSL patients accompanied by acceptable morbidity [16, 17].
Although the Frenkel’s [17] treatment is accepted by many medical centres, however, the problem with the old protocol was the large number of injections (25 per year per eye). Thus, to further explore the more optimised treatment for PVRL, we decided to use a new protocol to see if fewer injections would still be effective. In this study, we introduce a new modified protocol of intravitreal MTX which has been used and validated in treating PVRL in over 40 patients at Beijing Tongren Hospital for ten years.
Material and methods
We reviewed the medical records with biopsy-confirmed PCNSL patients with vitreoretinal involvement, who were treated by intravitreal chemotherapy between April 2009 and August 2019 at Beijing Tongren Hospital. Those with human immunodeficiency virus positive were excluded. For cases that have no systemic history of lymphoma at presentation, a vitreous biopsy was performed to confirm the diagnosis. The intravitreal protocol was approved by the Institutional Review Board of Beijing Tongren Hospital. All patients had agreed and signed the informed consent forms.
In this study, the Intensive phase of once-weekly intravitreal injection of MTX was applied for 1 month. A dose of 400 µg/0.1 ml MTX was injected using a 29-gauge needle. It was followed by the Consolidation phase of one injection every 2 weeks for 1 month, and the Maintenance phase with once-monthly MTX injections for 1 month, adding up to a total of 7 injections. If patients achieved remission before 7 injections, they would stop the injections; if patients did not achieve remission after a full course of 7 injections, they would start another course of 7 injections until achieving the clinical remission. If the intraocular lesions recurred during the follow-up period, the above treatment protocol was repeated. The treatment was terminated if patients were unwell due to the systemic disease or suffered from serious ocular complications.
At each visit, patients were examined with visual acuity (VA) examination, intraocular pressure (IOP) measurement, slit-lamp biomicroscopy, and dilated fundus examination by fundus photography and optical coherence tomography (OCT). The data collected were as follows: demographic characteristics, biopsy diagnosis; initial location of the tumour; aqueous humour concentration of interleukin 10 (IL-10) to interleukin 6 (IL-6) ratio, status of the extraocular disease, total number of intravitreal injections, clinical response to therapy (including indications of clinical remission, absence of infiltrating cells in vitreous, retina, optic disc and choroid); the number of injections performed for clinical remission; complications observed during the study period and outcome, duration of follow-up, other interventions (such as vitrectomy, systemic and intrathecal chemotherapy, and radiotherapy), duration of survival after diagnosis, and cause of death if applicable. Pre-treatment and post-treatment of VA, as well as the main cause of significant loss of VA (Snellen chart reduced by 2 or more lines) was determined.
Statistical analysis
Demographic data were analysed using descriptive statistics. OS and PFS were calculated from the date of diagnosis to the date of last follow-up, relapse/progression, or death from any cause. The probabilities of PFS was estimated using the Kaplan-Meier method and the log-rank test for survival comparison. Stata version 15.0 (StataCorp LLC, College Station, TX, USA) was used to implement. Statistical analysis of the data between baseline and follow-up in each group were performed. Means ± SD or median (min-max) were reported for continuous variables. Mean values between groups in continuous variables were compared using independent t-tests. Wilcoxon rank-sum (Mann–Whitney) test was used for those continuous variables which were with non-normal distribution, and Chi-square was used to compare categorical data between the two groups. P values and confidence intervals (CI) were two sided. P values less than 0.05 were considered statistically significant.
Results
Patient’s characteristics
61 eyes of 40 patients with intraocular lymphoma were treated by proposed intravitreal injections of MTX from April 2009 to August 2019. The median age was 60.68 ± 10.07 years (median 62.50, range 31–81 years). The patients’ demographic and clinical data were summarised in Table 1a. The diagnosis of lymphoma was confirmed by vitrectomy of 12 eyes of 8 patients (Fig. 3). A total of 61 eyes of 40 patients were diagnosed with PVRL of the B-cell lymphoma. It was disclosed that 19 patients had a monocular disease. Of the 21 patients who had binocular disease, 7 had monocular involvement at initial examination and developed involvement of the fellow eye, with a mean interval of 15.43 ± 11.67 months (median19, range 2–28 months). The IL10/IL6 > 1 was detected in 40 eyes (65%) of 29 patients.
In 21 patients, the eye symptoms preceded the CNS symptoms. The mean interval between the involvement of eye and CNS was 23.00 ± 5.48 months (median 25, range 14–28 months). In 19 patients, the CNS involvement preceded the eye symptoms, with a mean interval of 17.50 ± 11.32 months (median 17, range 0.5–48 months).
We treated only those eyes that were clinically involved intraocular lymphoma. Intravitreal chemotherapy with MTX was taken as the sole treatment of intraocular lymphoma for the 40 patients. The overall response rate for evaluable patients was 100%. Among them, 24 PCNSL patients with ocular involvement had relapses of intracranial lesions and were treated with systemic chemotherapy, and then, further treated sequentially by intravitreal injection of MTX during the study period. Since completion of the study, 3 patients underwent systemic chemotherapy for the CNS involvement, as well as intravitreal injection of MTX. In addition, 1 patient had axillary lymph node metastasis, and she underwent biopsy and was diagnosed as the B-cell lymphoma.
In all the cases, a “double-layer” sign between the RPE and Bruch membrane was observed in the OCT, which was related to the disruption of the retinal barrier by lymphoma.
Efficacy of the therapy
61 treated eyes from 40 patients were cleared from malignant cells after intravitreal injections, the median number of intravitreal injections per patient was 6 (range of the number of injections, 1–14). Forty-two eyes (69%) had 7 or less injections and the mean number of injections per eye was 5 injections mean 4.86 ± 1.65 (median 4, range 1–7). In 6 eyes of 3 patients, an ocular relapse was noted in association with intracranial relapse at 12–24 months after clinical remission of the PVRL (Table 1b).
Besides, 12 eyes were clinically cleared from malignant cells after receiving vitrectomy, before commencing intravitreal chemotherapy. However, the PVRL relapsed again after undergoing vitrectomy (mean 3.12 ± 0.57 months [median 3, range 2–4] later) and received the same treatment of intravitreal injection of methotrexate. Patients who had binocular PVRL showed no difference in response to the intravitreal injection of MTX between the eye that underwent vitrectomy and non-treated eyes.
The data describing the VA were presented in Table 1c. Moreover, 16 eyes of 14 patients had ≥3 lines of VA improvement (ranging from a mean initial VA of 20/200 to a mean final VA of 20/40). Eyes with poor initial VA (CF) had not significantly changed, less improved from a mean initial VA of CF of 15 cm to a mean final VA of CF of 50 cm. On the other hand, eyes with satisfactory initial VA (20/25–20/20, Snellen chart) did not remarkably change. In 2 eyes of 2 patients, VA notably deteriorated (from LP to NLP) during the study period. In 6 eyes of 6 patients, cataract was found to be noticeable, and corrective surgery was not performed.
With a median follow-up of 30.55 ± 14.73 months (median 28, range 12–73), 6 eyes of 3 patients had relapsed, and 7 patients had died due to the progress of intracranial lymphoma. No patients died from treatment-related causes. In addition, 9 of 30 patients survived at least 5 years after initial diagnosis, while none of them had an ocular relapse. The median PFS and OS were 20.82 months (95% CI 14.64–27.01) and 29.29 months (95% CI 16.16–42.41), respectively (Fig. 4). We are currently following the remaining patients as well.
Complications
The main adverse effect related to intravitreal injection was corneal epitheliopathy (3 eyes, 0.5%), acceleration of existing cataract (6 eyes, 1%). The vitreous haemorrhage, sterile endophthalmitis, maculopathy, and optic atrophy were not observed in any of the patients. A transient elevation of IOP was found after intravitreal injection (2 eyes, 0.3%), however, no sustained IOP elevation was not present.
None of the patients developed severe corneal epitheliopathy. In the majority of patients, corneal epitheliopathy was either untreated or responded to a course of lubricant eye drops. Limbal stem cell deficiency was not observed as well. During the study period, cataract surgery with intraocular lens implantation did not undertake in the 6 eyes.
Discussion
To our knowledge, this was the largest PVRL series in the Asian population. In the study, we described the clinical characteristics of patients with PVRL, as well as long-term follow-up of their response to the modified regimen of intraocular injections of MTX. Our findings included the number of injections required for clinical remission, PSF, OS, effects on VA, and resulting complications.
A subset of PCNSL [18], vitreoretinal lymphoma (VRL) is a rare ocular malignancy. Therapies that have been successful in systemic lymphomas have not been reliably effective in PCNSL and VRL. Limitation of drug delivery through the blood–ocular barriers was a major challenge in the treatment of patients with PCNSL. The blood-retinal barrier was the most key point of clinical treatment for PVRL [19], because tumour primarily affects posterior ocular segments, including vitreous, retina, and optic nerve [15]. MTX, as the most efficient cytotoxic drug for patients with PCNSL, may result in a relatively low drug concentrations in the vitreous when a systemic “high-dose” regimen was used [20,21,22], which was not sufficient to clear lymphoma, while the related systemic toxicity may be remarkable [15, 21]. Instead, de Smet et al. [23] revealed that a sole intravitreal injection of MTX (400 µg/0.1 ml) was helpful to achieve tumoricidal levels within the eye (>1 µmol/l) for 5 days. However, previous studies described the need for a large number of injections (a maximum of 12 or 25 MTX injections) to clear clinically malignant cells [15, 17]. And in Smith’s series, six of a total of 26 eyes (23%) developed biopsy-proven ocular recurrence, occurring in association with intracranial recurrence, 12–24 months after clinical remission of the intraocular lymphoma [15].
In the current study, the protocol was amended in which the duration of the Consolidation phase and Maintenance phase was taken equal to 1 month. Concerning treating PVRL, we treated 61 eyes of 40 patients with PCNSL through the “Intensive-Consolidation-Maintenance” regimen of intravitreal injection of MTX combined with multiple systemic and/or intracranial treatments. In all the treated eyes, clinical remission of the intraocular lymphoma was demonstrated during the follow-up by absence of vitreous cells and resolution of retinal infiltration [24]. Most affected eyes (n = 42, 69%) were successfully treated at the end of the third month of management. In addition, 12 eyes were clinically cleared from tumours after undergoing vitrectomy, before the start of intravitreal chemotherapy. It was noteworthy that lymphoma relapsed after receiving vitrectomy, and there was no significant difference in response to the intravitreal injection of MTX between those patients who underwent vitrectomy and others. Three patients experienced the tumour relapses within the eyes, the second remission could be achieved by administering a further course of intravitreal chemotherapy. On the other hand, no eyes occurred the irreversible vision loss, which may be due to this further modified treatment regimen. Thus, it was of great importance to reduce the number of injections and finish the treatment protocol after 3 months. Nevertheless, it remained elusive whether there was a relapse if the treatment was not maintained after the maintenance period. Hence, further studies with a larger sample size need to be conducted.
In this study, a modified “Intensive-Consolidation-Maintenance” regimen was employed to treat the PVRL via intravitreal injection of MTX (400 µg/0.1 ml). In all patients, the final ophthalmic examination indicated that there was no lymphoma, and death (n = 7, 17.5%) was attributed to intracranial progression. Clinical ocular examinations were sufficiently sensitive to detect the intraocular tumour cells which may eventually induce relapses of lymphoma. In 19 of 40 patients, CNS involvement preceded the eye symptoms, with a mean interval of 17.50 ± 11.32 months between onset of CNSL and VRL. Hence, it is important to suspect the diagnosis in any patient with a history of either CNSL or systemic lymphoma with vitreous cells or retinal infiltrates. Although it was disclosed that the majority of patients with PCNSL and PVRL were of B-cell origin, a limited number of patients yielded T-cell lymphoma [17, 25]. Therefore, early vitrectomy with immediate cytological evaluation can ascertain the clinical diagnosis of PVRL [26, 27]. It has been reported that the sensitivity of RT-qPCR in the diagnosis of PVRL was only 64% [27,28,29]. Hence, the application of cytokines for distinguishing PVRL from uveitis has been previously studied. It was noteworthy that IL-10 was produced by malignant B lymphocytes in intraocular and CNS lymphoma, while IL-6 was generated in high levels by inflammatory cells in uveitis [30, 31]. Measurement of the ratio of IL-10/ IL-6 in vitreous was also helpful in the diagnosis of PVRL [31]. In the present study, we collected and analysed the aqueous humour samples to measure the levels of IL-6 and IL-10; and indicated the IL-10/IL-6 ratio can further improve the efficacy of diagnosis.
A limited number of complications were observed during the study period. In the current study, band keratopathy developed in 3 patients. MTX is probably responsible for eyes with corneal epitheliopathy, according to the effects of antimetabolites on the proliferated epithelium. Generally, the condition was mild, which was resolved spontaneously or after using eye lubricants without influencing vision. At that time, they had mild signs of dryness, which resolved within a relatively temporary side effect. Progression of preexisting cataract was observed as a common complication in 6 patients who underwent vitrectomy during the study period. However, this may be observed in healthy individuals as a consequence of aging. Remarkably, no eyes of irreversible vision loss or sequelae were attributed to the intravitreal injection of MTX. Smith et al. [15] reported other complications, such as corticosteroid-responsive sterile endophthalmitis, vitreous haemorrhage [17], neovascularization of the iris (NVI) or neovascularization glaucoma (NVG), maculopathy, and optic atrophy. Maculopathy, associated with significantly irreversible vision loss [32], may be related to intravitreal injection of MTX. In our study, treatment with intravitreal injection of MTX not resulted in these severe complications.
Rituximab was a chimeric monoclonal antibody targeting against the pan-B-cell marker CD20, has been studied as an adjunctive treatment for PVRL [33, 34]. However, only initial data in conjunction with MTX are available. Hence, it may be used to either reduce the MTX concentration or the number of injections required to prevent a relapse. Thus, alternative treatments, e.g. Rituximab, have not extensively utilised as the first line of treatment.
The main limitations of this study include its retrospective nature, some patient loss to follow-up, mostly due to patient death caused by CNS disease, and the lack of genetic analysis. In addition, the study was performed in one centre, potentially introducing selection bias. The main strength of the study is that all the patients were treated by one experienced ophthalmologist (WB. W) over a 10-year period using a unfirm treatment protocol.
Conclusion
Treatment of vitreoretinal lymphoma by intravitreal injection of MTX is currently used by a growing number of scholars who reported promising results [15, 17, 35,36,37]. However, the modified intravitreal injection regimen presented in this study may achieve complete clinical remission of vitreoretinal lymphoma with fewer injections. This makes it more acceptable for the patients and reduces complications of treatment. The accumulating clinical results brought us to propose the consideration of this protocol as a good first-line treatment option for intraocular lymphoma. Further studies were accordingly required to develop long-term studies based on this modified and effective regimen and indicate whether the proposed protocol can improve life expectancy.
Summary
What was known before
-
Primary central nervous system lymphoma (PCNSL) involving the ocular has a poor vision and clinical outcome, with a survival rate of less than 3 months in absence of undergoing an effective therapeutic strategy. Methotrexate (MTX), as the most efficient cytotoxic drug for patients with vitreoretinal involvement in primary intraocular lymphoma (PIOL), through intravitreal injection of MTX.
What this study adds
-
We evaluated the safety and efficacy of a proposed protocol of intravitreal MTX in the management of PCNSL involving the eye.
-
In our experience, the modified intravitreal chemotherapy with methotrexate was effective in inducing clinical remission of intraocular tumour in PCNSL with few complications. The accumulating clinical results brought us to propose the consideration of this protocol as a good first-line treatment option for intraocular lymphoma.
Data availability
Availability of data and materials: The data of this case report are available from the corresponding author on reasonable request.
References
Coté TR, Manns A, Hardy CR, Yellin FJ, Hartge P. Epidemiology of brain lymphoma among people with or without acquired immunodeficiency syndrome. AIDS/Cancer Study Group. J Natl Cancer Inst. 1996;88:675–9.
Levy-Clarke GA, Chan CC, Nussenblatt RB. Diagnosis and management of primary intraocular lymphoma. Hematol Oncol Clin North Am. 2005;19:739–49. viii.
Newell ME, Hoy JF, Cooper SG, DeGraaff B, Grulich AE, Bryant M, et al. Human immunodeficiency virus-related primary central nervous system lymphoma: factors influencing survival in 111 patients. Cancer. 2004;100:2627–36.
Schabet M. Epidemiology of primary CNS lymphoma. J Neurooncol. 1999;43:199–201.
Hochberg FH, Miller DC. Primary central nervous system lymphoma. J Neurosurg. 1988;68:835–53.
Coupland SE, Heimann H, Bechrakis NE. Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clin Exp Ophthalmol. 2004;242:901–13.
Jellinger K, Radaskiewicz TH, Slowik F. Primary malignant lymphomas of the central nervous system in man. Acta Neuropathol Suppl. 1975;6:95–102.
Doolittle ND, Miner ME, Hall WA, Siegal T, Jerome E, Osztie E, et al. Safety and efficacy of a multicenter study using intraarterial chemotherapy in conjunction with osmotic opening of the blood-brain barrier for the treatment of patients with malignant brain tumors. Cancer. 2000;88:637–47.
Hoang-Xuan K, Delattre JY. Ongoing protocols for non-AIDS primary central nervous system lymphoma [review]. J Neurooncol. 1999;43:287–91.
Kraemer DF, Fortin D, Doolittle ND, Neuwelt EA. Association of total dose intensity of chemotherapy in primary central nervous system lymphoma (human non-acquired immunodeficiency syndrome) and survival. Neurosurgery. 2001;48:1033–40. discussion 1040–1.
Schlegel U, Schmidt-Wolf IGH, Deckert M. Primary CNS lymphoma. Clinical presentation, pathological classification, molecular pathogenesis and treatment. J Neurol Sci. 2000;181:1–12.
Zamber RW, Kinyoun JL. Radiation retinopathy [published erratum appears in West J Med 1993;158:201]. West J Med. 1992;157:530–3.
Fishburne BC, Wilson DJ, Rosenbaum JT, Neuwelt EA. Intravitreal methotrexate as an adjunctive treatment of intraocular lymphoma. Arch Ophthalmol. 1997;115:1152–6.
Batchelor TT, Kolak G, Ciordia R, Foster CS, Henson JW. High-dose methotrexate for intraocular lymphoma. Clin Cancer Res. 2003;9:711–5.
Smith JR, Rosenbaum JT, Wilson DJ, Doolittle ND, Siegal T, Neuwelt EA, et al. Role of intravitreal methotrexate in the management of primary central nervous system lymphoma with ocular involvement. Ophthalmology. 2002;109:1709–16.
Hoffman PM, McKelvie P, Hall AJ, Stawell RJ, Santamaria JD. Intraocular lymphoma: a series of 14 patients with clinicopathological features and treatment outcomes. Eye. 2003;17:513–21.
Frenkel S, Hendler K, Siegal T, Shalom E, Pe’er J. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br J Ophthalmol. 2008;92:383–8. https://doi.org/10.1136/bjo.2007.127928.
Abrey LE, Yahalom J, DeAngelis LM. Treatment for primary CNS lymphoma; the next step. J Clin Oncol. 2000;18:3144–50.
Goldberg S, Frenkel S, Blumenthal EZ, Solomon A, Pe’er J. Intraocular lymphoma. Ophthalmology. 2007;114:1236–7.
Castellino A, Pulido JS, Johnston PB, Ristow KM, Bennani NN, Inwards DJ, et al. Role of systemic high-dose methotrexate and combined approaches in the management of vitreoretinal lymphoma: a single center experience 1990-2018. Am J Hematol. 2019;94:291–8. https://doi.org/10.1002/ajh.25350.
Cunha-Vaz J. The blood-ocular barriers. Surv Ophthalmol. 1979;23:279–96.
Henson JW, Yang J, Batchelor T. Intraocular methotrexate level after high-dose intravenous infusion [letter]. J Clin Oncol. 1999;17:1329.
de Smet MD, Stark-Vancs V, Kohler DR, Smith J, Wittes R, Nussenblatt RB. Intraocular levels of methotrexate after intravenous administration. Am J Ophthalmol. 1996;121:442–4. https://doi.org/10.1016/s0002-9394(14)70444-1.
Abrey LE, Batchelor TT, Ferreri AJM, Gospodarowicz M, Pulczynski EJ, Zucca E, et al. Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol. 2005;23:5034–43. https://doi.org/10.1200/JCO.2005.13.524.
White VA, Gascoyne RD, Paton KE. Use of the polymerase chain reaction to detect B- and T-cell gene rearrangements in vitreous specimens from patients with intraocular lymphoma. Arch Ophthalmol. 1999;17:761–5.
Coupland SE, Bechrakis NE, Anastassiou G, Foerster AM, Heiligenhaus A, Pleyer U, et al. Evaluation of vitrectomy specimens and chorioretinal biopsies in the diagnosis of primary intraocular lymphoma in patients with Masquerade syndrome. Graefes Arch Clin Exp Ophthalmol. 2003;241:860–70. https://doi.org/10.1007/s00417-003-0749-y.
Benson WE. Vitrectomy. In: Spaeth GL, ed. Ophthalmic Surgery: Principles and Practice. Philadelphia: W.B. Saunders; 1982. p. 410–30.
Rhodes CH, Glantz MJ, Glantz L, Lekos A, Sorenson GD, Honsinger C, et al. A comparison of polymerase chain reaction examination of cerebrospinal fluid and conventional cytology in the diagnosis of lymphomatous meningitis. Cancer. 1996;77:543–8. 10.1002/(SICI)1097-0142(19960201)77:3<543::AID-CNCR17>3.0.CO;2-4.
Shen DF, Zhuang Z, LeHoang P, Böni R, Zheng S, Nussenblatt RB, et al. Utility of microdissection and polymerase chain reaction for the detection of immunoglobulin gene rearrangement and translocation in primary intraocular lymphoma. Ophthalmology. 1998;105:1664–9. https://doi.org/10.1016/S0161-6420(98)99036-4.
Chan CC, Whitcup SM, Solomon D, Nussenblatt RB. Interleukin-10 in the vitreous of patients with primary intraocular lymphoma. Am J Ophthalmol. 1995;120:671–3. https://doi.org/10.1016/s0002-9394(14)72217-2.
Buggage RR, Whitcup SM, Nussenblatt RB, Chan CC. Using interleukin 10 to interleukin 6 ratio to distinguish primary intraocular lymphoma and uveitis [letter]. Invest Ophthalmol Vis Sci. 1999;40:2462–3.
Millay RH, Klein ML, Shults WT, Dahlborg SA, Neuwelt EA. Maculopathy associated with combination chemotherapy and osmotic opening of the blood-brain barrier. Am J Ophthalmol. 1986;102:626–32. https://doi.org/10.1016/0002-9394(86)90536-2.
Wong ET, Tishler R, Barron L, Wu JK. Immunochemotherapy with rituximab and temozolomide for central nervous system lymphomas. Cancer. 2004;101:139–45. https://doi.org/10.1002/cncr.20339.
Kitzmann AS, Pulido JS, Mohney BG, Baratz KH, Grube T, Marler RJ, et al. Intraocular use of rituximab. Eye. 2007;21:1524–7. https://doi.org/10.1038/sj.eye.6702804.
Biccler JL, Savage KJ, Brown PDN, Jørgensen J, Larsen TS, Poulsen CB, et al. Risk of death, relapse or progression, and loss of life expectancy at different progression-free survival milestones in primary central nervous system lymphoma. Leuk Lymphoma. 2019;3:1–8. https://doi.org/10.1080/10428194.2019.1594219.
de Smet MD, Vancs VS, Kohler D, Solomon D, Chan CC. Intravitreal chemotherapy for the treatment of recurrent intraocular lymphoma. Br J Ophthalmol. 1999;83:448–51. https://doi.org/10.1136/bjo.83.4.448.
Wang JK, Yang CM, Lin CP, Shan YD, Lo AY, Tien HF. An Asian patient with intraocular lymphoma treated by intravitreal methotrexate. Jpn J Ophthalmol. 2006;50:474–8. https://doi.org/10.1007/s10384-005-0327-4.
Funding
The National Natural Science Foundation of China (Nr. 81272981), the Beijing Natural Science Foundation (Nr. 7151003) provided financial support.
Author information
Authors and Affiliations
Contributions
WWB: Examination of patient, interpretation of results, writing the manuscript; ZN: Interpretation of results and writing/reviewing of manuscript; XXL: Interpretation of results and reviewing of manuscript. WYX: Reviewing of manuscript. LYM: Examination and treatment of patient. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study followed the tenets of the Declaration of Helsinki and its ethical standards of 1964. The study was approved by the Medical Ethics Committee of the Beijing Tongren Hospital, and written informed consent was obtained from all participants.
Consent for publication
All authors consent to publish the manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, N., Xu, X., Liu, Y. et al. A proposed protocol of intravitreal injection of methotrexate for treatment of primary vitreoretinal lymphoma. Eye 36, 1448–1455 (2022). https://doi.org/10.1038/s41433-021-01657-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01657-0