Abstract
Purpose
To investigate the efficacy of lid wipes (LWs) containing terpinen-4-ol and sodium hyaluronate (Hy-ter®) for the treatment of seborrheic blepharitis compared to baby shampoo (BS).
Methods
This randomized, double-blind, active control, parallel group, multicentre clinical trial included 48 eyes of 48 patients with seborrheic blepharitis who were randomly divided into two treatment arms (1:1, n = 24) using block randomization. LWs or BS were prescribed twice a day for 8 weeks followed by a discontinuation period of 4 weeks. Change in Blepharitis Symptom measure (BLISS), Schirmer’s test, tear breakup time (TBUT), noninvasive TBUT (NI-TBUT), ocular surface disease index (OSDI) score, corneal and conjunctival staining, meibography, and Demodex count at different visits (Baseline, 4th, 8th, and 12th week) were the main outcome measures.
Results
The baseline values of both groups were similar (p > 0.05). Despite high clinical efficacy in both treatment arms, patients using LWs showed a lower BLISS score at the 8th and 12th-week visit (1.9 ± 2.2 versus 7.2 ± 6.6, p = 0.003; 4.0 ± 1.3 versus 5.8 ± 6.3, p = 0.026). NI-TBUT showed a significant increase starting from the 4th week for patients using LWs and 8th week for patients using BS. Both treatment modalities caused a reduction in the Demodex count after 4 weeks of treatment (p < 0.001). The treatment withdrawal did not cause any recurrence in both treatment arms.
Conclusion
BS or LWs containing Hy-ter® can be used with good efficacy for the treatment of seborrheic blepharitis. However, LWs may provide a better symptomatic relief compared to BS after 8 weeks of treatment.
Similar content being viewed by others
Introduction
Blepharitis is inflammation of the eyelids and is one of the most common reasons for ocular discomfort. It can be classified according to the anatomical location as anterior or posterior; however, it has traditionally been classified as staphylococcal, seborrheic, meibomian gland dysfunction (MGD), or mixed blepharitis [1]. All types of blepharitis have common clinical findings such as itching, burning, redness, irritation, etc. [2]. Dry eye can also be observed concurrently in patients with blepharitis. In total, 25–40% of patients with seborrheic blepharitis and MGD and 50% of patients with staphylococcal blepharitis have been reported to have dry eye [1].
While immune reactivity against the staphylococcal antigens has been implicated in the pathogenesis of staphylococcal blepharitis, Demodex mite infestation of the eyelids has been implicated in both anterior and posterior blepharitis [3]. However, the exact etiopathogenesis of the disease is unclear. The treatment approach for blepharitis is based mainly on lid hygiene which includes eyelid massage, warm compresses, and eyelid scrubs [4]. Patients with blepharitis can benefit also from the short-term use of the topical steroids. However, some patients can develop resistant symptoms due to chronic blepharitis [5]. Several different treatment options are available for chronic blepharitis targeting mainly the Demodex mites such as tea tree oil (TTO), terpinen-4-ol (T4O) [6, 7], ivermectin, metronidazole [8], castor oil [9], permethrin [10], etc.
Numerous clinical trials have been conducted with an effort to provide an efficient treatment approach [11, 12]. Topical TTO or T4O treatment (shampoo or lid wipes (LWs)) have shown great success in recent studies, especially to reduce the Demodex infestation [6, 7, 13]. However, although almost all implicated treatment options showed benefits for the eradication of the mites and the amelioration of the blepharitis-related symptoms, included patients in most of the studies were heterogeneous [4]. Furthermore, most of the studies lack the results of treatment after discontinuation for a specific period.
In this clinical trial, we aimed to investigate the efficacy of treatment with LWs containing T4O and sodium hyaluronate (Hy-ter®) compared to BS in patients with seborrheic blepharitis in terms of the change in tear film functions, dry eye, and blepharitis-related symptoms, Demodex count, and meibomian gland (MG) functions during and after the discontinuation of the treatment.
Methods
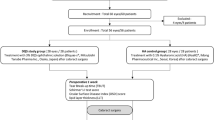
This multicenter, prospective, randomized, double-blind, active control, parallel group clinical trial assessing the efficacy of LWs containing T4O and sodium hyaluronate versus BS included patients with seborrheic blepharitis who were randomly divided into two treatment arms (LWs containing T4O and sodium hyaluronate versus baby shampoo (BS)) using block randomization (1:1). Since the sample size is small, block randomization was preferred to reduce bias and achieve balance in the allocation of participants to treatment arms. Computer generated randomization list was used and the list was kept concealed for the investigators recruiting the patients. The study was conducted according to the Declaration of Helsinki and it was approved as a prospective study by the local ethical committee. Informed consent was obtained from the patients before the first examination. The clinical trial was registered in the clinicaltrials.gov (NCT04441528).
The age and gender of the patients were recorded as demographics. Only the right eyes of the patients were included in the analysis. Patients were referred to the ophthalmology department from the dermatology clinic with the diagnosis of seborrheic dermatitis. Only the patients with the diagnosis of seborrheic blepharitis were included in the study. The diagnosis of seborrheic blepharitis was made upon the typical clinical findings as hyperaemic and greasy anterior lid margins with soft scales and adherence of lashes to each other.
Patients with ophthalmological pathologies that may affect the tear film functions including ocular rosacea, contact lens use, history of any ocular surgery, or patients with systemic pathologies including rheumatic diseases, thyroid disorders, diabetes mellitus, etc. or those using systemic medications that may affect the tear film functions including corticosteroids, antibiotics, immunosuppressants, fish oil, flaxseed oil, and other omega-3 supplements were excluded from the study. Patients younger than 18-year-old or those who used any treatment for blepharitis within the 6 months prior to the examination were excluded from the study.
LWs containing T4O and sodium hyaluronate (Hy-ter®, Blefastop®, NTC, Italy) or BS (Johnson’s Baby Shampoo, Johnson & Johnson, New Jersey, USA) were prescribed twice a day for 8 weeks followed by a discontinuation period of 4 weeks. Patients in both treatment arms were advised not to apply warm compresses. LWs and BS were given in blinded boxes and bottles, respectively. BS was diluted with clean water (1:1 mixture) and transferred to opaque bottles for blinding. The patients were asked to apply it with clean fingertips to the eyelashes together with gentle pressure on the eyelids for 1 min while eyes were closed, followed by rinsing off the BS with clean water at room temperature. Patients in the LW group were asked to apply the LWs with gentle pressure on the eyelids for 1 min as well to provide a similar massage effect as in BS. The patients were masked for the ingredient of the treatment but were informed about the form of the treatment (a bottle of shampoo versus LWs). The examiners were masked for the treatment type of the patients and did not take part in the explanation part of the treatment. The application was demonstrated at the enrollment visit and written instructions were given to the patients. Unused products were returned to the investigator explaining the use of the products at the end of the 8 weeks and weighed as a measure of participant compliance.
Schirmer’s test, tear breakup time (TBUT), average noninvasive TBUT (NI-TBUT), ocular surface disease index (OSDI) score, Blepharitis Symptom measure (BLISS), corneal and conjunctival staining score, meibography, and Demodex count were evaluated at each visit. The flow diagram of the trial is summarized in Supplementary Table 1.
Schirmer’s test was performed at the same hour of the day without topical anesthesia. TBUT was performed after staining with a fluorescein strip at least 30 min after Schirmer’s test. Three measurements were taken from each eye as recommended by the DEWS report 2007 [14] and the average of the three results was calculated. The corneal and conjunctival staining was graded from 0 to 5 using the Oxford scale. OSDI scores were calculated according to the response of the patients to the questionnaire. OSDI test includes 12 questions that are divided into three parts: (1) questions 1–5 refer to ocular pain or visual difficulties such as blurred vision or light sensitivity; (2) questions 6–9 are about visual functionality questioning the ability to read or drive at night; and (3) questions 10–12 evaluate environmental factors such as air conditioning or wind. The responses range between 0 and 4 with 0 indicating none of the time and 4 indicating always. The OSDI score range between 0 and 100.
BLISS score of the patients was also calculated according to the response of the patients to the questionnaire developed by Hosseini et al. [15]. This questionnaire includes questions assessing the followings: eyes that itch; eyes that burn; eyelids feel heavy or puffy; feel like something is in your eye; dry eyes; gritty eyes; irritated eyes; eyes that tear or water; crusty eyes; flaking from your eyelids; eyelids that are stuck together; red eyes or eyelids; and debris like pieces of skin, or dandruff in your eyes. The patients were asked to choose any of the following as an answer for each question: none of the time, occasionally, frequently, or all of the time.
NI-TBUT was measured using the Sirius anterior segment analysis system (Sirius; CSO, Florence, Italy). The participants were asked to blink twice and then to keep the eyes open as long as possible. Three successive measurements were taken for each eye. The average time of all the breakup intervals forming on the cornea was recorded as the average noninvasive tear breakup time. Average NI-TBUT was used in the analysis.
Upper and lower MGs were evaluated using the meibography mode of the Sirius anterior segment analysis system. First, the upper or lower eyelid was everted, and imaging of the MGs was obtained from the tarsal conjunctival surface. For selecting the clearest image, at least six shots were taken from the upper and lower tarsal conjunctival surfaces. During the analysis, the clearest image of the MG structures was selected from these six images and the eyelid borders were marked, and then, the borders of the MGs were marked with the device’s software. The device calculates the loss in the MGs, and the result is given according to the rate of loss. The total loss area was obtained as the average of the upper and lower eyelid loss areas.
Eyelash epilation from patients with seborrheic blepharitis was performed similarly to the modified method described by Gao et al. [16]. Four eyelashes from each eye, two from the upper lid and two from the lower lid were epilated carefully with a fine forceps. Only the lashes with cylindrical dandruff or the lashes with brittle root were selectively epilated and were put separately on each end of a glass slide. One drop of 10% potassium hydroxide (KOH) was pipetted and put on the epilated lashes and a coverslip was placed carefully onto the lashes. The samples in KOH were examined within 10–15 min using light microscopy at ×10–40 magnification. The presence and the total number of mites were recorded.
The duration of treatment for blepharitis is unclear and there is no consensus for when to stop or for how long to continue the treatment. Previous studies on the treatment of blepharitis reported different treatment protocols. Determining the duration of treatment can be related to the life cycle of Demodex mites. Demodex larvae hatch after 3–4 days and the larvae develop into adults in 7 days. The life cycle of a mite is ~14 days and the total life span is several weeks [17]. Therefore, 4 weeks of treatment covers two lifecycles of Demodex. Most of the studies preferred to design the study to evaluate the treatment response after 4 or 8 weeks of use [7, 12, 18,19,20]. However, at least 2 weeks of treatment has also been studied due to the 2-week life cycle of Demodex [21, 22]. Although all of the studies evaluated the treatment response in patients with blepharitis, none of the studies investigated the effect of treatment discontinuation. In our study, we monitored the patients after 4 and 8 weeks of treatment and another 4 weeks of treatment discontinuation.
Statistical analysis
The normal distribution of the samples was evaluated with the Shapiro–Wilk test. For the comparison of the ratio between the groups, a chi-square test or a Fisher’s exact test was utilized. For the comparison of the means among different visits for dependent groups, the Friedman test was used as the omnibus test, and a Wilcoxon signed-rank test with Bonferroni correction was used for the post hoc analysis between the groups at different visits. For the comparison of the means of independent groups, the Mann–Whitney U test was used. For the correlation analysis, Spearman’s correlation test was used.
For sample size calculations, we used the reduction in BLISS score [10, 15]. For detecting a clinically significant difference of five points with the standard deviation of normal values as 5 and a two-sided significance level of 0.05, and a power of 90%, a minimum of 22 participants were required. Openepi software was used for the sample size calculation and SPSS software (version 21.0) was utilized for all of the remaining statistical analyses. p values below 0.05 were accepted as statistically significant.
Results
Sixty-two patients with a diagnosis of seborrheic blepharitis were assessed for eligibility for the study. However, six patients declined to participate in the study and eight patients did not meet the inclusion criteria. Therefore, 48 eyes of 48 patients were included in the analysis and divided into two treatment arms (n = 24). The mean age of the patients using LWs was 29.2 ± 11.8 years and it was 33.7 ± 12.5 years for patients using BS (p = 0.199). While 12 (50%) of the patients using LWs were male and 12 (50%) were female, 10 (41.7%) of the patients using BS were male and 14 (58.3%) were female (p = 0.562).
The change of dry eye parameters and symptom scores at different visits for both treatment arms is presented in Table 1. BLISS score showed a significant decrease among different visits for both treatment arms (BS, p = 0.008; LWs, p < 0.001). While the BLISS score showed a significant decrease for 8 weeks in patients using LWs (0–4th week, p < 0.001; 4–8th week, p < 0.001), no significant change was observed after the discontinuation of the treatment in the last 4 weeks (p = 0.756). However, patients using BS showed a decrease in the BLISS score only in the first 4 weeks (p < 0.001) without any significant change throughout the following 8 weeks (4–8th week, p = 1.0; 8–12th week, p = 1.0). While NI-TBUT showed a significant increase starting from the 4th week for patients using LWs (0–4th week, p = 0.048), it showed an increase starting from the 8th week (0–4th week, p = 0.112; 0–8th week, p = 0.048) for patients using BS which was maintained after the discontinuation of the treatment (p = 1.0). OSDI score did not show any change in patients using BS (p = 0.072); however, patients using LWs had better OSDI scores throughout the first 8 weeks (0–4th week, p = 0.044; 4–8th week, p = 0.02) and this decrease was maintained in the last 4 weeks (p = 1.0). The corneal and conjunctival staining score, Schirmer’s test, and MG loss area did not show any significant change in both treatment arms. None of the patients reported any side effects during their treatment within the study period.
The comparison of tear film functions, dry eye, and blepharitis-related symptoms between two treatment arms for each visit using the Mann–Whitney U test is presented in Table 2. The baseline data are also presented in the same table. The change of parameters in time is also visualized in Fig. 1. The baseline characteristics of the patients in both treatment arms were similar. Patients using LWs showed significantly lower BLISS scores compared to patients using BS at the 8th and 12th week visit (p = 0.003, p = 0.026, respectively). Patients using LWs showed significantly higher MG loss area at the 12th week visit compared to the patients using BS (p = 0.02). The other parameters did not show any significant difference between the two treatment arms at any visit.
Patients using lid wipes showed a better symptomatic relief compared to baby shampoo after 8 weeks of treatment. NI-TBUT showed earlier improvement in patients using lid wipes. TBUT tear breakup time, NI-TBUT noninvasive tear breakup time, OSDI ocular surface disease index, BLISS Blepharitis Symptom scale.
The change of Demodex count per lash is shown in Table 3 for both treatment arms. Both LWs and BS led to a significant reduction in the Demodex count (p < 0.001) and Demodex positivity (p < 0.001) during the first 4 weeks of treatment. A significant recurrence of Demodex positivity was not observed in both treatment arms after the discontinuation of the treatment during the last 4 weeks (Table 3).
Comparison of the mean amount of change of all parameters at each visit is shown in Table 4. The change of Schirmer’s test between the baseline visit and the 12th week visit in patients using LWs (2.4 ± 10.0 mm) was higher than the patients using BS (−2.3 ± 9.7 mm, p = 0.024). The change of TBUT, NI-TBUT, MG loss area, corneal and conjunctival staining score, and Demodex count per lash showed no significant difference between LW and BS group at any time period (Table 4). The decrease of OSDI score was significantly more prominent in patients using LWs compared to the patients using BS between 0–8th week visits (−9.2 ± 9.8 versus −0.8 ± 9.9, p = 0.024) and 4–8th week visits (−4.9 ± 8.5 versus 2.3 ± 6.8, p = 0.012). Similarly, the amelioration of the BLISS score was significantly more prominent in patients using LWs compared to the patients using BS between 0 and 8th week visits, 0 and 12th week visits, 4 and 8th week visits, and 4 and 12th week visits (p = 0.011, p = 0.009, p < 0.001, p = 0.002, respectively).
The correlation analysis between all parameters and BLISS score and Demodex count per lash is shown in Supplementary Table 2. BLISS score showed a very strong positive correlation with the OSDI score among all patients included in the study (r = 0.981, p < 0.001) without any significant correlation with the other parameters.
LW users did not return any product showing full compliance in all patients whereas BS users returned the bottle with varying amounts of BS. However, compliance comparison was not possible for the two different application methods.
Discussion
In this prospective, randomized clinical trial, both BS and LWs containing T4O and sodium hyaluronate (Hy-ter®) showed symptomatic improvement and significant Demodex reduction in the treatment of seborrheic blepharitis. However, while BS provided significant blepharitis-related symptomatic relief until the 4th week, the symptomatic relief of the LWs continued until the 8th week leading to better symptom scores at the end of the 8 and 12 weeks compared to the BS. Both treatment modalities caused a significant reduction in the Demodex count after 4 weeks of treatment which was maintained even after the withdrawal of the treatment in the last 4 weeks. The discontinuation of the treatment did not cause any symptomatic or tear film function-related recurrence in both treatment arms.
The previous clinical trials investigating the efficacy of different treatment options have used various primary outcomes such as Demodex count, OSDI, Standard Patient Evaluation of Eye Dryness, and Symptom Assessment iN Dry Eye scores. The primary outcome of the present study was the BLISS score which evaluated the blepharitis-related symptoms [15]. We believe that the main point in the care of blepharitis patients should be the symptomatic relief of patients. Because especially the tear film functions or Demodex count might not be correlated with the symptoms of the patients and they are prone to be affected by various ocular pathologies. In our study, the BLISS score showed a very strong positive correlation with the OSDI score. However, most of the previous studies utilized dry eye-related questionnaires [9, 12] rather than a disease-specific questionnaire.
In this study, both BS and LWs provided a significant decrease in the BLISS score. After a similar decrease in the BLISS score after the first 4 weeks, LWs continued its effect longer than BS and provided a more prominent decrease in the BLISS score at both 8th and 12th week visits (Tables 2 and 4 and Fig. 1). Sodium hyaluronate in the LWs might have provided improvement in tear film functions. Castor oil, one of the ingredients of the Blefastop® LWs, has also been shown to improve the symptoms of patients with blepharitis [9]. T4O has been shown to have anti-inflammatory activity and may also contribute to the superiority of the LWs [23]. On the other hand, BS has phenoxyethanol which may cause reduced tear film stability [24] and possible skin irritant fragrances [25] as ingredients. BS can also breakdown the lipid layer of the tear film due to its detergent effect and this may contribute to irritation [12]. The longer effect of LWs might also be attributed to different application methods. However, the application of both treatments included some pressure for the same duration (1 min) on eyelids while applying the LWs or BS. Although the change of NI-TBUT showed no significant difference between the two treatment arms during the treatment or after its withdrawal, NI-TBUT values showed earlier improvement in patients using LWs. These above-mentioned advantages of the LWs and the possible disadvantages of the BS might also explain the later improvement in NI-TBUT in blepharitis patients using BS in the present study. Improvement of the OSDI scores in two groups was parallel to the change of the BLISS scores.
Blepharitis patients can show different clinical characteristics according to the blepharitis type (staphylococcal, seborrheic, etc.). Most of the previous clinical trials included a heterogeneous group of patients [6, 20] making the results suspicious [4]. Because a specific treatment approach might show different treatment efficacy for different types of blepharitis. Therefore, randomized controlled trials should be designed to include patients with a specific condition such as seborrheic blepharitis as in our study. In this way, type I errors can be prevented by minimizing the imbalances between groups.
The Demodex mite has been implicated in the pathogenesis of blepharitis due to its higher infestation rate in blepharitis patients despite conflicting results from the studies showing its similar infestation rate in healthy eyelids [26]. In this study, we did not observe any significant correlation of Demodex count with the symptom scores or tear film functions. Therefore, we speculate that Demodex infestation might not have an impact on the symptoms or tear film functions of patients with seborrheic blepharitis and its eradication might not be the objective of the treatment. However, Lee et al. observed that the Demodex count showed strong positive correlations with the OSDI score and 1/TBUT [27]. The difference between our study and the study by Lee et al. might be related to the difference of blepharitis type included in the study. We also showed that 44 (91.7%) of 48 patients with seborrheic blepharitis had Demodex positivity. However, Arici et al. observed Demodex positivity in only 28.8% of patients with seborrheic blepharitis [28]. The difference in the rate might result from the difference in the mounting agent which is used after the epilation of the eyelashes (KOH versus olive oil).
MG dysfunction can develop due to chronic posterior blepharitis [29]. Although seborrheic blepharitis causes anterior blepharitis by affecting primarily the glands of Zeis, it may also involve MGs to a lesser degree causing posterior blepharitis leading to a destruction in the MGs [29]. Therefore, in our study, we evaluated the MG loss in both treatment arms and showed that the blepharitis-related symptoms were not correlated to the MG loss. Both treatment arms did not reverse the MG loss and 4 weeks of treatment withdrawal did not increase the MG loss despite the absence of a longer follow up. Therefore, we suggest that the MG destruction in seborrheic blepharitis may be irreversible. However, the MG loss was not compared to a healthy control group in this study.
Limitations of the study include the lack of analysis of the tear inflammatory molecule levels. Although not studied, the inflammatory molecule levels might be correlated with the blepharitis-related symptoms and the treatment strategy may be focused on providing anti-inflammation in addition to the lubrication as in T4O and sodium hyaluronate in the LWs, rather than focusing on Demodex eradication. We also did not include or subdivide the patients according to the severity of the symptoms or clinical findings, because the main focus of the study was to investigate the efficacy of the treatment in a homogenous patient cohort. Another limitation of the study is the lack of the results of longer follow up after discontinuation of the treatment. The different application method of the two treatment arms (i.e., shampoo versus wipes) is another limitation of the study. However, we asked for patients to apply both treatments with their fingers by applying some pressure on the eyelids to make the treatment arms approximately similar in terms of the massage effect on the MGs.
In conclusion, in this study, both LWs and BS provided an improvement in the symptoms when applied twice a day for 8 weeks. However, LWs provided a better and longer symptomatic relief compared to BS. The discontinuation of treatment for 4 weeks did not cause any recurrence in the disease in terms of the symptoms or the tear film functions or the Demodex count in both treatment arms. LWs containing Hy-ter® provided an earlier improvement in the NI-TBUT values. The clinicians should consider these minor differences during the treatment decision process.
Summary
What was known before
-
Tea tree oil-based treatment for blepharitis provided improvement in dry eye-related symptom scores and tear inflammatory molecule profile.
What this study adds
-
Both baby shampoo and lid wipes containing terpinen-4-ol and sodium hyaluronate provided improvement in the symptoms.
-
Lid wipes provided improvement in the blepharitis specific symptoms for a longer time including the discontinuation of the treatment for 4 weeks after 8 weeks of treatment.
-
Lid wipes provided an earlier improvement in the noninvasive tear breakup time values.
References
McCulley JP, Dougherty JM, Deneau DG. Classification of chronic blepharitis. Ophthalmology. 1982;89:1173–80.
Amescua G, Akpek EK, Farid M, Garcia-Ferrer FJ, Lin A, Rhee MK, et al. Blepharitis preferred practice pattern®. Ophthalmology. 2019;126:P56–93.
Ficker L, Ramakrishnan M, Seal D, Wright P. Role of cell-mediated immunity to staphylococci in blepharitis. Am J Ophthalmol. 1991;111:473–9.
Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012:CD005556. https://doi.org/10.1002/14651858.CD005556.pub2.
Demircan A, Altan C, Azman FE, Alkin Z, Kucuksumer Y, Demirok A. Tear properties in eyes with chronic blepharitis. Turk J Ophthalmol. 2012;42:346–8.
Murphy O, O’Dwyer V, Lloyd-McKernan A. The efficacy of tea tree face wash, 1, 2-Octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Contact Lens Anterior Eye. 2018;41:77–82.
De Luca V, Carnevali A, Carnovale Scalzo G, Piccoli G, Bruzzichessi D, Scorcia V. Efficacy and safety of wet wipes containing Hy-Ter® solution compared with standard care for bilateral posterior blepharitis: a preliminary randomized controlled study. Ophthalmol Ther. 2019;8:313–21.
Salem DAB, El-shazly A, Nabih N, El-Bayoumy Y, Saleh S. Evaluation of the efficacy of oral ivermectin in comparison with ivermectin-metronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infect Dis. 2013;17:e343–7. https://doi.org/10.1016/j.ijid.2012.11.022.
Muntz A, Sandford E, Claassen M, Curd L, Jackson AK, Watters G, et al. Randomized trial of topical periocular castor oil treatment for blepharitis. Ocul Surf. 2021;19:145–50.
Hecht I, Melzer-Golik A, Sadi Szyper N, Kaiserman I. Permethrin cream for the treatment of demodex blepharitis. Cornea. 2019;38:1513–8.
Navel V, Mulliez A, Benoist d’Azy C, Baker JS, Malecaze J, Chiambaretta F, et al. Efficacy of treatments for Demodex blepharitis: a systematic review and meta-analysis. Ocul Surf. 2019;17:655–69.
Sung J, Wang MTM, Lee SH, Cheung IMY, Ismail S, Sherwin T, et al. Randomized double-masked trial of eyelid cleansing treatments for blepharitis. Ocul Surf. 2018;16:77–83.
Gao YY, Xu DL, Huang LJ, Wang R, Tseng SCG. Treatment of ocular itching associated with ocular demodicosis by 5% tea tree oil ointment. Cornea. 2012;31:14–17.
Anon. The definition and classification of dry eye disease: report of the definition and classification subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:75–92.
Hosseini K, Bourque LB, Hays RD. Development and evaluation of a measure of patient-reported symptoms of Blepharitis. Health Qual Life Outcomes. 2018;16:11. https://doi.org/10.1186/s12955-018-0839-5.
Gao YY, Di Pascuale MA, Li W, Liu DTS, Baradaran-Rafii A, Elizondo A, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Investig Ophthalmol Vis Sci. 2005;46:3089–94.
Rather PA, Hassan I. Human demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59:60–6.
Hirsch-Hoffmann S, Kaufmann C, Bänninger PB, Thiel MA. Treatment options for demodex blepharitis: patient choice and efficacy. Klin Monbl Augenheilkd. 2015;232:384–7.
Alver O, Kıvanç SA, Akova-Budak B, Tüzemen NÜ, Ener B, Özmen AT. A clinical scoring system for diagnosis of ocular demodicosis. Med Sci Monit. 2017;23:5862–9.
Epstein IJ, Rosenberg E, Stuber R, Choi MB, Donnenfeld ED, Perry HD. Double-masked and unmasked prospective study of terpinen-4-ol lid scrubs with microblepharoexfoliation for the treatment of demodex blepharitis. Cornea. 2020;39:408–16.
Fulk GW, Murphy B, Robins MD. Pilocarpine gel for the treatment of demodicosis—a case series. Optom Vis Sci. 1996;73:742–5.
Behrens-Baumann W, Niederdellmann C, Jehkul A, Kohnen R. Bibrocathol-augensalbe ist wirksam bei blepharitis. Ergebnisse einer randomisierten, doppelblinden, kontrollierten klinischen Stud Ophthalmol. 2006;103:960–5.
Hart PH, Brand C, Carson CF, Riley TV, Prager RH, Finlay-Jones JJ. Terpinen-4-ol, the main component of the essential oil of Melaleuca alternifolia (tea tree oil), suppresses inflammatory mediator production by activated human monocytes. Inflamm Res. 2000;49: 619–26. https://pubmed.ncbi.nlm.nih.gov/11131302/. Accessed 3 Dec 2020.
Wieslander G, Norbäck D. Ocular symptoms, tear film stability, nasal patency, and biomarkers in nasal lavage in indoor painters in relation to emissions from water-based paint. Int Arch Occup Environ Health. 2010;83:733–41.
Zirwas M, Moennich J. Shampoos. Dermatitis. 2009;20:106–10.
Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10:505–10.
Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between demodex and ocular discomfort. Investig Ophthalmol Vis Sci. 2010;51:2906–11.
Arici MK, Sümer Z, Toker MI, Erdoǧan H, Topalkara A, Akbulut M. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiol. 2005;12:287–90.
Putnam CM. Diagnosis and management of blepharitis: an optometrist’s perspective. Clin Optom. 2016;8:71–8.
Acknowledgements
KUTTAM provided baby shampoo and lid wipes and their blinded box and bottles for the study.
Author information
Authors and Affiliations
Contributions
CA was responsible for the study hypothesis, study design, interpretation of the results, literature review, writing the manuscript, and critical review of the manuscript. BM was responsible for extracting and analyzing data, reviewing the literature, and writing the manuscript. AS was responsible for the study hypothesis, study design, interpretation of the results, literature review, writing a part of the manuscript, and critical review of the manuscript. AYT was responsible for extracting data, reviewing the literature, and writing a part of the manuscript. HBT, ET, and YOB were responsible for microbiological examinations, reviewing the literature, and writing a part of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Arici, C., Mergen, B., Yildiz-Tas, A. et al. Randomized double-blind trial of wipes containing terpinen-4-ol and hyaluronate versus baby shampoo in seborrheic blepharitis patients. Eye 36, 869–876 (2022). https://doi.org/10.1038/s41433-021-01642-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01642-7