Abstract
Objective
To determine the normal intraocular pressure in a sample of Egyptian children 0–12 years of age, and compare it to that recorded in previous studies.
Methods
This is a prospective cross-sectional study, including 345 eyes. All children underwent complete history taking and ophthalmic examination. Any glaucomatous patients or glaucoma suspects were excluded. Intraocular pressure was measured using Haag Streit Perkins M2 handheld applanation tonometer under topical or general anaesthesia. Three readings were recorded for each eye and the average was calculated. Central corneal thickness was measured, using handheld pachymeter (Pachmate 2), whenever possible.
Results
The study included 345 eyes of 187 children (101 males and 86 females), aged 2 months to 12 years (mean: 5.69 ± 3.42 years). The recorded IOP was 5–20 mm Hg (mean: 11.5 ± 2.34 mm Hg). Central corneal thickness was 469–742 μm (mean: 564.8 ± 42.72 μm). The mean recorded intraocular pressure showed positive correlation with increased age (p = 0.026) and increased central corneal thickness (p = 0.037), with a difference of 1 mm Hg for every 100-μm change in central corneal thickness. The mean IOP was significantly lower than that recorded by most previous studies. A detailed comparative analysis is presented comparing our findings with other studies including grouped analysis, by country, ethnicity and tonometers used.
Conclusions
The mean IOP in a group of normal Egyptian children was 11.5 ± 2.34 mm Hg, with positive correlation to age and central corneal thickness. This mean intraocular pressure was lower than that previously reported in any other population.
Similar content being viewed by others
Introduction
‘Childhood glaucoma’ or ‘paediatric glaucoma’ is often associated with significant visual loss and characterised by elevated intraocular pressure (IOP) and optic-disk cupping. It may be primary, in which a developmental abnormality of the anterior chamber angle only exists, or secondary. Primary glaucoma in children is generally divided, according to age of onset, into primary congenital glaucoma, from birth to early childhood, and juvenile primary open-angle glaucoma, from 4 years to early adulthood. Secondary glaucoma includes a variety of conditions resulting from damage to the aqueous outflow system due to congenital or acquired ocular diseases or systemic disorders [1, 2]. IOP is a crucial risk factor of glaucoma that can be lowered medically or surgically to control the course of the disease [3,4,5]. It is an important tool in early diagnosis and monitoring of this significant cause of childhood blindness [6]. To achieve this goal, knowledge of the normal values of IOP in infants and children is necessary.
Previous studies have reported the normal IOP values in different populations [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22], but none has reported the normal IOP values in Egyptian children. As normal IOP values vary in different populations, it is essential that each population develops its individual normative data. As childhood glaucoma is not rare in Egypt, with a prevalence of 2.36 per 10,000 live births [23], knowledge of the normal IOP values in Egyptian children was deemed necessary for proper management and visual salvage of these children.
The aim of this study was to document the normal IOP values in the Egyptian paediatric age group of 0–12 years of age, to allow proper diagnosis and management of childhood glaucoma in Egyptian children. The second aim was to statistically compare IOP values obtained by the current study to those obtained in previous ones by meta-analysis.
Methods and materials
This is a prospective study conducted in the Ophthalmic Department of the Children’s Hospital of Cairo University between May 2018 and September 2019. The ethics committee of Children’s Hospital of Cairo University, the ethics committee of the Ophthalmic Department, the Council of the Ophthalmic Department, the Council of the Faculty of Medicine and Cairo University council have approved the study protocol. The study protocol followed the tenets of the Declaration of Helsinki. Informed consent was obtained from either the parents or the legal guardian of the child.
The study included 345 eyes of a sample of Egyptian children aged 0–12 years of age. Assuming a margin of error of 5% and confidence interval 95% in a target population as many millions, the following formula was used for sample size calculation: n = Nx / ((N – 1)E2 + x), where n is the sample size, E is the margin of error and N is the population size. Inclusion criteria involved children 0–12 years, with other indication for general anaesthesia rather than mere IOP measurement, or feasibility for IOP measurement under topical anaesthesia while awake. Exclusion criteria involved any of the following: age exceeding 12 years, refusal to participate, uncooperative children with no indication for general anaesthesia, systemic or topical medications during the week preceding the examination (if known to affect the IOP), local or systemic diseases or syndromes with known association with glaucoma, previous ocular surgery, glaucoma (as suspected by a corneal diameter corneal diameter >11.5 mm during the first year or >12.5 mm in older children, Haab’s striae or a cup/disc ratio >0.2 during the first year of life or >0.3 in older children), corneal opacities or keratitis, conjunctivitis or a positive regurge test.
Evaluation on entry into the study involved history taking and clinical examination. Inquiry was made for sex, age, previous medications, surgeries or general diseases and previous ocular or extraocular surgery, allergy, inflammation or infection.
Clinical evaluation was performed while the child was awake, under topical Benoxinate hydrochloride 0.4% (Benox® 0.4 % eye drops), if cooperative with other indications for general anaesthesia. Uncooperative children, with another indication for general anaesthesia, were examined during the early stages of induction with Sevoflurane, before intubation. IOP was measured in stage one, according to Guedel’s classification, in which the pupil is normal in size, still reactive to light with regular breathing, and normal blood pressure but irregular pulse. This was done under guidance of the anaesthesiologist.
Clinical examination involved anterior segment evaluation (lid, conjunctiva, cornea, anterior chamber, pupil, iris and lens) using oblique illumination and/or slit-lamp examination, regurge test to exclude nasolacrimal duct obstruction, dilated fundus examination, extraocular muscles examination, measurement of white to white horizontal corneal diameter using sterile Castroviejo calliper, measurement of central corneal thickness using handheld pachymeter (Pachymate®) and IOP measurement. Obtaining IOP measurements was done using Perkin’s MK2 handheld applanation tonometer (Haag Streit, UK). Anesthetised or sedated children were examined in recumbent position. Awake ones were examined in sitting position. At least three readings were recorded, to ensure stable measurements, and the average of these was calculated. This average IOP will be subsequently used for all statistical calculations.
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 25 (IBM Corp., Armonk, NY, USA). Data were summarised using mean and standard deviation (SD) for quantitative variables, and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were done using unpaired t test, when comparing two groups, and analysis of variance (ANOVA) with multiple comparisons post hoc test, when comparing more than two groups. For comparing categorical data, χ2 test was performed. Exact test was used instead when the expected frequency was less than 5. Correlations between quantitative variables were done using Pearson correlation coefficient. Kappa measure of agreement was used to test agreement between categorical variables. P values less than 0.05 were considered as statistically significant.
The IOP was statistically described in terms of mean ± SD. The current study was compared to each available study using the Student t test for independent samples.
Regarding the meta-analysis, data from the included studies were analysed using Review Manager (RevMan – version 5.2, The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark), and Microsoft Excel 2010 (Microsoft Corp., Redmond, WA, USA). We expressed pooled as the mean difference (MD) with 95% CI subgrouped by country, race and instrument. We explored and quantified between-study statistical heterogeneity using the I2 test. Because heterogeneity was statistically significant (p < 0.05) and I2 was >50%, we used the DerSimonian and Laird random-effects model instead [24].
Forest plots were done using Review Manager (RevMan) [Computer programme], Version 5.3. (2014; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Results
The current study
The current study prospectively recruited data of 345 eyes of 187 patients. These included 176 eyes of 101 males and 169 eyes of 86 females. Among these, 171 were right and 174 were left eyes. Age ranged between 2 months and 12 years, with a mean age of 5.69 ± 3.42 years and a median age of 5 years. Patients were divided into five groups according to age: Group 1 (n = 39, 11.3%), 0–1 year; Group 2 (n = 61, 17.6%), >1–3 years; Group 3 (n = 99, 28.6%), >3–6 years; Group 4 (n = 83, 24%), >6–9 years and Group 5 (n = 63, 18.2%), >9–12 years.
Systemic diseases included diabetes mellitus in one patient (0.5%) and two of the children were albino (1%). One patient (0.5%) received insulin injections. Two patients (1%) gave a history of previous testicular surgery and one (0.5%) had tonsillectomy.
A total of 121 eyes (35%) were examined, while the child was awake, under topical anaesthesia with Benoxinate hydrochloride 0.4%. Seventeen eyes (4.9%) were examined under sedation (using inhalation mask Sevoflurane). The latter were sedated for the purpose of undergoing minor procedures, like examination under general anaesthesia or suture removal of the fellow eye. Examination, during the induction stage of general anaesthesia using Sevoflurane (for major surgical procedures), was carried out on 207 eyes (60.1%).
Anterior segment examination revealed the presence of ptosis in 3 eyes (0.8%), chalazion in 3 eyes (0.8%), keratoconus in 4 eyes (1%) and cataract in 48 eyes (13.9%). Fundus examination revealed the presence of tigroid fundus (4 eyes, 1%), albinoid fundus (4 eyes, 1 %), tilted disc (2 eyes, 0.5%) and Coat’s disease (2 eyes, 0.5%). Strabismus was present in 74 patients (39.5%).
Data obtained on measuring the horizontal corneal diameter, CCT, cup/disc ratio and IOP are shown in Table 1. The CCT could be measured in only 155 eyes. There was significant agreement between the three recorded IOP measurements (kappa statistic = 0.854, p < 0.001). Patients were divided into three groups based on IOP levels: Group L (Low), with IOP up to 10 mm Hg; Group M (Moderate), with IOP 11–18 mm Hg and Group H (High), with IOP >18 mm Hg. Group L included 122 eyes (35.3%), Group M, 221 eyes (64.1%) and Group H, 2 eyes (0.6%).
The relationship of IOP to the different tested parameters was statistically evaluated. T test showed an insignificant relationship between mean IOP and sex (p = 0.547), as well as eye laterality (p = 0.311). The mean IOP was 11.42 ± 2.16 mm Hg in males and 11.57 ± 2.52 mm Hg in females (p = 0.547). The mean IOP was 11.37 ± 2.28 mm Hg in OD and 11.62 ± 2.40 mm Hg in OS (p = 0.311).
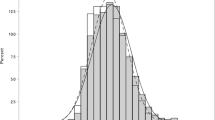
The relationship between age and IOP is shown in Table 1 and highlighted in Fig. 1A. ANOVA test showed a significant relationship between mean age and mean IOP level (p = 0.026). Post hoc pairwise comparison of IOP among the different age groups revealed significantly lower mean IOP levels in Group 1 than Groups 3 (p = 0.03), 4 (p = 0.008) and 5 (p = 0.026), as well as in Group 2 versus 4 (p = 0.023). The IOP, therefore, tends to be significantly lower in the first 3 years of life.
The relationship between IOP and awareness state was tested. T test showed an insignificant difference between mean IOP of awake participants (11.45 ± 2.04) and those examined under general anaesthesia (11.52 ± 2.49), p = 0.776.
The present study recorded a mean IOP of 11.5 ± 2.49 in the sitting position (121 children), as compared to 11.45 ± 2.04 mm Hg in the supine position (224 children), p = 0.77. Accordingly, posture did not significantly affect IOP levels.
Mean IOP was significantly lower in eyes with cataract (10.73 ± 2.26) than in those with clear crystalline lenses (11.58 ± 2.27), p = 0.024. This may, however, be attributed to the younger age of patients with congenital cataract (10.73 ± 2.26 months) in contrast to those with clear lenses (6.19 ± 14.4 years).
An insignificant relationship was found between mean IOP and horizontal corneal diameter (p = 0.051) as well as cup/disc ratio (p = 0.748). On the other hand, a significant correlation was documented between mean IOP and CCT (p = 0.037). Thicker corneas were associated with higher IOP values. For every 100-μm difference in CCT, there was 1 mm Hg change in IOP. This is highlighted in Fig. 1B.
Meta-analysis
The mean IOP obtained in the current study was significantly lower than previous studies (p < 0.05) [6,7,8,9,10,11,12,13,14,15,16,17, 20,21,22], Table 2. Comparisons of the mean IOP recorded in the current study to subgroups of previous studies, based on country, race, and instrument used to measure IOP, are shown in Figs. 2 and 3 and Supplementary Fig. 1, respectively. The mean IOP was significantly lower in the present study than all subgroups (p < 0.05), except black race, where the mean IOP in the present study was insignificantly lower (p = 0.04).
The weight of each comparison is expressed as a % of the total of the meta-analysis (100%). Each comparison is represented by a square (its size = study weight, and its centre is opposite to the difference in the mean of the current study and each of the other studies) on a straight line (representing the 95% CI of the mean’s difference). The subtotal of each subgroup and the final results of the meta-analysis are represented by the black diamond (its centre is the mean’s difference across all studies and the tips are the 95% CI of the mean’s difference across all studies). The equator line in the middle of the graph is opposite the 0 value. If the lines of any study and/or the diamond touch it, there is no statistical difference between the current and this study. Heterogeneity is represented by I2 statistic as a % and a p value. When the p value is <0.05, heterogeneity is considerable across the studies and the results should be taken cautiously. The test for the overall effect is represented by Z and p values. When the p value is <0.05, the overall result is statistically significant. The test for subgroup differences represents the significance of the difference across the subgroups, where a p value < 0.05 is significant.
Interpretation of the forest plots is the same as mentioned under Fig. 2.
Discussion
Glaucoma is a common cause of visual loss worldwide and in Egypt. IOP is a crucial and the main risk factor of glaucoma that can be manipulated medically or surgically to control the course of the disease. Other factors include low intracranial pressure, hypotension and diminished optic nerve perfusion [3]. Many factors contribute to IOP: constitutional, like corneal thickness and corneal hysteresis; and circumstantial, as postural position, time of the examination (physiological diurnal variation of IOP) and obtaining measurements under anaesthetics or sedatives [25, 26].
Different normal IOP levels were reported by previous studies [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22], which differed according to race, geographical distribution and instrument used to record the IOP [27]. To the best of our knowledge, no such study was conducted in Egypt or this region. The rationale for the present study was, therefore, to determine the normal IOP in a sample of Egyptian children, 0–12 years of age, to be used as a guide in the detection and management of congenital and juvenile glaucoma in Egypt, and to compare values obtained in Egyptian children to other populations.
This study is a prospective, cross-sectional clinical study that was conducted on 345 eyes of 187 participants, with a mean age of 5.69 ± 3.42 years (2 months to 12 years). Three IOP readings were recorded for each eye and the average of the three readings was documented. There was good agreement among the three recorded IOP measurements (kappa = 0.854, p = 0.001). Documented IOP was 5–20 mm Hg, with a mean of 11.5 ± 2.34.
There were no significant differences documented, in the present study, for the IOP values obtained in awake children (anaesthetised with Benoxinate hydrochloride 0.4% eye drops only), and those examined during the early stage of general anaesthesia using Sevoflurane. On the contrary, Blumberg et al. [28] and Buehner et al. [29], both found that Sevoflurane lowers IOP, even up to 8 min after the initial measurement. The absence of significant IOP lowering effect by Sevoflurane in the current study could be attributed to the strict insistence on measuring IOP during the early stage of anaesthesia.
The present study recorded a mean IOP of 11.5 ± 2.49 mm Hg in the upright position as compared to 11.45 ± 2.04 mm Hg in the supine position (p = 0.77). This does not agree with Weber and Price [25], who recognised increased IOP with postural change from upright to supine position, and attributed this to increase in episcleral pressure and uveal engorgement. A brief time is, presumably, needed before the effect of these mechanisms becomes prominent. As patients in the present were examined in the early stage of anaesthesia, there was, probably, no time for these mechanisms to take effect.
Interestingly, in the present study, the IOP was significantly lower in eyes with cataractous lenses than those with clear lenses (p = 0.023). The relationship between crystalline lens clarity and IOP was not previously reported in any other study. This finding needs further investigation in future, because of the limitation in current sample size (only 44 eyes with cataract). Moreover, it might be attributed to the young age of patients with congenital cataract for whom the IOP was recorded (10.73 ± 2.26 months), in contrast to the older age of those with clear lenses (6.19 ± 14.4 years). As shown in Table 1 and Fig. 1A, increasing age is associated with an increase in IOP.
In the current study, the measured central corneal thickness was 564.8 ± 42.72 μm with a range from 469 to 742 μm, and a positive correlation was found between CCT and IOP (p = 0.037), where the IOP increased by 1 mm Hg for every 100 microns increase in CCT (p = 0.03). The CCT varied among previous studies (Supplementary Fig. 2) [8, 14,15,16, 19, 20, 30,31,32]. Using different measurement techniques, numerous studies showed a positive correlation between CCT and measured IOP in children [8, 10, 15, 16, 20, 31, 33]. According to these studies, there has been a well-established quantitative relationship between CCT and IOP ranging from 0.32 to 3.5 mm Hg increase in measured IOP for every 100 µm increase in central corneal thickness. Alkhodari [22], however, found that the measured IOP increased as little as 0.024 and 0.022 mm Hg for the right and left eyes, respectively, for every 100 µm increase in central corneal thickness. On the contrary, Ehler et al. [34] found that for every 100:μm deviation from 520-μm CCT, misestimating the IOP by as much as 7 mm Hg could be expected.
This variance in values of quantitative relation among these studies is likely attributed to methodologies, instrumentations and time of measuring CCT and IOP values. In addition, the effect of IOP fluctuation was not taken into consideration though proved to be significant [35]. In general, there is a positive correlation between IOP and CCT and the present study agrees with this trend.
Previous studies, conducted to determine the normal IOP in various populations, are summarised in Table 2. By meta-analysis, the recorded IOP in the present study was significantly lower than all previous studies (Table 2). The IOP recorded here was, however, closest to the Nigerian [6], Indian [9], and Palestinian [22] IOP. Nevertheless, comparison with the Nigerian study is inappropriate, as the latter measured IOP only in neonates during the first week of life, while the present study included no neonates. The IOP documented here in Egyptian children was significantly lower than that recorded in children in other countries (Fig. 2), and significantly lower than Asian and white races, but insignificantly lower than children of the black race (Fig. 3). In the present study, IOP was recorded by Perkin’s handheld tonometer. It was significantly lower than IOP recorded by Perkin’s as well as other types of tonometers (Supplementary Fig. 1).
Among previous studies, conducted to determine the normal IOP in various populations, some used contact tonometers, others used noncontact tonometers (NCTs) and few used both contact and NCTs in the same study. It is noteworthy that the type of tonometer used could affect the level of IOP recorded and bias any comparison among different studies using different types of tonometers. Bradfield et al. [36] evaluated 439 subjects below 18 years of age and found, in an office setting, that Tono-Pen measurements were slightly lower than slit-lamp-mounted Goldmann applanation tonometry (GAT) when IOP was less than 11 mm Hg and slightly higher than GAT when IOP was greater than 11 mm Hg. Tono-Pen measurements were consistently slightly higher on average than handheld GAT under general anaesthesia. Better agreement was found among older children in both settings. Martinez-de-la-Casa et al. [37] measured IOP values of 18.5 ± 5.5 mm Hg with Icare rebound tonometry (IRT), 17.5 ± 3.8 mm Hg with GAT and 17.4 ± 5.6 mm Hg with NCT. Feng et al. [38] reported, in their study of 419 paediatric patients, MDs of −0.81 ± 2.74 mm Hg between IRT and NCT, of 1.81 ± 2.43 mm Hg between IRT and GAT and of 2.56 ± 2.36 mm Hg between NCT and GAT. Grigorian et al. [39] reported an IOP 1.38 mm Hg higher with IRT than GAT. Uzlu et al. [40] compared IOP measurements obtained with NCT, IRT and GAT in 110 eyes of 55 paediatric cases and reported highest IOP levels with IRT and lowest with GAT. MDs were 1.97 ± 0.15 between IRT without anaesthesia and GAT, 1.40 ± 0.14 between IRT with topical anaesthesia and GAT, 1.02 ± 0.193 between IRT and NCT, 0.45 ± 0.193 between IRT with topical anaesthesia and NCT and 0.95 ± 0.13 mm Hg between NCT and GAT (p < 0.05 for all). The variability in IOP measurements in different countries could, therefore, falsely reflect IOP variability due to instrument variability rather than country variability. Nevertheless, the inter-instrument variability, as noted by the above discussion, is mild and hardly exceeded 2 mm Hg.
Limitations to the current study included examination of all cases between 9 am and 2 pm, preventing a record of diurnal variations of IOP. In addition, no neonates were included in the study, as the youngest participant was 2 months of age. Moreover, measurement of IOP in children attending an ophthalmic clinic or theatre might have biased the results, as the IOP might have been affected by the associated ophthalmic pathology. Lastly, children were examined during the ‘early’ stages of anaesthesia before intubation, but still the exact timing of examination was not quantified in terms of minutes and seconds. As a recommendation for future studies is measurement of IOP in children attending a non-ophthalmic clinic or those anaesthetised for non-ophthalmic causes, to avoid any bias caused by the child’s ophthalmic pathology as cataract for example. Other recommendations involve inclusion of neonates and recording measurements throughout the 24 h, with accurate documentation and attempt at exact fixing of time of examination from the start of induction.
In conclusion, the IOP recorded in Egyptian children was 5–20 mm Hg, with a mean of 11.5 ± 2.34 mm Hg, which is significantly lower than the IOP measured in any other population. The measured central corneal thickness was 469–742 μm, with a mean of 564.8 ± 42.72 μm and had a significant relationship to IOP. For every 100 μm increase in CCT, an increase of IOP of 1 mm Hg was documented.
Summary
What was known before
-
The mean intraocular pressure measured by different studies in other populations was between 11.84 and 19.3 mm Hg.
-
No previous study measured the mean normal intraocular pressure in Egyptian children.
What this study adds
-
The IOP recorded in Egyptian children (2 months to 12 years old) was 5–20 mm Hg, with a mean of 11.5 ± 2.34 mm Hg, which is significantly lower than the IOP measured in any other population.
-
The measured central corneal thickness in Egyptian children was 469–742 μm, with a mean of 564.8 ± 42.72 μm and had a significant relationship to intraocular pressure.
-
For every 100-μm increase in CCT, an increase of IOP of 1 mm Hg was documented.
References
Papadopoulos M, Cable N, Rahi J, Khaw PT. BIG Eye Study InvestigatorsThe British Infantile and Childhood Glaucoma (BIG) Eye Study. Invest Ophthalmol Vis Sci. 2007;48:4100–6.
Marchini G, Tiscani M, Chemello F. Pediatric glaucoma: current perspectives. Pediatric Health Med Ther. 2014;5:15–27.
Baneke AJ, Aubry J, Viswanathan AC, Plant GT. The role of intracranial pressure in glaucoma and therapeutic implications. Eye. 2020;34:178–91.
ElSheikha OZ, Abdelhakim MASE, Elhilali HM, Kassem RR. Is viscotrabeculotomy superior to conventional trabeculotomy in the management of Egyptian infants with congenital glaucoma?. Acta Ophthalmol. 2015;93:e366–71.
Khalil DH, Abdelhakim MA. Primary trabeculotomy compared to combined trabeculectomy-trabeculotomy in congenital glaucoma: 3-year study. Acta Ophthalmol. 2016;94:e550–4.
Olatunji VA, Ademola-Popoola D, Adepoju FG, Adesiyun OO. Normal values of intraocular pressure in full-term Nigerian newborns. Saudi J Ophthalmol. 2016;30:185–8.
Doughty MJ, Laiquzzaman M, Muller A, Oblak E, Button NF. Central corneal thickness in European (white) individuals, especially children and the elderly, and assessment of its possible importance in clinical measures of intraocular pressure. Ophthalmic Physiol Opt. 2002;22:491–504.
Muir KW, Jin J, Freedman SF. Central corneal thickness and its relationship to intraocular pressure in children. Ophthalmology. 2004;111:2220–3.
Sihota R, Tuli D, Dada T, Gupta V, Scahdeva MM. Distribution and determinants of intraocular pressure in a normal pediatric population. J Pediatr Ophthalmol Strabismus. 2006;43:14–18.
Yildirim N, Sahin A, Basmak H, Bal C. Effect of central corneal thickness and radius of corneal curvature on intraocular pressure measured with the Tono-Pen and non-contact tonometer in healthy school children. J Pediatr Ophthalmol Strabismus. 2007;44:216–22.
Sahin A, Basmak H, Yildirim N. The influence of central corneal thickness and corneal curvature on intraocular pressure measured by tono-pen and rebound tonometer in children. J Glaucoma. 2008;17:57–61.
Song Y, Congdon N, Li L, Zhou Z, Choi K, Lam DS, et al. Corneal hysteresis and axial length among Chinese secondary school children: the Xichang Pediatric Refractive Error Study (X-PRES) report no. 4. Am J Ophthalmol. 2008;145:819–26.
Haider KM, Mickler C, Oliver D, Moya FJ, Cruz OA, Davitt BV. Age and racial variation in central corneal thickness of preschool and school-aged children. J Pediatr Ophthalmol Strabismus. 2008;45:227–33.
Hikoya A, Sato M, Tsuzuki K, Koide YM, Asaoka R, Hotta Y. Central corneal thickness in Japanese children. Jpn Ophthalmo. 2009;53:7–11.
Heidary F, Gharebaghi R, Wan Hitam WH, Naing NN, Wan-Arfah N, Shatriah I. Central corneal thickness and intraocular pressure in Malay children. PLoS One. 2011;6:e25208.
Krzyzanowska-Berkowska P, Asejczyk-Widlicka M, Pierscionek B. Intraocular pressure in a cohort of healthy eastern European schoolchildren: variations in method and corneal thickness. BMC Ophthalmol. 2012;12:61.
Sakalar YB, Keklikci U, Unlu K, Alakus MF, Yildirim M, Dag U. Distribution of central corneal thickness and intraocular pressure in a large population of Turkish school children. Ophthalmic Epidemiol. 2012;19:83–88.
Huang Y, Lin S, Ma D, Wang Z, Du Y, Lu X, et al. Corneal biomechanical properties and associated factors in school-age children. Eye Sci. 2013;28:34–39.
Bueno-Gimeno I, Gene-Sampedro A, Pinero-Llorens DP, Lanzagorta-Aresti A, Espana-Gregori E. Corneal biomechanics, retinal nerve fiber layer, and optic disc in children. Optom Vis Sci. 2014;91:1474–82.
Wei W, Fan Z, Wang L, Li Z, Jiao W, Li Y. Correlation analysis between central corneal thickness and intraocular pressure in juveniles in Northern China: the Jinan city eye study. PLoS One. 2014;9:e104842.
Reddy SC, Rosnita A. Tono-pen measurement of intraocular pressure under topical anaesthesia in full term normal newborns. Int J Ophthalmol. 2014;7:92–94.
Alkhodari HT. Distribution of central corneal thickness and intraocular pressure in emmetropic eyes of healthy children of Palestine. Int J Ophthalmol. 2019;12:496–503.
Mokbel TH, El Hefney EM, Hagras SM, ALNagdy AA, Badawi AE, Kasem MA, et al. Childhood glaucoma profile in Dakahelia, Egypt: a retrospective study. Int J Ophthalmol. 2018;11:674–80.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Weber AK, Price J. Pressure differential of intraocular pressure measured between supine and sitting position. Ann Ophthalmol. 1981;13:323–6.
David R, Zangwill L, Briscoe D, Dagan M, Yagev R, Yassur Y. Diurnal intraocular pressure variations: an analysis of 690 diurnal curves. Br J Ophthalmol. 1992;76:280–3.
Farvardin M, Heidary F, Sayehmiri K, Gharebaghi R, Jabbarvand, Behrooz M. A comprehensive meta-analysis on intra ocular pressure and central corneal thickness in healthy children. Iran J Public Health. 2017;46:724–32.
Blumberg D, Congdon N, Jampel H, Gilbert D, Elliott R, Rivers R, et al. The effects of sevoflurane and ketamine on intraocular pressure in children during examination under anesthesia. Am J Ophthlmol. 2007;143:494–9.
Buehner E, Pietsch UC, Bringmann A, Foja C, Wiedemann P, Uhlmann S. Effects of propofol and isoflurane anesthesia on the intraocular pressure and hemodynamics of pigs. Ophthalmic Res. 2011;45:42–46.
Hashemi H, Yazdani K, Mehravaran S, KhabazKhoob M, Mohammad K, Parsafar H, et al. Corneal thickness in a population-based, cross-sectional study: the Tehran eye study. Cornea. 2009;28:395–400.
Nejabat M, Heidary F, Talednejad MR, Salouti R, Nowroozzadeh MH, Masoumpour M, et al. Correlation between intraocular pressure and central corneal thickness in Persian children. Ophthalmol Ther. 2016;5:235–43.
Hashemi H, Saatchia M, Khabazkhoob M, Emamian MH, Yekta A, Fotouhi A. Distribution of corneal thickness and its determinants in 6-12-year-old children in an Iranian general population. J Curr Ophthalmol. 2017;31:150–6.
Gul A, Caglar C, Cinal A, Yasar T, Kilic A. Ocular biometry and central corneal thickness in children: a hospital-based study. Arq Bras Oftalmol. 2014;77:152–4.
Ehlers N, Bramsen T, Sperling S. Application tonometry and central corneal thickness. Acta Ophthalmol (Copenh). 1975;53:34–43.
Cheng J, Xiao M, Xu H, Fang S, Chen X, Kong X, et al. Seasonal changes of 24-hour intraocular pressure rhythm in healthy Shanghai population. Medicine (Baltimore). 2016;95:e4453.
Bradfield YS, Kaminski BM, Repka MX, Melia M, Pediatric Eye Disease Investigator Group, Davitt BV, et al. Comparison of Tono-Pen and Goldmann applanation tonometers for measurement of intraocular pressure in healthy children. J AAPOS. 2012;16:242–8.
Martinez-de-la-Casa JM, Jimenez-Santos M, Saenz-Frances F, Matilla-Rodero M, Mendez-Hernandez C, Herrero-Vanrell R, et al. Performance of the rebound, noncontact and Goldmann applanation tonometers in routine clinical practice. Acta Ophthalmol. 2011;89:676–80.
Feng CS, Jin KW, Yi K, Choi DG. Comparison of intraocular pressure measurements obtained by rebound, noncontact, and goldmann applanation tonometry in children. Am J Ophthalmol. 2015;160:937–43.
Grigorian F, Grigorian AP, Li A, Sattar A, Krishna R, Olitsky SE. Comparison of the Icare rebound tonometry with the Goldmann applanation tonometry in a pediatric population. J AAPOS. 2015;19:572–4.
Uzlu D, Akyol N, Türk A, Oruç Y. A comparison of three different tonometric methods in the measurement of intraocular pressure in the pediatric age group. Int Ophthalmol. 2020;40:1999–2005.
Author information
Authors and Affiliations
Contributions
IRM was responsible for writing the protocol, conducting the literature search, screening and examining potentially eligible subjects, recording data in an excel sheet, analysing data, interpreting results, creating preliminary tables and figures and writing the preliminary manuscript. RRK was responsible for designing the research idea and protocol, writing the protocol, further analysing data and interpreting results, updating reference lists, modifying tables and figures, conducting the meta-analysis and writing the final manuscript. NAE and DHK were responsible for writing the protocol, correcting and modifying the preliminary manuscript, further analysing data and interpreting results and providing feedback on the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Moussa, I.R., Kassem, R.R., Edris, N.A. et al. Normal intraocular pressure in Egyptian children and meta-analysis. Eye 36, 1266–1273 (2022). https://doi.org/10.1038/s41433-021-01633-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01633-8