Abstract
Purpose
To investigate the geographic variation in the cumulative incidence of private cataract surgery (PCS) and its association with remoteness, socioeconomic, and private health insurance coverage indexes in a large Australian population.
Methods
A prospective population-based study of 266,896 Australian adults living in New South Wales (NSW) aged 45 years older and over were enrolled in the 45 and Up Study. PCS was identified using Medicare claims data. Participants were assigned to a Statistical Area Level 3 (SA3) based on residential postcode in NSW. Cumulative incidence of PCS (number of surgery per 100,000 population from 2006 to 2016) among 89 SA3s was calculated and standardized to the baseline population. Remoteness and socioeconomic deprivation was derived from Australian Bureau of Statistics (ABS). Private health insurance coverage rates were obtained from the baseline interview.
Results
A total of 257,237 participants with complete data were included in the current analysis. During the study period, a total of 67,707 cataract surgeries were performed among 39,744 participants. Cumulative incidence of PCS varied from 14,897 to 37,314 per 100,000 across 89 SA3s. Multivariable adjusted regression models showed that remoteness index and private health insurance coverage rates were independently associated with cumulative incidence of PCS (all P < 0.05), while no significant association between socioeconomic deprivation and cumulative incidence of PCS was observed. Collectively, these three variables explained 52.7% of the geographic variability.
Conclusions
The geographical variation in the cumulative incidence of PCS calls for interventions targeted at individuals living in remote areas to reduce the burden of cataract-related vision impairment.
Similar content being viewed by others
Introduction
Cataract remains one of the leading causes of visual impairment and blindness, posing a significant public health burden and substantial impacts to the global economy [1]. The effects of visual impairment from cataract can lead to elevated risk of falls and bone fractures [2], accidents [3], depression [4], and mortality [5, 6].
Cataract surgery is currently the only effective intervention and has become the most frequently performed surgical procedure in Australia [7]. The volume of cataract surgery has increased globally in recent decades, with an average annual burden of over US$573 million [8, 9]. The Australian healthcare system is comprised of two models of care: a public and a private system. The cost of cataract surgery as a public patient is covered by Medicare and waiting time for surgery is based on disease severity [10, 11]. Moreover, patients can also choose to have surgery in a private facility with a portion of the cost covered by Medicare and an out-of-pocket expense paid by the patient. These out of pocket expenses can vary depending on the level of private health cover and the fee set by the chosen surgeon. In Australia, the private sector plays a crucial role in cataract management with over 70% of cataract surgeries performed in private settings [10]. As the population continues to age, the prevalence of cataract is estimated to increase dramatically and private settings will play an even more significant role in the timely delivery of cataract care to minimize the burden of disease.
Previous research has examined geographic distribution in cataract surgery in America [12], UK [13], and Canada [14]. However, little is known about the geographic variation in cataract surgery in Australia. One study conducted in New South Wales (NSW), Australia investigated variation in rates of cataract surgery by area of residence for Aboriginal and non-Aboriginal adults rather than a standardized regional breakup of Australia [15]. Additionally, whether cataract surgery rates in Australia differs based on remoteness index, socioeconomic status, or private health insurance coverage is still unclear. This information has the potential to be valuable for policymakers to optimally allocate resources.
Therefore, the primary aim of this study is to explore the geographic variation in the cumulative incidence of private cataract surgery (PCS) in NSW, Australia using Statistical Area Level 3 (SA3) data from a large cohort study of middle age and older Australians. The secondary aim is to assess whether the geographic variation is correlated with remoteness, socioeconomic deprivation, and private health insurance coverage index.
Methods
Data source
The Sax Institute’s 45 and Up Study is a large-scale Australian cohort study of 266,896 men and women aged 45 and over, randomly sampled from the Department of Human Services (formerly Medicare Australia) enrollment database who were invited by mail to be a part of the study. People 80+ years of age and residents of rural and remote areas were intentionally over-sampled. The database is a national health care database which includes all citizens and permanent residents of Australia and some temporary residents and refugees. The overall response rate was estimated to be 18% and ~11% of the entire NSW population aged 45 years or older were included in the final sample. Individuals joined the study by completing a postal questionnaire (distributed from January 2006 to December 2009) and providing informed consent for follow-up through repeated data collection and linkage of their data to national health databases. The methods of the 45 and Up Study have been described in details elsewhere [16].
The baseline questionnaire data from study participants were linked to the Medicare Benefits Schedule (MBS). The MBS database includes data on all operative procedures performed in the private system for which a Medicare rebate was claimed. Rebates are not claimed for services provided within the public system as public hospitals receive funding from the governments, therefore, participants who underwent cataract surgery within the public system cannot be identified using the MBS database. Ethical approval for the 45 and Up Study was granted by the University of NSW Human Research Ethics Committee. Ethics approval for this study was granted by the Royal Victorian Eye and Ear Hospital Human Research Ethics Committee.
Geographic areas
Geographic areas are defined in the Australian Statistical Geography Standard (ASGS) developed in 2011, which is used to disseminate social, demographic, and economic statistics based on the concept of a functional area [17]. ASGS consists of six hierarchical levels; each level aggregates to the level above and the component units at each level cover the whole of Geographic Australia without gaps or overlaps. For this study, we chose SA3s as the hierarchy unit for analysis as these provided a standardized regional breakup of Australia. The aim of having SA3s is to create a standard framework for the analysis of Australian Bureau of Statistics (ABS) data at the regional level through clustering groups of SA2s that have similar regional characteristics. Each individual was assigned to an SA3 based on his or her residential postcode. A total of 89 SA3s were identified for the present analysis.
Identification of PCS
Cataract surgeries in private facilities were identified based on the following MBS item numbers: 42698, 42701, 42702, and 42716 during the period of 2006 to 2016. In each SA3, we calculated age- and sex-standardized cumulative incidence of PCS (surgery times per 100,000 from 2006 to 2016) by SA3 using a direct standardization technique to the baseline 45 and Up Study population in 5-year age and sex groups.
Accessibility/remoteness index of Australia (ARIA)
The ARIA is a standard index of remoteness and accessibility to service centers in Australia and was developed by the Australian government in 1999 [18]. Geographical areas are given a standardized score (continuous from 0 to 15) based on the road distance to service towns of different sizes. Scores for regions are derived by averaging scores of a 1 km2 grid. The index scores can be classified into major cities (ARIA score: 0–0.20), inner regional (0.20–2.40), outer regional (2.40–5.92), and remote (5.92–15) areas.
Socioeconomic indexes for areas (SEIFA)
The ABS has developed the SEIFA to allow measurement of relative socioeconomic status at a small geographic area level. These indexes include relative socioeconomic advantage and disadvantage (IRSAD), relative socioeconomic disadvantage (IRSD), education and occupation (IEO), and economic resources (IER) [19]. It summarizes a range of socioeconomic variables associated with advantage and disadvantage such as the proportion of families with high incomes, people with tertiary education and employees in skilled occupations. Low values indicate areas that are relatively disadvantaged, and high values indicate areas that are relatively advantaged. In the current analysis, we used the median IRSAD value in each SA3 to represent the socioeconomic level given its strongest relationship with outcome.
Private health insurance coverage rate
Private health insurance coverage rate was obtained from responses provided during the baseline interview. Health insurance categories included private with extras, private with no extras, veterans’ card (white or gold), health care concession card, and others. Private health insurance coverage rate was defined as the rate of participants who held private health insurance with or without extras.
Statistical analysis
All statistical analysis was performed using Stata (version 12.0; StataCorp, College Station, TX). Scatter plots were used to demonstrate substantial variation in the cumulative incidence of PCS across the SA3s, remoteness, socioeconomic deprivation, and private health insurance coverage index. Associations between remoteness, socioeconomic deprivation and private insurance coverage index, and cumulative incidence of PCS were assessed using univariate linear regression models. Covariates significantly associated with cumulative incidence of PCS were added to multivariable linear regression models. Statistical significance was defined as a P value of <0.05.
Results
Of the 266,896 eligible participants at baseline, 7061 with incomplete registry data such as unknown postcode (4955), socioeconomic index (2106), and cataract surgery before January 1, 2006 (2598) were excluded from the study, thus yielding 257,237 participants in the analysis. Between 2006 and 2016, a total of 67,707 cataract surgeries were performed across 39,744 participants. Table 1 illustrates the socioeconomic and private insurance coverage characteristics of SA3s with the five highest and five lowest rates for the cumulative incidence of PCS.
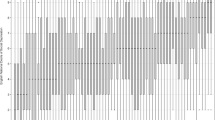
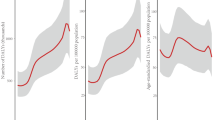
The scale of geographic variation of cumulative incidence of PCS by SA3 can be seen in Fig. 1. SA3s showed a wide variation in the cumulative incidence of PCS, ranging from 14,897 to 37,314 surgery times per 100,000. Variation was up to 2.5 times higher when comparing the highest and lowest rates of cataract surgery. Figure 2 presents the cumulative incidence of PCS by SA3s index of remoteness. Major city areas have the highest cumulative incidence of PCS (28,225 surgery times per 100,000), while the lowest cumulative incidence of PCS was observed in outer regional (21,126 surgery times per 100,000) and remote areas (21,409 surgery times per 100,000). Figure 3 shows the cumulative incidence of PCS over the area’s IRSAD. In general, the higher the IRSAD score in an SA3 area, the higher the cumulative incidence of PCS. The cumulative incidence of PCS by SA3 showed a positive correlation with the IRSAD score (R2 = 0.38). A similar result was observed for private insurance coverage rates (R2 = 0.45; Fig. 3).
The cumulative incidence of private cataract surgery by SA3 shows a positive correlation with the index of relative socioeconomic advantage and disadvantage (R2 = 0.38) and private health insurance coverage rates (R2 = 0.45). Each point represents an SA3. The solid line represents the fitted line and shaded areas represents 95% confidence intervals.
In univariable linear regression models, remoteness index, socioeconomic deprivation, and private health insurance coverage were significantly associated with cumulative incidence of PCS, respectively (all P values < 0.05, Table 2). After adjusting for these covariates, the multivariable adjusted model showed that remoteness index and private health insurance coverage rates were independently associated with the cumulative incidence of PCS (all P < 0.05), while the significant positive association between socioeconomic deprivation and cumulative incidence of PCS diminished after multiple adjustments (P = 0.192). Collectively, these three covariates explained 52.7% of geographic variability in the cumulative incidence of PCS (R2 = 0.527).
Discussion
In this large analysis of an Australian population, we found a wide geographical variation in the cumulative incidence of PCS. Moreover, we also found that lower cumulative incidence of PCS existed in more remote areas when compared to major city areas. Greater private health insurance coverage rate was associated with the higher cumulative incidence of PCS. These results suggest that interventions targeted at individuals living in remote and disadvantaged areas are required to increase the cumulative incidence of PCS and reduce the burden of cataract-related vision impairment.
We found a difference of more than double between the lowest (Broken Hill and Far West) and highest (Newcastle) cumulative incidence of PCS. It is unclear why this SA3 has such high cumulative incidence of PCS, possibly due to higher service provider density and several patient’s factors (e.g., visual demands and motivation for surgery), eye care policy-related factors (e.g., promotion of cataract surgery), and environmental factors specific to that particular SA3 (e.g., UV exposures, smoking rates). Although a considerable geographic variation in cataract surgery was observed in America [12], UK [13], and Canada [14], differences in study design, cataract surgery definition (public or public and PCS), and health insurance systems make direct comparisons difficult. However, these studies all stressed the importance of varied access and private surgery settings on the wide variation in cataract surgery rates. According to a recent Australian statistic, over 70% of cataract patients had their surgeries in private facilities [10]. The shorter median waiting time, more flexible choices of surgeons and hospitals, and availability of bilateral cataract operations within 1 month have attributed to the dominant preference for private facilities to conduct cataract surgery in Australia [17].
Our multivariable model considering index of remoteness, socioeconomic deprivation, and private insurance coverage found a significant gradient decrease in the cumulative incidence of PCS in more remote areas, ranging from 21,126 surgery times per 100,000 in outer regional areas to 28,225 surgery times per 100,000 in major city areas. It was not surprising that when the residential distance from a large urban area increased, the density of private hospitals and access to private health care might decrease and this would impact on privately operated cataract surgeries. We also found the significantly lower cumulative incidence of PCS in areas with lower private health insurance coverage rates in the multivariable adjusted model. A reduced out-of-pocket payment for cataract surgery could have the potential to drive cataract patients to undergo surgery in private settings. After multiple adjustments, the socioeconomic deprivation was no longer significantly associated with the cumulative incidence of PCS in SA3s. The similar levels of cumulative incidence of PCS for those with disadvantaged socioeconomic status compared with those with more advantaged socioeconomic status likely reflect concerted efforts to improve access to private eye care services in disadvantaged participants in NSW (e.g., private–public partnership clinics) [18]. Of note, these three covariates collectively explained 52.7% of geographic variation in the cumulative incidence of PCS, other factors, such as UV light exposure, education, employment, number of ophthalmologist or optometrist, and lifestyle factors among different SA3s may also explain the geographic variation in the cumulative incidence of PCS. Further studies are needed to investigate the potential causes for this geographic variation.
A major strength of this study is the large sample size which enabled comparison of surgery rates among various SA3s. The use of Medicare standardized item codes reduces the potential for coding errors across different systems. However, there are several limitations. Firstly, we did not have access to clinical information such as visual acuity threshold for cataract surgery, cataract severity, and visual needs of patients. These variables may affect the volume and the timing of performing cataract surgery. Secondly, the participants’ statistical areas of residence were based on the baseline questionnaire and we could not account for participants who may have moved away or died during the study period. Thirdly, we did not have information on aboriginal status which is likely to contribute to the variation of cataract surgery rates based on previous studies [15]. Fourthly, the availability of public cataract surgery might affect geographical variation in the cumulative incidence of PCS. Nevertheless, private settings have played a significant role in the timely delivery of cataract care to minimize the burden in Australia, as a recent statistic shows that over 70% of cataract patients had their surgeries in private facilities. Therefore, the effects of the variation of the public cataract surgery on our findings may be trivial. Last but not the least, the participation rate of 18%, and known sample biases (e.g., under-representation of CALD persons) means that great care should be taken if generalizing these results to the general population.
In conclusion, a considerable geographical variation in the cumulative incidence of PCS and its correlation with remoteness index and private health insurance coverage indicate that interventions targeted at individuals living in remote and disadvantaged areas are required to help reduce the burden of cataract-related visual impairment in NSW, Australia.
Summary
What was known before
-
Previous research has reported a wide geographic variation in cataract surgery in America, UK, and Canada. While little is known about the geographic distribution in cataract surgery in Australia.
What this study adds
-
A wide geographical variation in the cumulative incidence of private cataract surgery (PCS) was observed in an Australian population.
-
Cumulative incidence of PCS was significantly correlated with remoteness index and private health insurance coverage.
References
Thorburn R, Roland M. The effectiveness of preschool vision screening by health visitors. Br J Community Nurs. 2000;5:41–4.
Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol. 2005;89:53–9.
Meuleners LB, Hendrie D, Lee AH, Ng JQ, Morlet N. The effectiveness of cataract surgery in reducing motor vehicle crashes: a whole population study using linked data. Ophthalmic Epidemiol. 2012;19:23–8.
McCusker S, Koola MM. Association of ophthalmologic disorders and depression in the elderly: a review of the literature. Prim Care Companion CNS Disord. 2015;17. https://doi.org/10.4088/PCC.14r01731.
Wang JJ, Mitchell P, Simpson JM, Cumming RG, Smith W. Visual impairment, age-related cataract, and mortality. Arch Ophthalmol. 2001;119:1186–90.
Zhu Z, Wang L, Young CA, Huang S, Chang BH, He M. Cataract-related visual impairment corrected by cataract surgery and 10-year mortality: the Liwan Eye Study. Investigative Ophthalmol Vis Sci. 2016;57:2290–5.
Brian G, Taylor H. Cataract blindness-challenges for the 21st century. Bull World Health Organ. 2001;79:249–56.
Armstrong KL, Jovic M, Vo-Phuoc JL, Thorpe JG, Doolan BL. The global cost of eliminating avoidable blindness. Indian J Ophthalmol. 2012;60:475–80.
Klein BE, Howard KP, Lee KE, Klein R. Changing incidence of lens extraction over 20 years: the Beaver Dam eye study. Ophthalmology. 2014;121:5–9.
Curtis AJ, Russell CO, Stoelwinder JU, McNeil JJ. Waiting lists and elective surgery: ordering the queue. Med J Aust. 2010;192:217–20.
Yi Q, Flanagan SJ, McCarty DJ. Trends in health service delivery for cataract surgery at a large Australian ophthalmic hospital. Clin Exp Ophthalmol. 2001;29:291–5.
Kauh CY, Blachley TS, Lichter PR, Lee PP, Stein JD. Geographic variation in the rate and timing of cataract surgery among US communities. JAMA Ophthalmol. 2016;134:267–76.
Keenan T, Rosen P, Yeates D, Goldacre M. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Br J Ophthalmol. 2007;91:901–4.
Hatch WV, Cernat G, Singer S, Bell CM. A 10-year population-based cohort analysis of cataract surgery rates in Ontario. Can J Ophthalmol. 2007;42:552–6.
Randall DA, Reinten T, Maher L, Lujic S, Stewart J, Keay L, et al. Disparities in cataract surgery between Aboriginal and non-Aboriginal people in New South Wales, Australia. Clin Exp Ophthalmol. 2014;42:629–36.
Up Study C, Banks E, Redman S, Jorm L, Armstrong B, Bauman A, et al. Cohort profile: the 45 and up study. Int J Epidemiol. 2008;37:941–7.
Doyle M. Assocaite professor in orthoptics. Australian Orthoptic Journal. 1991;27:iv.
Health and Care Professions Coucil (HCPC). Standards of proficiency: Orthoptists. London; 2013.
Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011.
Acknowledgements
This research was completed using data collected through the 45 and Up Study (www.saxinstitute.org.au). The 45 and Up Study is managed by the Sax Institute in collaboration with major partner Cancer Council NSW; and partners: the National Heart Foundation of Australia (NSW Division); NSW Ministry of Health; NSW Government Family & Community Services–Ageing, Carers and the Disability Council NSW; and the Australian Red Cross Blood Service. We thank the many thousands of people participating in the 45 and Up Study. Pharmaceutical Benefits Scheme (PBS) and Medicare Benefits Schedule (MBS) data were provided by the Australian Government Department of Human Services.
Funding
Professor Mingguang He receives support from the University of Melbourne at Research Accelerator Program and the CERA Foundation. The Centre for Eye Research Australia (CERA) receives Operational Infrastructure Support from the Victorian State Government. This project is funded by the Australia China Research Accelerator Program at CERA. Professor Mingguang He is also supported by the Fundamental Research Funds of the State Key Laboratory of Ophthalmology, National Natural Science Foundation of China (81420108008). Dr Zhuoting Zhu is supported by the Research Foundation of Medical Science and Technology of Guangdong Province (B2021237). The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Z.Z. and L.L. conceptualized and designed the study with L.Z. and M.H. Z.Z. and L.L. did the literature search and wrote the first draft of the manuscript. Z.Z., L.L., X.S. and W.W. did the statistical analysis. W.W., L.Z., and M.H. had full access to all of the data. All authors commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhu, Z., Li, L., Scheetz, J. et al. Geographic variation in cumulative incidence of private cataract surgery in Australia and its influencing factors: Findings from the 45 and Up Study. Eye 36, 1767–1771 (2022). https://doi.org/10.1038/s41433-021-01630-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01630-x
This article is cited by
-
A longitudinal analysis of factors associated with age-related cataract among older Australian women: a cohort study of 7851 older Australian women 79–90 years
Irish Journal of Medical Science (1971 -) (2023)
-
Application of Andersen–Newman model to assess cataract surgery uptake among older Australian women: findings from the Australian Longitudinal Study on Women’s Health (ALSWH)
Aging Clinical and Experimental Research (2022)