Abstract
Purpose
To determine difference in surgically induced astigmatism (SIA), post-operative intraocular pressure (IOP) and axial length (AL) between single site and twin-site phacotrabeculectomy augmented with Mitomycin C (MMC).
Design
Prospective interventional randomised controlled study.
Methods
In a prospective interventional comparative study, eligible patients were scheduled for phacotrabeculectomy. They were randomised to either group A: single site or group B: twin-site phacotrabeculectomy with MMC 0.2 mg/mL. Axial length was measured by using Zeiss IOL master I, pre-operatively and at 1, 3, 6 and 12 months post-operatively. Corneal topography was performed using Bausch and Lomb Orbscan I pre-operatively and at 3, 6 and 12 months post-operatively to analyse surgically induced astigmatism. Vector analysis was used to analyse the surgically induced astigmatism.
Results
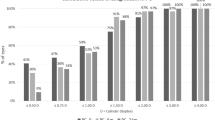
One hundred and eight eyes of which 55 patients in group A, and 53 patients in group B were enroled for vector analysis. The mean preoperative astigmatic vector power was +0.89 ± 0.4 D and +0.97 ± 0.5 D in group A and B respectively. The mean post-operative astigmatic vector power was +0.78 ± 0.4 D in group A and +0.96 ± 0.5 D in group B at the end of 12 months. Corneal topography showed post-operative superior flattening (51.8% at 3 months and 55.4% at 12 months) in group A (P = 0.072) compared to superior steepening (59.6% at 3 months and 61.5% at 12 months) in group B (P = 0.977).
Conclusions
The two commonly used techniques of combined cataract and glaucoma surgery proved to be efficacious without significant difference in surgical induced astigmatism.
Similar content being viewed by others
Introduction
As our elderly population is increasing, the simultaneous presence of cataract and glaucoma is also increasing. Phacotrabeculectomy is the preferred technique for combined cataract and glaucoma surgery [1, 2]. It can be done either via a single site incision for both the procedures or a twin-site incision i.e. two separate incisions for each of the procedure [3]. However, the decision to perform phacotrabeculectomy through one site or two site remains controversial. Some studies have shown that there is no significant difference in intraocular pressure (IOP) control with both the techniques [4].
It has been suggested that single-site phacotrabeculectomy may result in increased trauma to the wound resulting in poorer filtration, indicating a possible benefit of separating the incisions in two-site phacotrabeculectomy [5].
However delayed wound healing after trabeculectomy has significant influence on corneal curvature and axial length (AL) caused by persistent surgical wound effect. Previous reports have also shown that there is induced corneal astigmatism after trabeculectomy and combined operation with various surgical techniques [6,7,8,9,10,11,12]. According to an evidence based review of the surgical techniques and adjuvant used in combined operation, the strongest evidence of efficacy exists for using mitomycin C (MMC), separating the incisions for cataract and glaucoma surgery, and removing the nucleus by phacoemulsification [13].
Surgically induced astigmatism (SIA) is an important factor as it not only influences the quality of vision but also the visual rehabilitation after surgery [3]. Astigmatism that is induced by the single site and twin-site procedure is different as the incision site for cataract removal alters the corneal curvature [14]. Previous studies have shown lesser SIA and better IOP control in case of twin-site surgery [15].
The purpose of this study was to determine difference in SIA, post-operative IOP and AL between single site and twin-site phacotrabeculectomy augmented with MMC.
Methods
This is a prospective interventional randomised study conducted on 110 eyes of 110 patients. This study was performed between November 2010 and October 2011. This study was approved by the Institutional Review Board. Informed consent was obtained. All procedures conformed to the guidelines of the Declaration of Helsinki.
Patient enrolment and treatment assignment
A pilot study of sample 20 (10 per group) was conducted to compare the magnitude of SIA of single site and twin-site combined surgeries. Based on the pilot study estimation, we attained a sample size n = 110 (55 per group). Standard deviation of two groups IOP were 3.42 and 2.52 with mean difference of 1.6 were taken as reference with power 80% and level of significance 5%. Inclusion criteria were patients with visually significant cataract in patients with medically uncontrolled primary open-angle glaucoma (POAG), or not tolerating medical therapy, and primary angle closure glaucoma (PACG) and pseudoexfoliation glaucoma (PxfG). Cases with previous ocular surgery, corneal opacity, previous Argon Laser Trabeculoplasty or Selective Laser Trabeculoplasty, secondary glaucoma, subluxated or mature or hypermature cataract, age related maculopathy and diabetic maculopathy were excluded from study.
The enroled patients were randomly allocated using computer-generated numbers to either group A or B where they underwent single-site (group A) or twin-site phacotrabeculectomy (group B). The post-operative data outcome of 1 year was analysed.
Surgical technique
Phacotrabeculectomy was performed under peri-bulbar anaesthesia with a superior fornix‑based conjunctival flap by a single surgeon. All cases received subconjunctival MMC 0.2 mg/ml soaked Weck-cel sponge (~2 mm × 2 mm) for 2 min followed by irrigation with 30 ml of balanced salt solution. A 4 × 4 mm triangular scleral flap was made for all surgeries. In single‑site surgery, phacoemulsification was performed by anterior chamber (AC) entry with a 2.8 mm keratome under the triangular scleral flap. In the twin‑site procedure, phacoemulsification with a foldable in‑the‑bag IOL (AcrySof SN60WF, Alcon, Inc., Hünenberg, Switzerland) implantation was completed through a temporal 2.8 mm clear corneal incision and closed with a single 10‑0 nylon suture. A 2 × 2 mm deep block was excised using Kelly’s punch followed by peripheral iridectomy. The viscoelastic was thoroughly washed and the scleral flap was closed with three 10-0 nylon sutures. The conjunctiva was closed with 8‑0 polyglactin suture.
Post-operative regime was topical antibiotic for 4 weeks, topical cycloplegic for 4 weeks and topical prednisolone acetate 1% tapered over 6–8 weeks. All patients were followed up on post-op day 1, 2 weeks, 1 month, 3 months, 6 months, 12 months and additional evaluations as needed.
Data collection
Preoperative data included demographics and clinical details of glaucoma. Comprehensive ocular examination was conducted pre-operatively and at each post-operative visit. Data collection included subjective refraction, best‑corrected Log MAR visual acuity (BCVA), corneal topography (Bausch and Lomb Orbscan I), IOP (Goldmann applanation tonometer), AL (Zeiss IOL Master I) and corneal endothelial cell count (ECE) was calculated using noncontact specular microscope (SP 3000P Topcon, Tokyo, Japan). Use of anti-glaucoma medications and complications if any were recorded. One optometrist obtained topography measurements pre-operatively and after 3, 6 and at 12 months post-operatively. Simulated K-values of corneal topography were used to analyse surgically induced topographic astigmatism.
Statistical and vector analysis
All statistical analyses were performed with STATA 11.1 (Texas, USA). Mean (SD) and frequency (%) were given to describe the summary data. Categorical variables were compared by chi squared test. Paired t test/Wilcoxon signed rank test was used to test the mean difference between preoperative and post-operative values in the ocular parameters. Student’s t test/Mann–Whitney test was used to test the mean difference between one site and two site in ocular parameters. P values < 0.05 was considered as statistically significant. Vector analysis was done by SIA calculator version 2.1© 2010.
Results
A total of 108 eyes of 108 patients met the inclusion and exclusion criteria. Two patients were lost to follow up. A total of 55 (50.9%) and 53 (49.1%) eyes had undergone one-site and two-site surgeries respectively. There were 25 eyes with POAG, 21 eyes with PACG and 9 eyes with PXFG in the single-site group and 25 eyes with POAG, 20 eyes with PACG and 8 eyes with PXFG in the twin-site group, (P = 0.98). The median age at surgery was 60 years in the single-site group and 59 years in the twin-site group (P = 0.79).
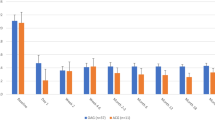
The preoperative IOP ranged from 13 to 40 mm of Hg in the single-site group with a median of 23.14 ± 5.69 mm of Hg, whereas in the twin-site group the IOP ranged from 15 to 41 mmHg with a median of 22.36 ± 5.15 mm of Hg. Post-operative IOP was followed up for 12 months, at which point the IOP ranged from 7 to 24 mmHg in single-site group with a median of 10.85 ± 3.57 mm of Hg, whereas in the twin-site group the IOP ranged from 7 to 17 mmHg with a median of 10.66 ± 2.34 mm of Hg which was statistically significant in both group with P < 0.0001.
The preoperative and post-operative (12 months) astigmatic vector powers are shown in Fig. 1 and the changes in astigmatic vector powers in either group are shown in Tables 1, 2 and 3. Comparing preoperative and post-operative astigmatic vector powers, using Wilcoxon signed rank test, outcomes were statistically significant in the single-site group (P = 0.018) and not significant in twin-site group (P = 0.942) at 12 months. The mean change in astigmatic vector power between either group, using Mann–Whitney test, was statistically significant with P = 0.032.
We also studied effect of either surgery causing corneal steepening, flattening or irregular corneal curvature (Table 4). Corneal steepening was defined as increase in the SimK max by 0.5 D or more; while flattening was defined as decrease in the SimK max by 0.5 D or more. Astigmatism was said to be irregular when the corneal curvature was not uniform on topography and changed from point to point. Corneal topography showed post-operative superior flattening in 54.5%, 58.2% at 3 and 12 months, respectively in the single-site group (P = 0.072) and post-operative superior steepening in 60.3%, 64.1% at 3 and 12 months, respectively in the twin-site group (P = 0.977). The difference in topographical changes was statistically not significant when comparing the 3 months and 12 months change in curvature in both the groups.
AL in single-site group was 23.02 ± 1.51 mm pre-operatively and 22.99 ± 1.51 mm at 12 months post-operatively. In the twin-site group the AL was 22.85 ± 1.39 mm pre-operatively to 22.82 ± 1.39 mm at 12 months post-operatively. In both groups, the reduction was statistically significant (P < 0.0001).
The mean BCVA pre-operatively was 0.63 ± 0.38 log MAR in the single-site group and 0.64 ± 0.41 log MAR in the twin-site group and post-operatively mean BCVA was 0.04 ± 0.09 log MAR in the single-site group and 0.02 ± 0.06 log MAR in the twin-site group which was statistically significant in both the groups with P < 0.0001 and thus inferring the effectiveness of these surgical procedures in improving the visual acuity.
The mean preoperative ECE was 2367.18 ± 314.04 cells/mm2 in the single-site group and 2262.45 ± 238.88 cells/mm2 in the twin-site group and post-operatively at 12 months 2070.45 ± 280 cells/mm2 in single-site group and 1924.89 ± 201.39 cells/mm2 in the twin-site group which was statistically significant in both the groups with P < 0.0001.
Post-operatively, anti-glaucoma medications were started in five cases of the single-site group as compared to four cases of the twin-site group. Post-operatively in the single-site group, two cases had hypotony and shallow AC each while in the twin-site group, one case had hypotony and shallow AC each, all of which were managed conservatively.
Discussion
This prospective study objectively compared SIA following single‑site and twin‑site phacotrabeculectomy at twelve months after surgery. We used vector analysis and compared both the magnitude and direction of astigmatism before and after surgery within the groups. The combined approach provides good IOP control as well as improved best corrected visual acuity when compared with preoperative vision [16,17,18,19,20,21,22,23]. SIA in different studies showed different patterns following combined phacotrabeculectomy. Various studies described that corneal topographic changes in few patients can last about 12 months, others described that the induced changes disappear in 6–12 months post-operatively [9, 24].
Rosen et al. and Claridge et al. who studied the corneal topographic changes following trabeculectomy found superior corneal steepening and with the rule shift in astigmatism. They reported that the main change of astigmatic vector was 1.25 ± 0.8 D by 6 months in the vertical meridian [8, 9]. They proposed that this may arise from tissue contraction around the trabeculectomy site as a result of extensive scleral cautery and from overtight scleral flap sutures. As opposed to the study done by Rosen et al. the use of minimal scleral cautery and application of sutures with minimal but adequate tension to the superior scleral flap in both our study group may be a factor causing the superior flattening in single-site group and more steepening in twin-site group.
Zarnowski et al. described [25] post operative against the rule astigmatism of 1.1 D with trabeculectomy when MMC was used. Our single-site group needed a 2.8 mm superior corneal incision, leading to superior flattening and the twin-site group required a temporal 2.8 mm clear corneal incision leading to with the rule shift (superior steepening) due to coupling effect.
Egrilmez et al. compared post-operative induced astigmatism in trabeculectomy versus nonpenetrating glaucoma surgeries on a much smaller number of subjects compared with our study [26]. They concluded that despite larger flap size and larger surgical area, nonpenetrating trabecular surgeries induced less against the rule astigmatism than tarbeculectomy. This was in agreement with findings in our study that there were more frequent flatter corneas along the vertical meridian with one-site phacotrabeculectomy when compared with two-site phacotrabeculectomy which induced more steeper corneas along the vertical meridian.
Both techniques of combined cataract and glaucoma surgery proved to be efficient and safe procedures. The improvement in BCVA and reduction in IOP did not differ significantly between the single-site and twin-site approach. But there was a significant difference between the techniques in terms of ECE, the two-site approach showing greater reduction in ECE over time. There was no significant difference between the two techniques in terms of CCT and AL over time, but the minimal reduction in AL in both groups proved to be highly significant post operatively. Our data was comparable with the results of previous studies comparing single‑site and twin‑site phacotrabeculectomies.
We studied the two techniques over a short period of time (12 months), thus proving to be a limitation. Hence a larger time frame is required in order to clearly come to conclusion regarding safety and efficacy of the two surgical procedures.
In conclusion, both the two commonly used techniques of combined cataract and glaucoma surgery proved to be efficacious without significant difference in surgical induced astigmatism. There was no difference in IOP reduction between single‑site and twin‑site techniques. No added advantage is obtained by separating the two sites of incision and the surgeon can choose either technique according to one’s ‘skill and comfort’ level.
Summary
What was known before
-
Phacotrabeculectomy leads to surgical induced astigmatism.
What this study adds
-
With-the-rule astigmatism may benefit with the single-site phacotrabeculectomy approach.
-
Against-the-rule astigmatism would benefit from the twin-site phacotrabeculectomy approach.
References
Shingleton BJ, Price RS, O’Donoghue MW, Goyal S. Comparison of 1‑site versus 2‑site phacotrabeculectomy. J Cataract Refract Surg. 2006;32:799–802.
el Sayyad F, Helal M, el‑Maghraby A, Khalil M, el‑Hamzawey H. One‑site versus 2‑site phacotrabeculectomy: a randomized study. J Cataract Refract Surg. 1999;25:77–82.
Wang L, Shirayama M, Ma XJ, Kohnen T, Koch DD. Optimizing intraocular lens power calculations in eyes with axial lengths above 25.0 mm. J Cataract Refract Surg. 2011;37:2018–27.
Buys YM, Chipman ML, Zack B, Rootman DS, Slomovic AR, Trope GE. Prospective randomized comparison of one‑ versus two‑site Phacotrabeculectomy two‑year results. Ophthalmology. 2008;115:1130–3.e1.
Vass C, Menapace R. Surgical strategies in patients with combined cataract and glaucoma. Curr Opin Ophthalmol. 2004;15:61–6.
Kook MS, Kim HB, Lee SU. Short-term effect of mitomycin-C augmented trabeculectomy on axial length and corneal astigmatism. J Cataract Refract Surg. 2001;27:518–23.
Hugkulstone CE. Changes in keratometry following trabeculectomy. Br J Ophthalmol. 1991;75:217–8.
Rosen WJ, Mannis MJ, Brandt JD. The effect of trabeculectomy on corneal topography. Ophthalmic Surg. 1992;23:395–8.
Claridge KG, Galbraith JK, Karmel V, Bates AK. The effect of trabeculectomy on refraction, keratometry and corneal topography. Eye. 1995;9:292–8.
Vernon SA, Zambarakji HJ, Potgieter F, Evans J, Chell P. Topographic and keratometric astigmatism up to 1 year following small flap trabeculectomy (microtrabeculectomy). Br J Ophthalmol. 1999;83:779–82.
Hong YJ, Choe CM, Lee YG, Chung HS, Kim HK. The effect of mitomycin-C on postoperative corneal astigmatism in trabeculectomy and a triple procedure. Ophthalmic Surg Lasers. 1998;29:484–9.
Gayton JL, Van der Karr MA, Sanders V. Combined cataract and glaucoma procedures using temporal cataract surgery. J Cataract Refract Surg. 1996;22:1485–91.
Jampel HD, Friedman DS, Lubomski LH, Kempen JH, Quigley H, Congdon N, et al. Effect of technique on intraocular pressure after combined cataract and glaucoma surgery: an evidence-based review. Ophthalmology. 2002;109:2215–24.
Şimşek Ş, Yaşar T, Demirok A, Çinal A, Yilmaz ÖF. Effect of superior and temporal clear corneal incisions on astigmatism after sutureless phacoemulsification. J Cataract Refract Surg. 1998;24:515–8.
Rossetti L, Bucci L, Miglior S, Orzalesi N. Temporal corneal phacoemulsification combined with separate‑incision superior trabeculectomy vs standard phacotrabeculectomy. A comparative study. Acta Ophthalmol Scand Suppl. 1997:39.
Lyle WA, Jin JC. Comparison of a 3- and 6-mm incision in combined phacoemulsification and trabeculectomy. Am J Ophthalmol. 1991;111:189–96.
Wedrich A, Menapace R, Radax U, Papapanos P, Amon M. Combined small-incision cataract surgery and trabeculectomy: technique and results. Int Ophthalmol. 1992;16:409–14.
Allan BD, Barrett GD. Combined small incision phacoemulsification and trabeculectomy. J Cataract Refract Surg. 1993;19:97–102.
O’Grady JM, Juzych MS, Shin DH, Lemon LC, Swendris RP. Trabeculectomy, phacoemulsification, and posterior chamber lens implantation with and without 5fluorouracil. Am J Ophthalmol. 1993;116:594–9.
Munden PM, Alward WLM. Combined phacoemulsification, posterior chamber intraocular lens implantation, and trabeculectomy with mitomycin C. Am J Ophthalmol. 1995;119:20–9.
Wedrich A, Menapace R, Radas U, Papanos P. Long-term results of combined trabeculectomy and small incision cataract surgery. J Cataract Refract Surg. 1995;21:49–54.
Ruderman JM, Fundingsland B, Meyer MA. Combined phacoemulsihcation and trabeculectomy with mitomycin C. J Cataract Refract Surg. 1996;22:1–6.
Buys YM, Chipman ML, Zack B, Rootman DS, Slomovic AR, Trope GE. Prospective randomized comparison of one- versus two-site phacotrabeculectomy two-year results. Ophthalmology. 2008;115:1130–3.
Hornova´ J. Trabeculectomy with releasable sutures and corneal topography. Cesk Slov Oftalmol. 1998;54:368–72.
Zarnowski T, Haszcz D, Rakowska E, Zagorski Z. Corneal astigmatism after trabeculectomy. Klin Ocz. 1997;99:313–5.
Egrilmez S, Ates H, Nalcaci S, Andac K, Yagci A. Surgically induced corneal refractive change following glaucoma surgery: non-penetrating trabecular surgeries versus trabeculectomy. J Cataract Refract Surg. 2004;30:1232–9.
Acknowledgements
The authors specially thank Dr. Saurabh Sawhney and Dr. Aashima Aggarwal for SIA calculator version 2.1, © 2010, which helped our Biostatistician Miss. Ramalakshmi to calculate the processes of vector analysis.
Author information
Authors and Affiliations
Contributions
DM: Idea for the project, surgeries performed and proof reading. AS: Editing the paper, writing the abstract and making the tables. SR: Writing the paper. MK: Statistics. RR: Proof reading.
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maheshwari, D., Segi, A., Shinde, S.R. et al. Surgically induced astigmatism following single site and twin site phacotrabeculectomy augmented with mitomycin C. Eye 36, 1100–1105 (2022). https://doi.org/10.1038/s41433-021-01601-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01601-2