Abstract
Intraocular liquids tamponade agents, such as perfluorocarbon liquids (PFCLs), semifluorinated alkanes (SFAs), silicone oils (SOs) and heavy silicone oils (HSOs), are a crucial intraoperative and/or postoperative tool in vitreoretinal surgery, in particular for the management of complex vitreoretinal diseases. However, their use is not without complications, which are potentially severe. Consequently, a growing interest has been devoted to the biocompatibility of these compounds and the adequacy of current regulations that should guarantee their safety. Obviously, an updated knowledge on research findings and potential risks associated to the use of intraocular liquid compounds is essential, not only for vitreoretinal surgeons, but also for any ophthalmologist involved in the management of patients receiving intraocular liquid tamponades. In light of this, the review provides a comprehensive characterisation of intraocular liquid tamponades, in terms of physical and chemical properties, current clinical use and possible complications. Moreover, this review focuses on the safety profile of these compounds, summarising the existing regulation and the available evidence on their biocompatibility.
摘要
眼内液体填充剂, 如全氟化碳液体 (PFCLs) 、半氟化烷烃 (SFAs) 、硅油 (SOs) 和重硅油 (HSOs), 是玻璃体视网膜手术中及术后重要的玻璃体填充物, 对于复杂的玻璃体视网膜疾病的治疗尤其重要。然而, 这些填充剂可产生甚至严重的并发症。因此, 人们越来越关注这些化合物的生物相容性以及现行法规是否足以保证其使用的安全性。显然, 不仅对玻璃体视网膜疾病的外科医生来说, 或是对任何参与眼内液体填充患者治疗的眼科医生来说, 对眼内液体填充剂的研究结果和潜在风险有最新的认识和了解是必不可少的。有鉴于此, 本文就眼内液体填充剂的理化性质、临床应用现状及可能产生的并发症作一综述。此外, 本文还对这些填充剂的安全性进行了汇总, 并总结了有关其生物相容性的现有法规和现有证据。
Similar content being viewed by others
Introduction
Pars plana vitrectomy (PPV) is the most common ophthalmic surgical procedure after cataract surgery. Along with the progressive development of vitrectomy systems, PPV has benefited from the introduction of intraocular medical devices. In particular, intraocular liquids tamponade agents have been used intraoperatively or postoperatively as vitreous substitutes, changing dramatically management and prognosis of complicated vitreoretinal diseases [1, 2].
Based on their chemical structure, intraocular liquids tamponades can be divided into perfluorocarbon liquids (PFCLs), semifluorinated alkanes (SFAs), silicone oils (SOs) and heavy silicone oils (HSOs). However, these compounds have been associated with multiple, potentially severe, ocular complications [1, 3, 4]. It is now known that emulsification plays a crucial role, particularly with regard to SO-related complications, but, the mechanisms and the influencing factors of this process in vivo have not been completely elucidated [4, 5]. Moreover, recently reported episodes of retinal toxicity raised significant concerns on the safety and the adequacy of current testing methods for intraocular liquid tamponades [6,7,8]. Thus, to use these compounds consciously, safely and effectively, vitreoretinal surgeons should have appropriate knowledge of their properties, the regulation to which they are subjected and the available evidence on their safety profile.
In light of the above points, this review aims to comprehensively characterise intraocular liquid tamponades in terms of chemico-physical properties, clinical use, complications, existing regulation and safety profile, focusing on the most updated evidence regarding their biocompatibility.
Methods
We performed a literature review regarding liquid intraocular tamponade agents using PubMed and Google to January 2021 and the following MeSH terms: vitreoretinal surgery; liquid intraocular tamponades; perfluocarbon liquids; semifluorinated alkanes; silicone oil; heavy silicone oil; emulsification; physical, chemical and rheological properties; complications; toxicity; inflammation; cytotoxicity tests. We included retrospective and prospective clinical studies with large sample size, laboratory experimental studies and authoritative reviews.
Medical device regulatory requirements
Intraocular liquid tamponades are classified as medical devices within the European Union (EU), according to the current regulation, the COUNCIL DIRECTIVE 93/42/EEC [9], and subsequent updates (M1 Directive 98/79/EC; M2 Directive 2000/70/EC; M3 Directive 2001/104/EC; M4 Regulation EC No 1882/2003; M5 Directive 2007/47/EC), which will be replaced by the Medical Device Regulation 2017/745 on 26th May 2021. The aim of these laws is to harmonise national provisions to protect patients and users, with regard to safety, efficacy and use of medical devices.
Classification
The classification criteria of medical devices are based on the vulnerability of human body to their effects [9]. Medical devices are classified as Classes I, IIa, IIb and III, depending on duration and type of contact with the patient body, or specific additional features (e.g., presence of animal derivatives, blood derivatives, etc.). Intraocular liquid tamponades are classified on the basis of the type of contact (vitreous chamber), and duration of contact (transient: <1 h; short-term: up to 30 days; long-term: >30 days). In particular, PFCLs and SFAs are class IIa, ‘surgical invasive medical devices intended for short-term use’, whereas SOs and HSOs are class IIb, ‘implantable devices and long-term surgically invasive medical devices’ [9].
Conformité Européene (CE) marking
The CE marking indicates that the medical device has been assessed for high safety, efficacy, and environmental protection requirements, fulfils the provisions of applicable directives and can be sold throughout the European Economic Area, considering the specific regulations of each EU country. In order to affix the CE marking to a medical device, the manufacturer should apply one of the Conformity Assessment Procedures and, when requested, apply to a Notified Body of his choice [9]. Once the CE marking and relative CE certificate are released by the Notified Body, they are valid for a maximum of five years and confirmed by annual inspections of the same Notified Body.
Essential requirements
All medical devices must meet the Essential Requirements concerning the characteristics, safety and performances set out in Annex I of the Council Directive 93/42/EEC [9], which apply to them, considering their intended use.
International organisation for standardization (ISO) standards
Besides the Essential Requirements [10], ISO standards are generally applicable to medical devices quality management system from design to release (ISO 13485:2016) [10] and risk management processes (ISO 14971:2019) [11]. Moreover, experts commissions develop ISO standards relevant to specific applications to define typical requirements of design phase, safety assessment, validations, manufacturing and testing. Specifically, regarding ocular endotamponades, the ISO 16672:2020 details the requirements for their intended performance, design attributes in terms of chemical and biological contaminants, physico-chemical properties, pre-clinical and clinical evaluation, sterilisation, stability, product packaging, product labelling and information supplied by the manufacturer [12]. Additional ISO standards applicable to intraocular liquid endotamponades are referred to ISO 16672:2020 (Table 1).
Physico-chemical characteristics
All intraocular liquid tamponades are synthetic chemicals, industrially produced with various synthesis processes.
Perfluorocarbon liquids
Perfluorocarbon liquids are fluorochemicals derived from hydrocarbons in which all hydrogen atoms are replaced by fluorine atoms. Due to the strength of the carbon-fluorine bond, saturated fluorinated compounds are chemically and biologically inert and thermodynamically stable [13, 14]. However, the synthesis process or oxidation during unsuitable storage conditions can result in the formation of reactive and potentially cytotoxic contaminants or impurities, such as partially hydrogenated perfluoroalkanes, perfluoroalkyl alcohols and benzene derivatives [6, 13]. Various purification methods aim to reduce the concentration of such impurities from the raw materials under cytotoxic levels after the synthesis. Storage-related impurities require additional stability testing.
Physically, PFCLs are characterised by high density, high interfacial tension (IT) with water, low dynamic viscosity (η) (more commonly <5 mPa∙s) and refractive index (RI) close to that of water (Table 2) [13]. Due to their density, these compounds are able to unfold, flatten and stabilise the detached retina and displace the subretinal fluid anteriorly [13]. The IT limits the potential passage of PFCL through retinal breaks (RBs), whereas the optical clarity allows an intraoperative visualisation clear enough to perform surgical manoeuvres such as laser photocoagulation or membrane peeling [1, 13]. Moreover, the low viscosity facilitates their handling, but contributes also to their high tendency to emulsify [7, 13]. Finally, PFCLs are volatile and the vapour pressure is crucial to optimise their removal from the vitreous cavity as it induces PFCL vaporisation on the retinal surface, once exposed to air during the fluid-air exchange [15]. Among them, perfluoro-n-octane (PFO) has the highest vapour pressure at room temperature and, thus, the highest tendency to evaporate during fluid-air exchange [15]. Moreover, as temperature increases, vapour pressure increases and viscosity decreases. Interestingly, significant changes of both properties have been reported within the range of temperatures registered during vitrectomy (range: 24.8 ± 0.8 − 33.6 ± 1.4 °C) [15, 16].
Semifluorinated alkanes
Semifluorinated alkanes are amphiphilic compounds, composed of perfluoroalkyl groups (hydrophilic) bonded to hydrocarbon-alkyl groups (hydrophobic), and soluble in PFCLs, SO and hydrocarbons. Their physical properties are summarised in Table 2.
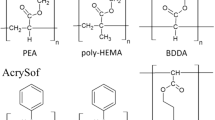
Silicone oils
Silicone oils are organosilicon compounds consisting of hydrophobic polymers of polydimethylsiloxane (PDMS), whose chemical structure is (-Si(CH3)2O-)n. Silicone oils made up only by PDMS polymers are indicated as standard or conventional. These chemicals are characterised by density slightly lower than water, IT with water lower than PFCLs, RI slightly higher than that of water (Table 2), and chemical inertness [2]. Increasing the length of silicone chains, the molecular weight (MW) and the viscosity of the final product vary accordingly. The most commonly used SOs are those with η of 1000 mPa∙s (MW ~37 kDa) and 5000 mPa∙s (MW ~65 kDa), but SOs of 2000 and 5700 mPa∙s are also currently available. SOs with longer chains and higher η show reduced propensity to emulsify in vitro, but are also more difficult to inject/remove during surgery, in particular with smaller-gauge instrumentation. It is worth to specify that the value of η refers to the SO dominant fraction, made up of chains of the desired length. Nevertheless, the synthesis process unavoidably generates a variable amount of silicone chains of both higher and lower degree of polymerisation and, despite subsequent purification processes, the final product contains a mixture of polymers and oligomers varying in chain length. Consistently, Mendichi et al. [17] found a significant variation of η value between different samples of SO 1000 mPa∙s, and, for some of them, poor agreement with the declared η.
Low molecular weight compounds
Regarding impurity profile, linear or cyclic PDMS chains of different length and low MW are referred to as low molecular weight compounds (LMWC). Among them, three cyclic oligosiloxanes, that are octamethylcyclotetrasiloxane (D4, MW: 296.64 g/mol), decamethylcyclopentasiloxane (D5, MW: 370.8 g/mol) and dodecamethylcyclohexasiloxane (D6, MW: 444.93 g/mol), have been better investigated, recently recognized by the European Chemicals Agency as toxic, and added into the Candidate List of Substances of Very High Concern for Authorisation due to their potential persistency, toxicity (<1000 ppm) and bioaccumulation (https://echa.europa.eu/it/candidate-list-table/-/dislist/details).
Mixtures of SOs and very-high-molecular-weight-components
Two new SOs, namely Siluron Xtra® (4100-4800 mPa∙s; Fluron GmbH) and Siluron2000 (2000-2400 mPa∙s; Fluron GmbH) have been recently developed with the aim of reducing susceptibility to emulsification of 1000 mPa∙s [18]. Indeed, the incorporation of a higher-MW component (PDMS of MW 423 kDa and 2.5 million mPa∙s) into a 1000 mPa∙s SO (10 and 5% PDMS 2.5 million mPa∙s in Siluron Xtra® and in Siluron2000, respectively) leads to a final product with increased extensional viscosity and decreased shear viscosity compared to the equivalent single grade SO, thus resulting in a SO bubble more resistant to emulsification but easier to handle [18].
Heavy silicone oils
Heavy silicone oils are polymers synthetised by mixing SO and SFA to achieve a tamponade heavier than water. Specifically, three HSOs are currently available: Densiron 68 (30.5% F6H8 and 69.5% of 5000 mPa∙s SO; Fluoron GmbH), Densiron Xtra (30.5% F6H8 and 69.5% of Siluron Xtra; Fluoron GmbH) and Oxane HD (89% 5000 mPa∙s SO and 11% partially fluorinated olefin, perfluorooctyl-5-methyl-hex-2-ene, indicated as RMN-3; Bausch & Lomb). The different composition results in different physical properties (Table 2).
Clinical use
Perfluorocarbon liquids
PFCLs are used as intraoperative tools in complex vitreoretinal procedures [1]. In particular, the most commonly used are PFO (molecular formula: C8F18) and perfluorodecalin (PFD, molecular formula: C10F18).
Surgical management of complicated primary RD and redetachment, particularly if associated with PVR, has been the most common indication for intraoperative PFCLs use [1, 14, 19]. In case of severe PVR, PFCLs can be used to facilitate posterior PVR dissection, identify residual preretinal tractions and small anterior RBs/holes, avoid too posterior drainage retinotomies and keep the retina stable during anterior PVR dissection or creation of relaxing retinotomies or retinectomies [1, 13, 14]. Intraoperative PFCL use has also been reported for RDs associated with giant retinal tears (GRT), macular holes (MH), ocular traumas, and, less commonly, proliferative diabetic retinopathy (PDR)-associated tractional RD, removal of foreign bodies or dislocated lens or lens fragments, retinopathy of prematurity and suprachoroidal/submacular haemorrhage. [1, 20,21,22,23]
Semifluorinated alkanes
SFAs have been first used intraoperatively for retinal unfolding and removal of SO remnants from the vitreous cavity and intraocular surfaces; then, as vitreous tamponades in complex RDs, mainly with inferior involvement and multiple inferior RBs [2, 19]. The SFAs currently CE-certified for intraocular use are perfluorobutylpentane (F4H5) and perfluorohexyloctane (F6H8). Specifically, F4H5, highly miscible with very viscous SO remnants, is approved as rinsing solution to remove residual emulsified SO and sticky oil from the vitreous chamber and adherent to the retina or intraocular lenses (IOLs) using a wash-out procedure [24, 25]. The heavier F6H8 is indicated as intraoperative tool, temporary intraocular tamponade and rinsing solution for IOLs after SO tamponade. Nevertheless, as rinsing solution, F6H8 resulted to be less effective than F4H5 in SO removal, both in vitro and in vivo [26]. With regard to its use as tamponade for complicated RDs conflicting results have been reported [3, 19, 27]. As the main problem related to F6H8 was the significant rate of emulsification and subsequent inflammation, at present, its use as intraocular tamponade has been replaced by HSO [19].
Silicone oils
The primary indication for SO use is the surgical management of complex RDs, associated with different features and aetiologies, such as PVR, multiple and/or posterior RBs, GRT, ocular trauma, PDR and necrotising retinitis [4]. Although the Silicone Study did not find any significant difference in terms of functional and anatomical outcomes comparing perfluoropropane and SO in RD with severe PVR, SO offers several advantages, such as longer support to the retina, compartmentalisation inside the vitreous cavity, decreased risk of slippage in case of retinectomies [28]. In case of GRT-RD, better anatomical outcomes have been reported in SO-tamponated eyes compared with gas-tamponated eyes [29]. In severe PDR, SO can help to release tractions and cause the eye compartmentalisation confining angiogenic growth factors and cytokines to the posterior segment, thus, potentially preventing the anterior segment neovascularisation [30]. The use of SO has been also proposed for surgical management of MH (especially in patients not suitable for gas tamponade or after failed primary surgery), persistent or uveitis-associated hypotony and suprachoroidal haemorrhage [4].
Comparing 1000 and 5000 mPa∙s SOs in RD repair, the viscosity resulted to be not associated with different anatomical and functional outcomes [31]. Therefore, the choice of SO is usually influenced by the ease of handling and the propensity to emulsification; thus, SO 1000 mPa∙s SO is generally preferred, whereas 5000 mPa∙s SO is usually chosen when a longer retention time is expected, due to its reduced propensity to emulsify.
Heavy silicone oils
Heavy SOs have been proposed as long-term tamponade for complicated RDs, especially with inferior or posterior RBs, MH-RD, and inferior PVR [2, 19]. Despite favourable anatomical and functional outcomes, no significant advantage has been found comparing HSO and standard SO in complex RDs with predominantly inferior pathology [4, 32, 33]. A hypothetical advantage of HSO was to prevent postoperative posterior and inferior PVR. Indeed, using gas or standard SO, the fluid rich of proinflammatory cytokines and growth factors, called ‘PVR soup’, is dislocated inferiorly or posteriorly in upright and supine position, respectively. The ability of HSO to separate the ‘PVR soup’ from posterior/inferior RBs and, consequently, from the cells involved in PVR formation (fibroblasts, retinal pigment epithelial (RPE) cells, Müller cells), was presumed to reduce the rate of inferior PVR and macular re-detachment [34]. However, the HSO Study, comparing eyes treated with HSO with eyes treated with standard SO for RD with inferior RBs and inferior PVR, found no significant difference in terms of anatomical success, final VA and overall rate of PVR between the two groups, as in HSO-eyes the PVR occurred more commonly superiorly [35].
Heavy SO tamponade has been also proposed for persistent MH [36] and massive suprachoroidal haemorrhage [37].
In conclusion, HSO is indicated in selected cases, such as persistent and/or myopic MH with or without RD, myopic foveoschisis, complex or traumatic RD with inferior RBs and PVR [34]. However, due to the potential complications, HSOs must be removed as soon as possible and their retention time is limited to a maximum of 3 months.
Ocular complications related to intraocular liquid tamponades
Perfluorocarbon liquids
Complications associated with long- and short-term PFCLs tamponade
Perfluorocarbon liquids have now been limited to intraoperative use as multiple and severe complications have been associated to their use as long-term tamponade agents, such as retinal structural damage, retinal toxicity, corneal toxicity, emulsification, severe inflammation, epiretinal and retrocorneal membranes [14]. Moreover, cataract, epiretinal membrane, PVR, raised intraocular pressure (IOP) have been described after short-term PFCL tamponade [38].
Complications associated with intraoperative use of PFCLs
The intraoperative use of PFCL has been demonstrated to induce a macrophagic foreign body response in RPE cells, potentially related to residual intravitreal/epiretinal PFCL droplets, accumulating also after complete air-fluid exchange [39, 40]. In addition, three main complications have been associated with the intraoperative PFCL use, namely intraocular retention, sticky oil and acute intraocular toxicity.
Subretinal retention of PFLC
Subretinal PFCL retention occurs in up to 11.1% of cases after its intraoperative use, more likely in case of large-sized retinotomies and presence of tractions at the RBs, with no differences between PFO and PFD [41]. Subretinal PFCL can result in RPE atrophy, photoreceptors damage, and, in case of subfoveal location, irreversible visual impairment [14, 41]. In the latter scenario, surgical removal has been suggested [41].
Sticky oil
The use of PFO followed by direct PFO/SO exchange has been associated with the formation of SO-like hyper-viscous material containing PFO, named ‘sticky oil’, strongly adherent to the retinal surface during SO removal [42, 43]. It has been demonstrated that PFCL interacts with HSO in vitro, leading to the formation of a hyper-viscous solution similar to sticky oil in appearance and texture [42]. It has been suggested that PFCL in direct contact with SO/HSO at the oil interface can change the solubility equilibrium, inducing modifications of the saturation point of the oil [42].
With regard to the surgical practice, due to the potential interaction between PFCL and SO/HSO, direct PFCL/SO or PFCL/HSO exchange should be avoided and PFCL removal must be as complete as possible before injecting SO or HSO, as indicated in the package inserts.
Acute intraocular toxicity
Severe acute intraocular toxicity after the intraoperative use of PFO Ala-Octa (Alamedics, Germany) during uneventful vitreoretinal procedures has been recently reported in 117 eyes resulting in very poor visual outcomes [6]. The main clinical findings were optic nerve atrophy, retinal atrophy, retinal vascular occlusion and retinal necrosis involving the posterior pole [6]. These episodes were attributed to specific lots of PFO, originally certified as safe, but then resulted to be toxic on a counter-analysis [6]. This alert raised by Pastor et al. [6]. highlighted the need to critically review the safety assessment of intraocular medical devices.
Semifluorinated alkanes
Several ocular complications have been associated with the use of F6H8 as tamponade, such as cataract progression, corneal opacification, pupillary block, raised IOP, hypotony, severe anterior chamber (AC) and posterior segment inflammation, retrolental, epiretinal and PVR membranes [2, 19, 27]. Overall, the main issue was the extensive emulsification, reported in up to 100% of cases, characterised by emulsified droplets dispersed in both anterior and posterior chamber, presumably causing an inflammatory and a foreign body reaction [19].
No complications have been associated with the use of F4H5 as rinsing solution [24].
Silicone oils
SO tamponades have been associated with multiple complications, such as emulsification, intraocular inflammation, keratopathy, cataract, IOP-related complications, optic nerve damage, epiretinal membrane and peri-oil fibrosis [4]. Although the pathogenetic mechanisms of these complications are not completely elucidated, SO emulsification appears to play the main role [44]. Emulsification of SO is the process by which small oil droplets (emulsion) are generated by the breakdown of the original SO bubble, resulting to be dispersed in the aqueous phase.
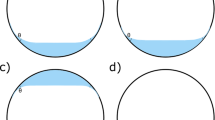
Factors influencing SO emulsification
At the end of vitrectomy, after SO injection, the filling of the vitreous chamber is never complete (a filling of 90% is considered satisfactory) and a pocket of aqueous solution is invariably present and forms an interface with the SO. The shape of this interface, determining the amount of retinal area that is effectively tamponated by the SO, depends on the contact angle at the triple line between SO, aqueous solution and the retinal wall, the IT, fluid densities, filling degree and vitreous chamber shape [45, 46]. Once an interface between SO and aqueous solution is formed, the tendency of SO to emulsify is influenced by the chemico-physical properties of the interface and of the bulk, and by external factors, such as temperature and mechanical energy provided to the system. It is believed that shear stresses at the SO-aqueous interface generated during eye rotations, play a crucial role on the creation of the interface instability and the breakdown of the SO-aqueous interface [5, 47]. The flow field induced by eye rotations has a complicated three-dimensional structure [48,49,50,51,52].
Among bulk chemico-physical properties, viscosity plays a particularly significant role, as increasing SO viscosity has a stabilising effect on the interface with water, essentially because highly viscous oils are less capable of flowing in the vitreous chamber than low viscosity fluids [53]. Encircling bands, used for RD repair, have also been observed to reduce SO tendency to emulsify, as the indentation reduces the intravitreal mobility of the fluids [53]. Recently, Wang et al. [54] tried to produce emulsions in a spherical model of the vitreous chamber subjected to a sequence of saccadic rotations, using various SOs and saline solutions, with the addiction of surfactant molecules. Interestingly, they concluded that droplet formation driven by a surface emulsification mechanism might be more relevant than bulk emulsification in the eye as a bulk emulsion was never observed, even in presence of surface-active molecules and, thus, quite small IT; however, in some cases small droplets formed in correspondence of the moving triple line of contact between the interface and the solid wall [54].
Finally, Francis et al. experimentally showed that also the energy from surgical handpieces could be sufficient to produce SO emulsification [55].
Generalities on interfacial properties of surfactants solutions
Surfactants are substances with the property of lowering the surface/interfacial tension of a liquid, facilitating surface wettability or miscibility between different liquids, reducing the energy needed to create new interfacial area. Thus, the presence of surfactants increases the propensity of the liquid to emulsify. Generally, they are organic compounds (simple molecules, polymers, macromolecules, proteins) with polar and non-polar groups, which have affinity with polar (e.g. water) and non-polar (e.g. oils, air) phases, respectively. A surfactant molecule attains a minimum energy configuration when located at the interface between the polar and non-polar phases. Surfactant molecules migrate (adsorb) spontaneously at the interface, determining an interfacial surfactant excess, denoted as ‘adsorption’, and resulting in a dramatic decrease of IT value, as compared to that of the pure liquid [19]. For surfactants soluble in one of the two phases, adsorption depends on surfactant concentration in the bulk and achieves specific values at equilibrium. This equilibrium can be easily perturbed, as occurs, for example, if a new interface of a surfactant solution is suddenly formed, or an existing interface is expanded or contracted. In all cases equilibrium is restored by time-dependent processes, driven by diffusion of surfactant between the bulk and the interfacial layer. It follows that, for these interfaces IT is a dynamic quantity, depending on time through surface composition and, in turn, on the history of the system. In particular, the dilational viscoelastic modulus (|E | ) measures the response of IT to variations of the amount of interfacial area [56]. Adsorption of surface-active molecules decreases the IT, favouring emulsification, and, at the same time, confers a viscoelastic character to the IT response to variations of the interfacial area. Such a dynamic effect, quantified by |E | , is involved in the stability of the interface and of the liquid film between approaching droplets. Specifically, high values of |E | confer high mechanical stability to the liquid interface and hinder the coalescence of drops, stabilising the emulsion once formed and determining its evolution in time (Fig. 1). Thus, interfacial properties are of paramount importance for emulsification.
The effect of molecule adsorption on SO interfacial properties
Exposition of intravitreal SO to endogenous molecules (proteins, lipids, etc.), the presence of which is favoured by the post-surgery inflammatory state of ocular tissues, has been shown to be relevant for SO emulsification, demonstrating that several biomolecules can act as surfactants, adsorbing at the water-oil interface [57,58,59]. Bartov et al. [57] demonstrated that various blood constituents, such as lymphocytes, plasma, red blood cells and haemoglobin, act as emulsifiers for SO when dissolved in aqueous solution. Heidenkummer et al. [58], adding biomolecules to various SOs, demonstrated that 1000 mPa·s SOs were the least stable, whereas the most effective emulsifiers were fibrinogen, fibrin and serum, followed by γ-globulins. Savion et al. [59] found that red blood cell membranes, plasma lipoproteins and purified HDL-apolipoproteins favoured SO emulsification. Owing to the importance of adsorption processes for the generation of emulsions, it is crucial to understand how endogenous molecules modify the properties of the SO-aqueous interface. In the absence of surfactant molecules, the IT of the SO-water system at equilibrium ranges between 35 and 42 mN/m. These values, however, are somehow irrelevant for the emulsification problem since, in realistic conditions, the IT is dramatically affected by the adsorption at the interface of the endogenous surfactants. Nakamura et al. [60] reported that IT value was of ≈ 16 mN/m between SO 1000 mPa·s and liquefied bovine vitreous at 37 °C, and ≈ 12.6 mN/m after the oils were put in contact with retinal tissue specimens for 24 hours. Moreover, the IT value of SO against intraocular fluids was less than half of that against distilled water [60]. Nepita et al. [61] demonstrated that the adsorption of albumin and/or γ-globulins (chosen as present in high concentrations in blood) reduces significantly the IT, and found large values of the dilational viscoelasticity of the interface, which favours the stability of the emulsion, once formed, by inhibition of drop coalescence. The emulsification tests confirmed that, in the presence of proteins, emulsions were stable on the time scale of months, suggesting that, under post-surgical conditions, small amounts of mechanical energy are likely to be sufficient to break the interface into small droplets, which, in addition, are stable against coalescence [61]. Besides biomolecules, other types of molecules can adsorb and modify SO interfacial properties. For instance, LMWC, detected in purified SOs despite purification and ultrapurification processes, are known to act as surfactants. Moreover, comparing solutions of buffer, human serum albumin and SOs of different composition, SOs with greater concentrations of LMW silicones have been associated with the increase of both protein denaturation/aggregation and SO-in water emulsions [62]. Dresp et al. [63] investigating the effect of detergent contamination, concluded that, in case of reusable instruments, remnants of cleaning substances or of the sterilisation process, can increase the risk of emulsification of SO, due to a significant decrease of the IT value. Finally, drugs used as intraoperative tools in PPV, can also promote SO emulsification. For instance, the presence of solid particles of triamcinolone acetonide (TA) can lead to the formation of a specific type of stable emulsions, termed Pickering emulsions, that can be dramatically enhanced by the presence of even small amounts of surfactants adsorbing at the particle surface and modifying their hydrophobic/hydrophilic character [64].
SO emulsification and intraocular inflammation
SO emulsification is involved in the pathogenesis of intraocular inflammation, along with direct SO immunogenicity/toxicity, presence of potentially toxic SO impurities, and mechanical gravitational damage [44]. It has been hypothesised that chemotaxis of inflammatory cells and foreign body inflammatory reaction can be triggered by SO microemulsions, phagocytosed by macrophages and RPE cells [44]. This inflammation, in turn, further stimulates SO emulsification, starting a vicious circle [44]. Consistently, a significant correlation between inflammation grade and SO tamponade duration has been documented [44]. Moreover, it has been reported that SO droplets induce a granulomatous foreign-body reaction, characterised by their phagocytosis by RPE cells and presence of epithelioid cells [34].
Corneal complications
The direct contact between emulsified SO droplets migrated to the AC and the corneal endothelium can also be involved in SO-related keratopathy [65]. This occurs mainly in aphakic eyes and is characterised by decreased endothelial cell density, retrocorneal membrane, attenuated endothelial cell borders, stromal hypercellularity, calcification and vascularisation of the superficial stroma [65].
IOP-related complications
Emulsification and inflammation are also involved in SO-related ocular hypertension that occurs in up to 56% of cases and vary from early, usually transient, postoperative IOP rise to long-term ocular hypertension, with intermediate or late onset, potentially impairing visual function [4, 66]. The migration of emulsified SO droplets to the AC, potentially persisting also after SO removal, could induce inflammation and mechanical obstruction of the trabecular meshwork, compromising aqueous humour outflow [66]. In addition, a mechanism of pupillary block can be involved in the onset of early postoperative ocular hypertension [66]; whereas, SO-related glaucoma is supposed to depend mainly on open-angle mechanisms, such as the migration of emulsified SO droplets and chronic inflammation [66,67,68].
Cataract
The development of cataract in SO-filled eyes has been described in up to 70% of cases; however, it has been suggested that the rate of this complications would actually be 100% considering an extended follow-up period [4]. With regard to the type, posterior subcapsular cataract appeared to be more commonly found in patients with SO tamponade [69].
SO-associated optic neuropathy
In addition to the optic nerve damage associated with SO-related glaucoma, a direct toxic effect of SO droplets migrated in the retrolaminar optic nerve could contribute to the development of SO-related neuropathy [46, 70]. Shields and Eagle described the presence of intra-optic nerve SO vacuoles of SO resulting in cavernous degeneration of the optic nerve [71]. Moreover, it has been suggested that a mechanism of active transport could be involved in the retrolaminar migration of SO [72].
Intracranial migration of SO
The intracranial migration of SO is a rare complication of SO tamponade [70]. It has been hypothesised that SO can move from the vitreous cavity, through the optic nerve and optic chiasma, into the cerebral ventricular system, more commonly into the lateral ventricules [70]. The exact mechanisms of migration are still unknown; however, migration of emulsified SO droplets phagocytosed by macrophages [73], congenital anatomical abnormalities resulting in communication between subretinal and subarachnoid space [74] and/or persistent elevated IOP [71], might have a role. More commonly found as an incidental finding, intracranial SO can mimic neurosurgical diseases, such as tumour or intracranial haemorrhage, on the head computed tomography; however, specific characteristics have been identified on neuroimaging for the differential diagnosis [75]. Only in one of the cases reported a ventriculoperitoneal shunt was performed as the patient presented with headache and elevated intracranial pressure [76]; otherwise, observation is the preferred option [75].
Silicone oil-related visual loss
The definition ‘silicone oil-related visual loss’ refers to unexplained loss of more than 2 Snellen lines after SO removal or, less frequently, during SO tamponade [77,78,79]. The pathogenesis and the incidence of this complication are still unknown; however, SO emulsification could be involved in some of the proposed pathogenetic mechanisms, such as sequestration of emulsified SO in the retina and optic nerve with consequent structural damage, emulsified SO tissue infiltration causing neuronal cell loss or mechanical vascular obstruction leading to retinal hypoxia [78]. In this regard, the reduced thickness of the inner retinal layers, indicative of macular neuronal cell loss, has been associated with severe visual loss in eyes treated with uncomplicated PPV and SO tamponade for primary rhegmatogenous RD [80]. Other hypotheses are SO-related oxidative stress, SO-induced local changes in ions concentration and light phototoxicity during SO removal [50]. Finally, as this complication has been rarely described in eyes with duration of SO tamponade ≤8 weeks, it has been suggested that SO intraocular retention time could be a risk factor [79].
Heavy silicone oils
The spectrum of HSO-related complications overlaps that of SO. However, the different physico-chemical properties account for some differences [34]. Specifically, it has been speculated that adding SFAs increases the hydrophilicity and reduces the viscosity of the final HSO, that results to be more prone to emulsify [81]. The HSO-induced time-dependent intraocular inflammation resulted to be greater than that caused by standard SOs [44]. HSO is supposed to trigger a delayed type IV hypersensitivity reaction and complement factors and immunoglobulins have been detected on its surface [34]. The significant correlation between intraocular inflammation severity and intraocular HSO retention time dictates the restriction of tamponade duration [34].
IOP-related complications
A recent meta-analysis showed a trend towards a higher rate of ocular hypertension in HSO-filled eyes compared with SO-filled eyes [68]. In particular, Wong et al. [82] reported that the mean postoperative IOP in HSO-filled eyes was significantly higher than that of SO-filled eyes on day 1 and 7-14 postoperatively. Moreover, increased IOP at 1-day follow-up is a known negative prognostic factor for glaucoma [67].
Safety assessment
Regulations
The manufacturer of intraocular liquid tamponades guarantees their safety and efficacy within their intended purpose. During the product development, potential risks associated with technical design and manufacturing process are evaluated. Considering the intended purpose, the assessment of the compatibility with biological tissues, cells and body fluids of materials constituting the device, delivery systems or other medical devices in combined use is performed, along with validation of manufacturing processes (bulk preparation, filling, sterilisation, packaging), definition of medical device specifications and validation of its performance. Relevant pre-clinical and clinical data have to be produced. The technical file of the device includes detailed information about design, function, composition, intended use, manufacturing process, validation of testing methods, equipment and processes, and clinical evaluation. The Notified Body examines this file, verifies the compliance with the applicable Directive and releases the CE certificate.
After the market authorisation, the conformity of each batch with the essential requirements is assured by the tests reported in the analysis certificate. Specifically, the testing methods that can be performed to assure quality and conformity of a batch of finished medical device, are divided in two categories: physico-chemical and biological analyses.
Physico-chemical analyses
Physico-chemical analytical methods, such as gas chromatography, mass spectrometry or spectroscopy, detect and quantify toxic impurities in intraocular liquid tamponades. However, none of them directly assesses their toxicity. Toxicity thresholds of some substances are available for animals and can be estimated in humans according to ISO10993-17 [83]. However, toxicity thresholds are not available for all substances, and, thus, chemico-physical tests can confirm the device characteristics and specifications, but not assess the potential toxicity.
Biological analyses
In vitro cytotoxicity tests
In vitro cytotoxicity tests, described in ISO 10993-5 [84], aim to detect the potential toxicity of medical devices using in vitro cultures of established cell lines and assessing cellular health through different endpoints, such as morphology or viability. According to the methodology, these tests are divided in extract tests, indirect contact tests and direct contact tests [84]. Direct contact cytotoxicity tests provide both qualitative microscopic evaluation of cell morphology and quantitative evaluation of cell viability. ISO 10993-5 provides guidelines to correctly perform the tests; however, the most suitable test to analyse a specific intraocular tamponade has to be selected case by case based on its physico-chemical properties and the method has to be validated to define standard test conditions ensuring reliable and reproducible results [9, 84]. The risks of test failure have to be assessed to identify and address possible critical phases. Regarding intraocular liquid tamponades, the main risks are linked to PFCL volatility and possible sample evaporation, heaviness of PFCL potentially inducing mechanical cell deformation and mortality, SO buoyancy leading to absence of direct contact or insufficient contact time between sample and cell layer. Romano et al. [7, 8] validated direct contact tests for both PFCL and SO using murine fibroblast cells BALB/3T3 and human RPE cells (ARPE-19 cells) incubated with the sample for 24 h. Pastor et al. [6] used direct contact test, patented by their group [85], exposing ARPE-19 cells to PFO for 60 min after a 24-hour cell cycle synchronisation in foetal bovine serum-free cell culture medium. The application of an intraocular tamponade sample to the cells is critical [8]. Specifically, PFCLs need to be applied directly in contact with the cell layers in presence of the culture media in the wells. Romano et al. [7] validated the application of PFCL in one single bubble forming on the well bottom and occupying 59% of cell area. With regard to the potential floating of SOs on the culture medium surface, Romano et al. [8] applied SO samples on the cells after removing the culture media, followed by soft mixing of the cell culture plate before addition of the culture media, obtaining 100% contact area.
Ex vivo studies
Ex vivo tests are conducted on isolated tissue cultures, chosen on the basis of the intended use of the medical device, to represent more closely the in vivo condition as tissue cytoarchitecture is preserved. Therefore, regarding intraocular liquid tamponade, tests are performed on culture models of animal or human retina.
In vivo animal studies
Experimental animal models best represent the in vivo scenario, whereas the main limitation is the use of animals itself. Different animal eye models (rabbit, pig, monkey) have been used to assess ocular endotamponades applied intravitreally through different evaluation methods, such as clinical examination, electrophysiology and histological examinations [86,87,88,89,90,91,92,93,94,95].
Experimental evidence
Perfluorocarbon liquids
Partially hydrogenated perfluoroalkanes are known impurities of PFCLs and have been found to induce cytotoxic effects in primary cultures fibroblast cells at concentration > 10% [96]. Pastor et al. [6], using different chemical analytical methods, detected both perfluoro-derived and benzene-derived compounds in the toxic PFO batches responsible for the reported cases of acute intraocular toxicity. Specifically, two hydroxyl compounds, namely perfluorooctanoic acid (PFOA) and dodecafluoro-1-heptanol (DFH), and two benzene derivatives, such as ethylbenzene and p-xylene, were identified as suspected toxic compounds [6]. In response, Chang et al. [97] claimed that a comprehensive chemical analysis of PFCLs, is adequate to detect all potential toxic contaminants/impurities. However, recent experimental evidence highlighted the primary role of in vitro cytotoxicity tests to assess properly the ‘safety thresholds’ of these compounds. Menz et al. [98] proposed to determine the content of reactive H in partially hydrogenated perfluoroalkanes, defined as ‘H-value’, through the electrochemical determination of the fluorine resulting from their reaction with diamine. The limit of 10 ppm was identified as the threshold ensuring the absence of cytotoxicity and, thus, PFCL safety [98]. Nevertheless, Ruzza et al. [99] showed that the testing method used by Menz et al. [98] was unable to detect potentially toxic contaminants without reactive hydrogens, and that the H-content was inadequate to predict PFCL cytotoxicity. Indeed, Ruzza et al. [99] validated the use of 1H NMR spectroscopy to quantitatively analyse the perfluorinated compounds and determine a wide range of potential contaminants, including partially hydrogenated perfluoroalkanes (also not reacting with hexamethylenediamine), perfluoroalkyl alcohols, PFOA, and benzene derivatives. Moreover, PFCL samples contaminated with PFOA and HPFO, both known to be highly toxic impurities [6] although a reactive H is not present, showed very low H-content (0.13 and 0.07 ppm, respectively) but very high cytotoxicity on ARPE-19 and BALB 3T3, using direct contact in vitro cytotoxicity test validated according to ISO 10993-5 [84]. PFCL samples contaminated with 5HPFO, instead, showed very high H-content (up to 2800 ppm) but no cytotoxic effect [99]. In addition, 2 of 15 tested commercially available PFO and PFD devices resulted to be cytotoxic according to ISO10993-5 [84, 99]. Consistently, Srivastava et al. [100] used chemical analyses to identify and measure PFOA, DFH, ethylbenzene and tributyltin bromide in toxic batches of PFO; then, performed direct contact in vitro cytotoxicity tests to determine the concentrations at which these contaminants resulted to be toxic and, thus, their ‘safety threshold’.
The reliability of direct contact in vitro cytotoxicity tests to assess PFCLs cytotoxicity has been confirmed in ex vivo models [6, 7]. In particular, Pastor et al. [6], testing the toxic samples of AlaOcta PFO in porcine neuroretina explants, reported results consistent with those obtained with cell cultures. Romano et al. [7] compared the results of ex vivo culture model of human retina incubated with PFCL samples for 24 h to direct contact in vitro cytotoxicity test in the ARPE-19 cell line. The percentage of cell mortality was comparable after application of not cytotoxic control, but higher in the ex vivo model after application of cytotoxic control (12.5% 1H PFO), indicating higher sensibility of the latter [7].
In addition to the toxicity, the high density of PFCLs can induce potential cellular mechanical damage. Mertens et al. [101] reported that human RPE cells decreased in number but maintained their proliferation capacity after incubation with PFD, suggesting a mechanical rather than toxic effect. Inoue et al. [102], testing PFO on ARPE-19 and retinal ganglion cells (RGCs), reported a direct toxic effect on ARPE-19 cells after 7-day incubation. However, after 3-day incubation, the number of viable RGCs decreased only after PFO contact at the apical surface but not at the basolateral side, suggesting a mechanical effect [102]. Several in vivo studies confirmed the time-dependency of the PFCL-induced mechanical damage induced. [87,88,89,90, 102] Progressively worse histological changes, mainly in the inferior retina, have been associated with PFO tamponade in rabbit eyes starting at 6 days after surgery [88]. Intraoperative use of PFO in rabbits and pigs resulted in no retinal adverse effects; whereas, PFO-tamponade longer than 1-week led to globule dispersion and morphologic retinal alterations [86]. Vitreous substitution with different highly purified PFCLs in rabbit eyes has been found to induce progressive histological retinal changes at 2, 4 and 8 weeks after surgery [90]. Intraretinal infiltration of PFD has been documented in rabbits after 1 week of tamponade [87]. Finally, subretinal PFD has been associated with loss of photoreceptors segments at 1 day and localised retinal atrophy at 5-7 days after surgery in rabbit eyes [89].
Semifluorinated alkanes
Morphological retinal changes or reduced cell count in the inferior retina of rabbits have been documented about 3 months after intravitreal injection of F6H8 [91, 92]. Moreover, a significantly decreased fluorescent emission from cultures of human RPE cells and human corneal endothelial cells has been reported after 5-day incubation with F6H8 [103]. Porcine corneal endothelial organ culture models exposed to F4H5 for 120 min showed a significant endothelial cell density decrease and changes in endothelial morphology after 15 days of culture [104].
Silicone oils
Due to the known potential toxicity of LMWC, physicochemical analyses of SO have been mainly focused to assess their purity in terms of MW distribution (MWD) and LMWC content. In this regard, Mendichi et al. [17], analysing 10 purified SOs 1000 mPa∙s of different brands, demonstrated that these compounds have a broad MWD, as confirmed by Dresp [105] in SOs 2000 and 5000 mPas, with significant differences between different SOs [17, 105]. Moreover, the content of LMWC with MW ≤ 1000 g/mol varied significantly between the SOs 1000 mPa∙s (range: 51–1151 ppm) [17] and the oligosiloxanes content was significantly variable in different SOs 2000 and 5000 mPa∙s [105]. However, Mendichi et al. [17] demonstrated that LMWC with MW ≤ 1000 g/mol accounted only for a small proportion of ‘impurities’ in SOs 1000 mPa∙s, whilst a significant amount was represented by the relative content of LMWC with MW ≤ 10,000 g/mol, that, also, significantly differed between the samples (range: 2.31–9.40%). It has been speculated that D4, D5 and D6 can diffuse from vitreous cavity into surrounding tissues, penetrating into cellular membranes, and the injection of D4 and D5 into the AC of rabbit eyes induced a severe inflammatory reaction [106].
Only two studies investigated in vitro cytotoxicity of SOs [8, 102]. Inoue et al. [102] incubated ARPE-19 cells and RGCs with purified SO 1000 mPa∙s. No cytotoxic effect was detected in both cell lines at 3 days; whereas a significant decrease of ARPE-19 viability at 7 days occurred only when the contact area cells-SO was at the basolateral side, suggesting a mechanical rather than toxic effect [102]. Consistently, Romano et al. [8] did not detect any cytotoxicity in both ARPE-19 and BALB3T3 cells after 24-h exposure to purified SO 1000 mPa∙s.
A larger number of studies assessed safety of SO trough in vivo tests. [87, 93,94,95, 107] Penetration of SO into the inner retina and epiretinal membrane formation have been described in rabbit eyes after the intravitreal injection of emulsified SO 20 mPa∙s; whereas no histological changes were detected in eyes filled with non-emulsified SO [93]. In contrast, Versura et al. [87] found small SO droplets within retinal layers at 4 weeks from SO 1000 and 3000 mPa∙s injection. Moreover, SOs were found to be able to dissolve lipids and to evoke a local immunological reaction with accumulation of immunoproteins in ocular tissues, even in absence of obvious toxic effects [87]. Intravitreal membranes attached to the retina have been detected in SO 1000 mPa∙s-filled rabbit eyes in absence of significant inflammatory reaction [94]. Mackiewicz et al. [107] did not detect any significant histological retinal change and inflammation in rabbit eyes after 3-month tamponade with SO 1000, 3000 and 5000 mPa∙s.
Heavy silicone oils
Mackiewicz et al. [107] analysed clinical, electrophysiological and histological findings of rabbit eyes after 3-month tamponade with Densiron68 and other not commercially available HSOs. Densiron 68 and F4H5-based HSOs resulted to be well tolerated with no significant inflammation and histological retinal damage [107].
Conclusions
Due to their chemico-physical properties, intraocular liquid tamponade agents are needful tools in vitreoretinal surgery. However, there are still relevant concerns regarding their propensity to emulsify and their potential intraocular toxicity. This review provided an overview of their current clinical use and associated complications, focusing on the available scientific literature regarding their biocompatibility. Safety thresholds for concentrations of tamponade impurities have not yet been identified and there is still confusion on the properties that need to be tested as well as on the tests required for the safety assessment. Moreover, although it has been known that LMWC can potentially induce toxic effect in the long term and can act as surfactants for SO, no studies analysed the relation between different concentrations of LMWC and chronic adverse effects or SO emulsification. The properties that can impact on the removal of intraocular liquid tamponade agents also need to be further investigated as this step is crucial in the surgical practice [40, 42, 108]. In this regard, the management of temperature during vitreoretinal surgery could be a promising perspective as remarkable changes of both vapour pressure and viscosity have been reported within the range of mean temperatures registered during a vitrectomy [15, 16]. Finally, in a realistic scenario, more than one tamponade can be used during the same procedure, in addition to other intraocular devices (such as vital dyes) or drugs (such as TA). So far, the mechanisms of the related adverse effects are still not completely elucidated and there is no agreement on the appropriate tamponade-specific regulations aimed to ensure the safety of these compounds. Future studies addressing the effect of their properties and components on their chemico-physical behaviour and interactions are necessary for the optimisation of their clinical use. In perspective, it will be important to investigate cooperative effects that may arise from the interaction of multiple intraocular devices as well as their interaction with biological molecules and drugs.
References
Yu Q, Liu K, Su L, Xia X, Xu X. Perfluorocarbon liquid: its application in vitreoretinal surgery and related ocular inflammation. Biomed Res Int. 2014;2014:250323.
Kleinberg TT, Tzekov RT, Stein L, Ravi N, Kaushal S. Vitreous substitutes: a comprehensive review. Surv Ophthalmol. 2011;56:300–23.
Schatz B, El-Shabrawi Y, Haas A, Langmann G. Adverse side effects with perfluorohexyloctane as a long-term tamponade agent in complicated vitreoretinal surgery. Retina. 2004;24:567–73.
Wagenfeld L, Zeitz O, Skevas C, Richard G. Long-lasting endotamponades in vitreoretinal surgery. Ophthalmologica. 2010;224:291–300.
Chan YK, Ng CO, Knox PC, Garvey MJ, Williams RL, Wong D. Emulsification of silicone oil and eye movements. Invest Ophthalmol Vis Sci. 2011;52:9721–7.
Pastor JC, Coco RM, Fernandez-Bueno I, Alonso-Alonso ML, Medina J, Sanz-Arranz A. Acute retinal damage after using a toxic perfluoro-octane for 500 vitreo-retinal surgery. Retina. 2017;37:1140–51.
Romano MR, Ferrara M, Gatto C, Ferrari B, Giurgola L, D’Amato, et al. Evaluation of cytotoxicity of perfluorocarbons for intraocular use by cytotoxicity test in vitro in cell lines and human donor retina ex vivo. Transl Vis Sci Technol. 2019;8:24.
Romano MR, Ferrara M, Gatto C, Giurgola L, Zanoni M, Angi M, et al. Safety of silicone oils as intraocular medical device: An in vitro cytotoxicity study. Exp Eye Res. 2020;194:108018.
COUNCIL DIRECTIVE 93/42/EEC of 14 June 1993.
ISO 13485, 2016. Medical devices — Quality management systems — Requirements for regulatory purposes. https://www.iso.org/obp/ui#iso:std:iso:13485:ed-3:v1:en
ISO 14971, 2019. Medical devices - Application of risk management to medical devices. https://www.iso.org/obp/ui#iso:std:iso:14971:ed-3:v1:en
ISO 16672, 2020. Ophthalmic implants – ocular endotamponades. https://www.iso.org/obp/ui/#iso:std:iso:16672:ed-2:v1:en
Wong D, Lois N. Perfluorocarbons and semifluorinated alkanes. Semin Ophthalmol. 2000;15:25–35.
Georgalas I, Ladas I, Tservakis I, Taliantzis S, Gotzaridis E, Papaconstantinou D, et al. Perfluorocarbon liquids in vitreoretinal surgery: a review of applications and toxicity. Cutan Ocul Toxicol. 2011;30:251–62.
Romano MR, Romano V, Mauro A, Angi M, Costagliola C, Ambrosone L. The effect of temperature changes in vitreoretinal surgery. Transl Vis Sci Technol. 2016;5:4.
Romano MR, Vallejo-Garcia JL, Romano V, Angi M, Vinciguerra P, Costagliola C. Thermodynamics of vitreoretinal surgery. Curr Eye Res. 2013;38:371–4.
Mendichi R, Schieroni AG, Piovani D, Allegrini D, Ferrara M, Romano MR. Comparative study of chemical composition, molecular and rheological properties of silicone oil medical devices. Transl Vis Sci Technol. 2019;8:9.
Williams RL, Day M, Garvey MJ, English R, Wong D. Increasing the extensional viscosity of silicone oil reduces the tendency for emulsification. Retina. 2010;30:300–4.
Heimann H, Stappler T, Wong D. Heavy tamponade 1: a review of indications, use, and complications. Eye (Lond). 2008;22:1342–59.
Ambresin A, Wolfensberger TJ, Bovey EH. Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 degrees retinal photocoagulation. Retina. 2003;23:622–8.
Imamura Y, Minami M, Ueki M, Satoh B, Ikeda T. Use of perfluorocarbon liquid during vitrectomy for severe proliferative diabetic retinopathy. Br J Ophthalmol. 2003;87:563–6.
Millsap CM, Peyman GA, Ma PE, Greve MDJ. The surgical management of retinopathy of prematurity using a perfluorocarbon liquid. Int Ophthalmol. 1994;18:97–100.
Gibran SK, Romano MR, Wong D. Perfluorocarbon liquid assisted large retinal epithelium patching in sub-macular hemorrhage secondary to age related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2009;247:187–91.
Stalmans P, Pinxten A, Wong DS. Cohort safety and efficacy study of siluron2000 emulsification-resistant silicone oil and F4h5 in the treatment of full-thickness macular hole. Retina. 2015;35:2558–66.
Stappler T, Williams R, Wong D. F4H5: a novel substance for the removal of silicone oil from intraocular lenses. Br J Ophthalmol. 2010;94:364–7.
Liang Y, Kociok N, Leszczuk M, Hiebl W, Theisinger B, Lux A, et al. A cleaning solution for silicone intraocular lenses: “Sticky Silicone Oil”. Br J Ophthalmol. 2008;92:1522–7.
Kirchhof B, Wong D, Van Meurs J, Hilgers RD, Macek M, Lois N, et al. Use of perfluorohexyloctane as a long-term internal tamponade agent in complicated retinal detachment surgery. Am J Ophthalmol. 2002;133:95–101.
Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 2. Arch Ophthalmol. 1992;110:780–92.
Al-Khairi AM, Al-Kahtani E, Kangave D, Abu El-Asrar AM. Prognostic factors associated with outcomes after giant retinal tear management using perfluorocarbon liquids. Eur J Ophthalmol. 2008;18:270–7.
Castellarin A, Grigorian R, Bhagat N, Del Priore L, Zarbin MA. Vitrectomy with silicone oil infusion in severe diabetic retinopathy. Br J Ophthalmol. 2003;87:318–21.
Zafar S, Shakir M, Mahmood SA, Amin S, Iqbal Z. Comparison of 1000-Centistoke versus 5000-Centistoke silicone oil in complex retinal Detachment Surgery. J Coll Physicians Surg Pak. 2016;26:36–40.
Romano MR, Stappler T, Marticorena J, Groenewald C, Pearce I, Gibran SK, et al. Primary vitrectomy with Densiron-68 for rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2008;246:1541–6.
Kocak I, Koc H. Comparison of densiron 68 and 1000 cSt silicone oil in the management of rhegmatogenous retinal detachment with inferior breaks. Int J Ophthalmol. 2013;6:81–4.
Morescalchi F, Costagliola C, Duse S, Gambicorti E, Parolini B, Arcidiacono B, et al. Heavy silicone oil and intraocular inflammation. Biomed Res Int. 2014;2014:574825.
Joussen AM, Rizzo S, Kirchhof B, Schrage N, Li X, Lente C, et al. Heavy silicone oil versus standard silicone oil in as vitreous tamponade in inferior PVR (HSO study): interim analysis. Acta Ophthalmol. 2011;89:e483–9.
Rizzo S, Genovesi-Ebert F, Vento A, Cresti F, Miniaci S, Romagnoli MC. Heavy silicone oil (Densiron-68) for the treatment of persistent macular holes: Densiron-68 endotamponade for persistent macular holes. Graefes Arch Clin Exp Ophthalmol. 2009;247:1471–6.
Valldeperas X, Elizalde J, Romano MR, Wong D. Heavy silicone oil (Densiron) and supine position in the management of massive suprachoroidal hemorrhage: use of heavy silicone for suprachoroidal hemorrhage. Retin Cases Brief Rep. 2012;6:80–1.
Drury B, Bourke RD. Short-term intraocular tamponade with perfluorocarbon heavy liquid. Br J Ophthalmol. 2011;95:694–8.
Romano MR, Baddon C, Heimann H, Wong D, Hiscott P. Histopathological findings in an epimacular membrane after intraoperative use of perfluorocarbon liquid. Eye (Lond). 2010;24:740–2.
Romano MR, Vallejo-Garcia JL, Castellani C, Costagliola C, Vinciguerra P. Residual perfluorocarbon liquid (PFCL) in human eyes. Ann Acad Med Singap. 2014;43:195–6.
Liu W, Gao M, Liang X. Management of subfoveal perfluorocarbon liquid: a review. Ophthalmologica. 2018;240:1–7.
Romano MR, Vallejo-Garcia JL, Parmeggiani F, Romano V, Vinciguerra P. Interaction between perfluorcarbon liquid and heavy silicone oil: risk factor for “Sticky Oil” formation. Curr Eye Res. 2012;37:563–6.
Veckeneer MA, de Voogd S, Lindstedt EW, Menz DH, van Meurs JC. An epidemic of sticky silicone oil at the Rotterdam Eye Hospital. Patient review and chemical analyses. Graefes Arch Clin Exp Ophthalmol. 2008;246:917–22.
Semeraro F, Russo A, Morescalchi F, Gambicorti E, Vezzoli S, Parmeggiani F, et al. Comparative assessment of intraocular inflammation following standard or heavy silicone oil tamponade: a prospective study. Acta Ophthalmol. 2019;97:e97–102.
Eames I, Angunawela RI, Aylward GW, Azarbadegan A. A theoretical model for predicting interfacial relationships of retinal tamponades. Invest Ophthalmol Vis Sci. 2010;51:2243–7.
Isakova K, Pralits JO, Romano MR, Beenakker JWM, Shamonin DP, Repetto R. Equilibrium shape of the aqueous humor-vitreous substitute interface in vitrectomized eyes. J Model Ophthalmol. 2017;1:31–46.
Isakova K, Pralits JO, Repetto R, Romano MR. A model for the linear stability of the interface between aqueous humor and vitreous substitutes after vitreoretinal surgery. Phys Fluids. 2014;26:124101.
Repetto R. An analytical model of the dynamics of the liquefied vitreous induced by saccadic eye movements. Meccanica. 2006;41:101–17.
Repetto R, Siggers JH, Stocchino A. Mathematical model of flow in the vitreous humor induced by saccadic eye rotations: effect of geometry. Biomech Model Mechanobiol. 2010;9:65–76.
Repetto R, Stocchino A, Cafferata C. Experimental investigation of vitreous humour motion within a human eye model. Phys Med Biol. 2005;50:4729–43.
Stocchino A, Repetto R, Cafferata C. Eye rotation induced dynamics of a Newtonian fluid within the vitreous cavity: the effect of the chamber shape. Phys Med Biol. 2007;52:2021.
Rossi T, Querzoli G, Pasqualitto G, Iossa M, Placentino L, Repetto R, et al. Ultrasound imaging velocimetry of the human vitreous. Exp Eye Res. 2012;99:98–104.
Chan YK, Cheung N, Wong D. Factors influencing the shear rate acting on silicone oil to cause silicone oil emulsification physical factors of silicone oil emulsification. Invest Ophthalmol Vis Sci. 2014;55:7451–6.
Wang R, Snead M, Alexander P, Wilson DI. Assessing bulk emulsification at the silicone oil–saline solution interface in a 3D model of the eye. Acta Ophthalmol. 2021;99:e209–14.
Francis JH, Latkany PA, Rosenthal JL. Mechanical energy from intraocular instruments cause emulsification of silicone oil. Br J Ophthalmol. 2007;91:818–21.
Liggieri L, Miller R. Relaxation of surfactants adsorption layers at liquid interfaces. Curr Opin Colloid Interface Sci. 2010;15:256–63.
Bartov E, Pennarola F, Savion N, Naveh N, Treister G. A quantitative in vitro model for silicone oil emulsification. Role blood constituents Retin. 1992;12:S23–7.
Heidenkummer HP, Kampik A, Thierfelder S. Emulsification of silicone oils with specific physicochemical characteristics. Graefes Arch Clin Exp Ophthalmol. 1991;229:88–94.
Savion N, Alhalel A, Treister G, Bartov E. Role of blood components in ocular silicone oil emulsification. studies on an in vitro model. Invest Ophthalmol Vis Sci. 1996;37:2694–9.
Nakamura K, Refojo MF, Crabtree DV. Factors contributing to the emulsification of intraocular silicone and fluorosilicone oils. Invest Ophthalmol Vis Sci. 1990;31:647–65.
Nepita I, Repetto R, Pralits JO, Romano MR, Ravera F, Santini E, et al. The role of endogenous proteins on the emulsification of silicone oils used in vitreoretinal surgery. BioMed Res Int. 2020;2020:2915010.
Nayef LM, Khan MF, Brook MA. Low molecular weight silicones particularly facilitate human serum albumin denaturation. Colloids Surf B. 2015;128:586–93.
Dresp JH, Menz DH. Preparation and processing of vitreoretinal instrumentation and equipment as a risk factor for silicone oil emulsification. Retina. 2004;24:110–5.
Maestro A, Santini E, Zabiegaj D, Llamas S, Ravera F, Liggieri L, et al. Particle and particle-surfactant mixtures at fluid interfaces: Assembly, morphology, and rheological description. Adv Condens Matter Phys. 2015;2015:917516.
Miller JB, Papakostas TD, Vavvas DG. Complications of emulsified silicone oil after retinal detachment repair. Semin Ophthalmol. 2014;29:312–8.
Ichhpujani P, Jindal A, Jay, Katz L. Silicone oil induced glaucoma: a review. Graefes Arch Clin Exp Ophthalmol. 2009;247:1585–93.
Romano MR, Angi M, Romano V, Parmeggiani F, Campa C, Valldeperas X, et al. Intraocular pressure changes following the use of silicone oil or Densiron 68 as endotamponade in pars plana vitrectomy. Clin Ophthalmol. 2010;4:1391–6.
Romano V, Cruciani M, Semeraro F, Costagliola C, Romano MR. Development of ocular hypertension secondary to tamponade with light versus heavy silicone oil: a systematic review. Indian J Ophthalmol. 2015;63:227–32.
Feng H, Adelman RA. Cataract formation following vitreoretinal procedures. Clin Ophthalmol. 2014;8:1957–65.
Grzybowski A, Pieczynski J, Ascaso FJ. Neuronal complications of intravitreal silicone oil: an updated review. Acta Ophthalmol. 2014;92:201–4.
Shields CL, Eagle RC Jr. Pseudo-Schnabel’s cavernous degeneration of the optic nerve secondary to intraocular silicone oil. Arch Ophthalmol. 1989;107:714–7.
Knecht P, Groscurth P, Ziegler U, Laeng HR, Jaggi GP, Killer HE. Is silicone oil optic neuropathy caused by high intraocular pressure alone? A semi-biological model. Br J Ophthalmol. 2007;91:1293–5.
Papp A, Kiss EB, Tímár O, Szabó E, Berecki A, Tóth J, et al. Long-term exposure of the rabbit eye to silicone oil causes optic nerve atrophy. Brain Res Bull. 2007;74:130–3.
Honavar SG, Goyal M, Majji AB, Sen PK, Naduvilath T, Dandona L. Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999;106:169–77.
Potts MB, Wu AC, Rusinak DJ, Kesavabhotla K, Jahromi BS. Seeing floaters: a case report and literature review of intraventricular migration of silicone oil tamponade material for retinal detachment. World Neurosurg. 2018;115:201–5.
Hruby PM, Poley PR, Terp PA, Thorell WE, Margalit E. Headaches secondary to intraventricular silicone oil successfully managed with ventriculoperitoneal shunt. Retin Cases Brief Rep. 2013;7:288–90.
Issa R, Xia T, Zarbin MA, Bhagat N. Silicone oil removal: post-operative complications. Eye (Lond). 2020;34:537–43.
Oliveira-Ferreira C, Azevedo M, Silva M, Roca A, Barbosa-Breda J, Faria PA, et al. Unexplained visual loss after silicone oil removal: a 7-year retrospective study. Ophthalmol Ther. 2020;9:1–13.
Christensen UC, la Cour M. Visual loss after use of intraocular silicone oil associated with thinning of inner retinal layers. Acta Ophthalmol. 2012;90:733–7.
Scheerlinck LM, Schellekens PA, Liem AT, Steijns D, Leeuwen R. Incidence, risk factors, and clinical characteristics of unexplained visual loss after intraocular silicone oil for macula-on retinal detachment. Retina. 2016;36:342–50.
Caramoy A, Schröder S, Fauser S, Kirchhof B. In vitro emulsification assessment of new silicone oils. Br J Ophthalmol. 2010;94:509–12.
Wong D, Kumar I, Quah SA, Ali H, Valldeperas X, Romano MR. Comparison of postoperative intraocular pressure in patients with Densiron-68 vs conventional silicone oil: a case-control study. Eye (Lond). 2009;23:190–4.
ISO 10993-17, 2009. Biological evaluation of medical devices – Part 17: Establishment of allowable limits for leachable substances. https://www.iso.org/obp/ui/#iso:std:iso:10993:-17:ed-1:v1:en:en.
ISO 10993-5, 2009. Biological evaluation of medical devices – Part 5: Tests for in vitro 492 cytotoxicity. https://www.iso.org/obp/ui/#iso:std:iso:10993:-5:en.
Srivastava GK, Alonso-Alonso ML, Fernandez-Bueno I, Garcia-Gutierrez MT, Rull, Medina FJ, et al. Comparison between direct contact and extract exposure methods for PFO cytotoxicity evaluation. Sci Rep. 2018;8:1425.
Chang S, Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R. Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina. 1991;11:367–74.
Versura P, Cellini M, Torreggiani A, Bernabini B, Rossi A, Moretti M, et al. The biocompatibility of silicone, fluorosilicone and perfluorocarbon liquids as vitreous tamponades. Ophthalmologica. 2001;215:276–83.
Eckardt C, Nicolai U, Winter M, Knop E. Experimental intraocular tolerance to liquid perfluorooctane and perfluoropolyether. Retina. 1991;11:375–84.
Berglin L, Ren J, Algvere PV. Retinal detachment and degeneration in response to subretinal perfluorodecalin in rabbit eyes. Graefes Arch Clin Exp Ophthalmol. 1993;231:233–7.
Stolba U, Krepler K, Velikay-Parel M, Binder S. The effect of specific gravity of perfluorocarbon liquid on the retina after experimental vitreous substitution. Graefes Arch Clin Exp Ophthalmol. 2004;242:931–6.
Mackiewicz J, Maaijwee K, Lüke C, Kociok N, Hiebl W, Meinert H, et al. Effect of gravity in long-term vitreous tamponade: in vivo investigation using perfluorocarbon liquids and semi-fluorinated alkanes. Graefes Arch Clin Exp Ophthalmol. 2007;245:665–75.
Martinez-Reina MJ, Ruiz-Moreno JM, Montero JA, Rueda J. Histopathology and ultrastructure of rabbit retina after intravitreous injection of perfluorohexyloctane (F6H8). Curr Eye Res. 2005;30:773–9.
Ohira A, Wilson CA, deJuan E Jr, Murata Y, Soji T, Oshima K. Experimental retinal tolerance to emulsified silicone oil. Retina. 1991;11:259–65.
Pastor JC, Lopez MI, Saornil MA, Refojo MF. Intravitreal silicone and fluorosilicone oils: pathologic findings in rabbit eyes. Acta Ophthalmol (Copenh). 1992;70:651–8.
Soheilian M, Peyman GA, Moritera T, Wafapoor H. Experimental retinal tolerance to very low viscosity silicone oil (100 cs) as a vitreous substitute compared to higher viscosity silicone oil (5000 cs). Int Ophthalmol. 1995;19:57–61.
Sparrow JR, Ortiz R, MacLeish PR, Chang S. Fibroblast behavior at aqueous interfaces with perfluorocarbon, silicone, and fluorosilicone liquids. Invest Ophthalmol Vis Sci. 1990;31:638–46.
Chang S, Simpson RN. Impure perfluorocarbon liquids: a preventable tragedy. Retina. 2017;37:1019–20.
Menz DH, Feltgen N, Menz H, Müller BK, Lechner T, Dresp J, et al. How to ward off retinal toxicity of perfluorooctane and other perfluorocarbon liquids? Invest Ophthalmol Vis Sci. 2018;59:4841–6.
Ruzza P, Gatto C, Ragazzi E, Romano MR, Honisch C, D’Amato Tóthová J. H-content is not predictive of perfluorocarbon ocular endotamponade cytotoxicity in vitro. ACS Omega. 2019;4:13481–7.
Srivastava GK, Andrés-Iglesias C, Coco RM, Fernandez-Bueno I, Medina J, García-Serna J, et al. Chemical compounds causing severe acute toxicity in heavy liquids used for intraocular surgery. Regul Toxicol Pharm. 2020;110:104527.
Mertens S, Bednarz J, Richard G, Engelmann K. Effect of perfluorodecalin on human retinal pigment epithelium and human corneal endothelium in vitro. Graefes Arch Clin Exp Ophthalmol. 2000;238:181–5.
Inoue M, Iriyama A, Kadonosono K, Tamaki Y, Yanagi Y. Effects of perfluorocarbon liquids and silicone oil on human retinal pigment epithelial cells and retinal ganglion cells. Retina. 2009;29:677–81.
Mertens S, Bednarz J, Engelmann K. Evidence of toxic side effects of perfluorohexyloctane after vitreoretinal surgery as well as in previously established in vitro models with ocular cell types. Graefes Arch Clin Exp Ophthalmol. 2002;240:989–95.
Wenzel DA, Kunzmann BC, Druchkiv V, Hellwinkel O, Spitzer MS, Schultheiss M. Effects of Perfluorobutylpentane (F4H5) on Corneal Endothelial Cells. Curr Eye Res. 2019;44:823–31.
Dresp JH. Benchmarking different brands of silicone oils. Graefes Arch Clin Exp Ophthalmol. 2021;259:13–20.
Nakamura K, Refojo MF, Crabtree DV, Pastor J, Leong FL. Ocular toxicity of low molecular-weight components of silicone and fluorosilicone oils. Invest Ophthalmol Vis Sci. 1991;32:3007–20.
Mackiewicz J, Mühling B, Hiebl W, Meinert H, Maaijwee K, Kociok N, et al. In vivo retinal tolerance of various heavy silicone oils. Invest Ophthalmol Vis Sci. 2007;48:1873–83.
Romano MR, Groenwald C, Das R, Stappler T, Wong D, Heimann H. Removal of Densiron-68 with a 23-gauge transconjunctival vitrectomy system. Eye (Lond). 2009;23:715–7.
Author information
Authors and Affiliations
Contributions
MRR, RR and JDT contributed to the design of the review protocol, the correction of the draft, and the final revision. MF and IN conducted the search, screening potentially eligible studies, analysed the data, wrote the first draft. MF and DR created the tables. IN created Fig. 1. AGS and DR contributed to writing the first draft. LL and RM provided feedback on the draft and revised the final version. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Romano, M.R., Ferrara, M., Nepita, I. et al. Biocompatibility of intraocular liquid tamponade agents: an update. Eye 35, 2699–2713 (2021). https://doi.org/10.1038/s41433-021-01596-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01596-w
This article is cited by
-
Refinements in the use of silicone oil as an intraocular tamponade
Eye (2024)
-
A minimum specification dataset for liquid ocular endotamponades: recommendations by a European expert panel
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Unexplained visual loss in retinal detachment repair: comparing gas, silicone oil and heavy silicone oil by multivariable regression.
International Journal of Retina and Vitreous (2023)