Abstract
Purpose
To describe anterior chamber angle (ACA) structures and parameters in primary congenital glaucoma (PCG) and normal infant eyes, using Hand-held anterior segment optical coherence tomography (HH AS-OCT), as an in-office, non-contact technique.
Methods
Normal and PCG-infants <24 months were examined, using HH AS-OCT (RTVue RT- 100, Optovue Inc., Fremont, CA). Sedation was not required. Corneal pachymetry map, ACA width and iris thickness (IT) were measured. Trabecular meshwork (TM), Schlemm’s canal (SC), and scleral spur (SS) identification were assessed in both groups.
Results
Forty-eight infants; (26 PCG-eyes and 22 normal-eyes) aged 9.12 ± 6.7 months, were included. Nasal and temporal ACA width in PCG infants was found significantly larger (39.3 ± 6.6° vs. 30.4 ± 5.6, and 40.1 ± 5.3° vs. 32.5 ± 6.2 respectively) (p < 0.001). IT was significantly reduced (121.7 ± 43.9 μm in PCG-infants, vs. 160.3 ± 38.6 μm in normal-eyes) (p < 0.01). TM was identified in all normal eyes (100%) and nine (34.6%) PCG- eyes. SC was identified in 16 (72.7%) normal eyes versus four (15.4%) PCG. In PCG-eyes, an abnormal structure occluding the angle was seen in seven (26.9%), and a hyper-reflective membrane in five (19.2%), the iris was anteriorly inserted in all PCG-eyes, and iridotrabeculodysgenesis was clearly identified (with constant iris anterior insertion). The abnormal tissue obscuring the angle was seen in younger PCG-infants and iris thinning appeared to be part of the pathology, not a result of IOP elevation.
Conclusion
Using HH AS-OCT permits tomographic examination of the ACA in PCG infants and may help in the understanding of disease pathology. Hence, may assist in optimizing treatment.
Similar content being viewed by others
Introduction
Primary congenital glaucoma (PCG) is the most common glaucoma seen in infancy [1]. It accounts for 0.01–0.04% of blindness worldwide [2], the incidence of which is highly influenced by ethnicity and consanguinity [3].
Histological studies (from cadaver or enucleated eyes) have shown that in PCG, anterior chamber structures appear like an eye in the 7th or 8th month of gestation [4]. The iris and ciliary body (CB) fail to recede posteriorly; hence, overlapping the posterior portion of the trabecular meshwork (TM), and the longitudinal and circular fibers of the CB muscle insert into the TM rather than the scleral spur [4].
In presence of a clear cornea, such changes can be visualized through gonioscopy. However, for infants, this contact method requires sedation or examination under general anesthesia [5]. Gonioscopy is also considered subjective and requires specialized training [6]. Cross-sectional imaging of the anterior chamber provides quantitative data and may prove to be less subjective than gonioscopy. For this matter, anterior segment optical coherence tomography (AS-OCT) has the advantage, unlike ultrasound biomicroscopy (UBM), of being a non-contact method [7]. Inability of the infants to sit upright was an obstacle, but with the introduction of hand-held AS-OCT (HH AS-OCT), examination in the supine position became possible [8].
In 2017, Pilat and coworkers [8] looked into the possible benefits of examining children using a HH AS-OCT, however the report was limited to five cases with anterior segment dysgenesis (ASD), and only one with PCG. Apart from this work and an earlier retrospective report by Cauduro et al. in 2012, anterior segment imaging in PCG has not been thoroughly investigated [9].
The aim of this study was to identify and describe anterior chamber angle features and parameters in infants (2 years or less) with PCG and in normal infants, using HH-ASOCT as a diagnostic tool.
Patients and methods
This was a cross-sectional, descriptive study that was carried on 48 eyes of 48 infants (<24 months old) in the period from January 2018 till September 2018 at
Abuelrich pediatric hospital, Cairo University. The University Hospital Research Committee approved the study protocol. The study and data collection conformed to all local laws and were compliant with the principles of the Declaration of Helsinki. This was a convenient sample in which 26 infant eyes diagnosed with PCG were recruited from the pediatric glaucoma outpatient. Diagnosis of PCG was based on the Childhood Glaucoma Research Network classification [10] (CGRN) based on fulfilling two or more of the following (IOP > 21 mmHg, axial length showing myopic shift with increased ocular dimensions, cornea showing Haab striae, corneal diameter >11 mm in newborns, >12 mm in children younger than 1 year old and >13 mm in children older than 1 year and/or optic nerve progressive increase in cup/disc ratio). The control group included 22 eyes of 22 infants (<24 months of age) who came to the pediatric oculoplastic outpatient clinic complaining from lacrimation due to congenital nasolacrimal duct obstruction or mild congenital ptosis. To be included in the control group these infants had to have clear corneas with horizontal corneal diameter ranging from 10–11.5 mm, IOP ≤ 18 mmHg, normal fundus examination with no evidence of optic nerve cupping and a refractive error that is appropriate for their age. Both groups were consecutively enrolled, and the right eye was fixed for examination in the control group and in the PCG group with bilateral disease. In PCG group eyes who did not meet the inclusion criteria were excluded from the study.
All participants were thoroughly examined. Ophthalmological examination included measurement of intraocular pressure (IOP) using Perkins handheld applanation tonometry, corneal diameter measurements using calipers, anterior segment examination with handheld slit-lamp, and dilated fundus examination. Cycloplegic refraction was done for normal controls and attempted for PCG infants. Ultrasonography was done for PCG infants with hazy corneas obscuring clear visualization of the optic nerve. Axial length was estimated using B-scan for both groups. Anterior chamber (AC) depth was not measured as the device we used does not give an angle-to-angle image to allow for AC depth measurement. Infants with secondary glaucoma, history of previous intraocular surgery or history of trauma, were excluded from the study. We also excluded infants with densely opaque corneas that hindered visibility of the anterior chamber angle using HH AS-OCT.
Hand-held anterior segment optical coherence tomography (HH AS-OCT)
Using a non-contact technique, OCT was performed before the ophthalmologic examination to minimize potential artifacts. All the infants were examined with Fourier domain HH AS-OCT (RTVue RT- 100, Optovue Inc., Fremont, CA) with a scan rate of 26,000 axial scans/second, axial resolution of 5 μm, transverse resolution of 15 μm, and an add-on lens of the corneal adapter module (CAM-L mode: 6.0–2.0 mm). Observations were done by one examiner (DE). We applied the signal strength index (SSI) provided by the RTVue system to define scan quality. Images that were of poor SSI were excluded. SSI ≥ 35 was taken as a cutoff on a scale from 0–100. No sedation was necessary as most of the infants were imaged while spontaneously sleeping following being breast-fed or bottle-fed. As the HH-ASOCT is a non-contact method, examination was performed whilst gently holding the eyelids open. Anesthetic eye drops and eyelid speculum were not routinely used. We did not encounter problems with fixation, as we could gently manipulate the globe using a cotton-tipped applicator with a drop of topical anesthetic to provide us with reproducible images. All eyes were imaged in the room light without dilation.
Corneal thickness and Quantitative AC angle parameters
A pachymetry scan pattern, with 6-mm scan diameter and eight radials, was chosen to map the cornea. The RTVue corneal adapter module software provided the pachymetry map of total corneal thickness, automatically. When the corneal thickness was very high (beyond the capabilities of the device to provide a pachymetry map), measurements were taken manually. Three AS-OCT images were taken, scanning the angle at the 3 and 9 o’clock position. The average measurement for the angle was taken. Anterior chamber angle width was determined by measuring the degrees of the angle. The technique we used was similar to what was proposed by Pavlin and colleagues for measuring the ACA in UBM. Pavlin and colleagues proposed that the superior line be drawn through the trabecular meshwork and the inferior one along the anterior iris surface [11]. The iris thickness was measured manually in three positions: near the iris root, in the middle, and near the pupillary border. Three measurements were taken for each point then the average was calculated. This methodology of measuring the iris thickness in three locations was novel to this study. However, a previous study by Pilat et al. did quantitative assessment of the thickness of the iris using image J, they calculated the averaged iris thickness/area from the pupil to a point 2400 μm temporally/nasally [12].
Angle morphology
Examination of the anterior chamber angle structures was done. The scleral spur (SS) was identified as the prominent inner extension of the sclera (its thickest part). When it was not clearly identifiable, its anatomical location at the junction between the inner wall of TM and the sclera was utilized. Identification of SS was considered a very important anatomical landmark for the trabecular meshwork, located ≈250–500 μm anterior to the SS.
Statistical analysis
Data entry, processing and statistical analysis was carried out using MedCalc ver. 15.8. (MedCalc, Ostend, Belgium). Comparison between the two groups as regards basic clinical data and angle development was done using Student’s t and Chi square tests. Correlation studies between different ophthalmological data e.g., iris thickness, angle width, angle development data, corneal diameter, and corneal thickness; and its relative independent effectors (e.g., age and IOP) were conducted using logistic regression analysis and Pearson’s correlation coefficient. Paired comparative studies for both groups were done using ANOVA (analysis of variance) test which was Bonferroni corrected. Repeated measures ANOVA test (2-Factor study) was used for combined paired and unpaired comparative studies. ROC curve analysis was used to assess the sensitivity, cutoff point, AUC (means accuracy %) of HH-ASOCT and to measure its diagnostic accuracy in diagnosing PCG infants. Data were presented and suitable analysis was done according to the type of data (parametric and non-parametric) obtained for each variable. P values less than 0.05 (5%) was considered to be statistically significant.
Results
The current study included 48 eyes of 48 infants. Twenty-six eyes of 26 infants were diagnosed with PCG with a mean age of 9.3 ± 6.7 months and, a mean IOP measurement of 22.84 ± 6.27 mmHg. Twenty-two eyes of 22 normal infants with a mean age of 8.7 ± 7.2 months and a mean IOP measurement of 10.4 ± 1.33 mmHg. There was no statistically significant difference between the PCG and normal controls regarding both age and sex (p = 0.761, p = 0.628 respectively). The horizontal corneal diameter
(HCD) was 13.11 ± 1.14 mm in the PCG eyes versus 10.22 ± 0.97 mm in the normal eyes. The mean axial length in the PCG eyes was 20.75 ± 1.06 mm versus 18.34 ± 1.047 mm in the normal eyes. The spherical equivalent refraction of the normal infants ranged from +4.0 to +1.5 diopters. The central corneal thickness (CCT) as measured by the corneal pachymetry map, using the HH AS-OCT was 577.4 ± 54.8 μm in the PCG eyes versus 536.3 ± 36.4 μm in the normal ones.
Anterior chamber angle width and the iris thickness using HH-ASOCT
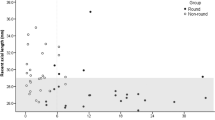
Using Student’s t-test, the mean IT near the iris root was 121.7 ± 43.9 μm in PCG infants, which was significantly thinner than mean IT near the iris root in normal eyes (160.3 ± 38.6 μm). Anterior chamber angle width in the nasal and temporal angles was also found to be significantly larger in PCG eyes than normal eyes (Table 1, Fig. 1).
Angle description using HH AS-OCT
In normal infants, SC was identified in 16 eyes (72.7%), SS was well identified in five eyes (22.7%) and poorly identified in 15 eyes (68.2%), TM was identified in all the eyes. None of the normal eyes showed any trabecular dysgenesis or anterior iris insertion. Whereas in PCG-eyes, only four eyes (15.4%) had an identified SC, SS was poorly identified in five eyes (19.32%) and well identified in two eyes (7.69%), nine eyes (34.6%) had an identified TM, seven eyes (26.9%) showed an abnormal structure obscuring the angle, five eyes (19.2%) had a hyper reflective membrane, and all of the cases of PCG showed anterior insertion of the iris (Figs. 2, 3).
Anterior chamber nasal and temporal angles as imaged by RTVue handheld anterior segment optical coherence tomography (RTVue HH-ASOCT) in a normal infant (A, B), versus in PCG (C, D, E, F). In normal infants, scleral spur (SS) could be detected, trabecular meshwork was identified (TM), and Schlemm’s canal (SC) was seen (A, B). Anteriorly inserted, thinned out iris, with severe trabeculodysgenesis and no identifiable angle structures as seen in a primary congenital glaucoma infant (blue arrow in C, D). An abnormal membrane clearly visualized extending from the iris to the trabecular meshwork (blue arrow in E, F), in another primary congenital glaucoma infant.
Nasal and temporal anterior chamber angles imaged by the RTVue handheld anterior segment optical coherence tomography (RTVue HH-ASOCT) in primary congenital glaucoma infants showing a hyper reflective membrane extending from the iris to the trabecular meshwork (blue arrow in A, B), Abnormal tissue was visualized occluding the angle (blue arrow in C, D). All the images show an anteriorly displaced thinned out iris.
Correlation studies between different ophthalmological data e.g., iris thickness, angle width, angle development data, corneal diameter, and corneal thickness; and its relative independent effectors (e.g., age and IOP) were conducted using logistic regression analysis and Pearson’s correlation coefficient for PCG infants.
Pearson’s correlation analysis showed that; Iris thickness (nasal, and temporal root) had a moderate positive correlation with age with significant statistical difference (p = 0.0233, r = 0.48, p = 0.035, r = 0.49 respectively). Nasal pupillary border IT and mid-temporal IT had a moderate negative correlation with HCD in both groups; with a significant statistical difference (p < 0.05). IT (nasal near pupillary border) and IT (mid temporal), had a moderate negative correlation with axial length in glaucoma group only; with highly significant statistical difference (p = 0.0034, r = −0.46, p = 0.033, r = −0.489 respectively). However, no correlation was found between the iris thickness and IOP. Angle width (Nasal) and Angle width (Temporal) had a moderate positive correlation with HCD in both groups; with highly significant statistical difference (p = 0.0047, r = 0.4, p = 0.006, r = 0.39 respectively). Pearson’s correlation analysis also showed that abnormal structure seen at the angle had a significant negative correlation with age in PCG group with significant statistical difference (p < 0.05).
To demonstrate the sensitivity and specificity of HH-ASOCT in separating PCG from normal eyes, ROC-curve analysis of the angle width and IT was carried to predict eyes with PCG from eyes without (Table 2). ROC-curve analysis showed that the Iris thickness (Nasal Near pupillary border) at a cutoff point (≤180 μm) predicted eyes with PCG with good accuracy (86%), sensitivity = 71% and specificity = 100% (p < 0.001). Also, the iris thickness (Temp Near pupillary border) at a cutoff point (≤231 μm) predicted eyes with PCG from eyes without, with excellent accuracy (90%), sensitivity = 93% and specificity = 76% (p < 0.001). Angle width (Nasal) at a cutoff point (>33.04°) predicted eyes with PCG from eyes without, with good accuracy (85%), sensitivity = 91% and specificity = 72% (p < 0.001). Angle width (Temp) at a cutoff point (>35.3°) predicted eyes with PCG from eyes without, with good accuracy (83%), sensitivity = 80% and specificity = 76% (p < 0.001).
Discussion
Optical coherence tomography (OCT) is a high-resolution non-invasive imaging technique, in which tissue observation occurs through sectional cuts of the ocular structure. Anterior segment imaging using this technology (AS-OCT), has remarkably improved over the past years, especially through the development of higher resolution systems considering time domain and Fourier-domain systems [13, 14].
Despite its multiple applications in the adult population, the role of AS-OCT in pediatric ophthalmology is still not well reported [15]. The challenging nature of the anterior segment anatomy of children was kept restricted to the use of UBM, which used immersion technique in a sedated child [16]. Inability of the infants and young children to sit upright to be examined by OCT was also an obstacle, this obstacle was bypassed by HH AS-OCT [7].
Our study used HH AS-OCT to examine the anterior segment and anterior chamber angle structures in both normal and PCG infants. To our knowledge, our study is the first to describe these features using HH AS-OCT in infants; both normal and glaucomatous. Previous studies focused on older children and with the exception of Pilat’s report in 2019. Older studies only reported on very limited numbers [7,8,9]. Pilat and coworkers [12] compared 22 PCG-patients with an average age of 4.4 years to a control group using a handheld SD-OCT device (Envisu 2300, Leica Microsystems, Germany). Their study focused mainly on describing corneal and iris changes in PCG, however our study gave detailed description of the angle structures in PCG infants as well as in normal infants.
We used the corneal pachymetry map produced by HH AS-OCT to measure the CCT in both PCG- and normal infants. The mean CCT in PCG infants was found to be significantly higher than in normal infants which was consistent with the findings of Pilat’s work [12]. However, the measurements in our study group were greater for both PCG affected eyes and normal ones (577.4 ± 54.8 μm in the PCG and 536.3 ± 36.4 μm in normal vs. 453.59 ± 62.72 and 437.07 ± 30.84 in Pilat’s study). This may be partly explained by the fact that none of our patients had received any pressure reducing procedures or medications at the time of examination, and partly by the age difference between both studies. Other potential confounding factors included machine operation differences and ethnicity.
The ACA width was determined by measuring the angle in degrees. One of the technical difficulties encountered, was placement of the apex and edge points because of variations in iris configuration, making the angle measurements rather subjective. Anterior chamber angle examination was carried on the nasal and temporal quadrants at the 3 o’clock and the 9 o’clock positions. These positions were chosen depending on the previous work by Lisandro et al., to identify the position of the SS; which showed that the location of SS in AS-OCT images was less detectable in the superior and inferior quadrants compared with the nasal and temporal ones [17]. Since the determination of the angle apex and angle sides is quite examiner-dependent, the reproducibility of anterior chamber angle measurements is questionable [11]. To avoid this limitation in our study, we took three measurements for each nasal and temporal angle and the average was calculated. However, defining the angle in degrees is to a great extent dependent on the shape and the configuration of the iris.
The angle width was found to be significantly larger in PCG infants confirming the histopathological description of PCG as an open angle glaucoma [18]. This finding is in agreement of what was previously described by Cauduro et al., on two eyes of PCG, in which they stated that they presented by wide angle, increased AC depth (3.75 mm), and inner anterior chamber diameter (13.66 mm) [9].
Concerning the iris thickness measurements in our study, it showed a significantly thinner iris in PCG infants, in the three points tested: near the iris root, in the middle and near the pupillary border. IT significantly negatively correlated to both axial length and HCD measurements, but it did not show any correlation with the IOP measurements. This could be partly attributed to increased diameter of the iridociliary structures which happens in PCG and partly to iris dysgenesis, being part of the pathology, rather than a result of elevated IOP. Similarly, Pilat found no significant correlations between the mean iris thickness and any of their clinical or demographic parameters [12]. Also, we found that the flat configuration of the iris together with its anterior insertion was clearly visualized in all cases of PCG. In some cases, the anterior iris insertion hid the angle structures and the iris seemed to insert directly into the TM.
These findings agreed with the histopathological changes, which had found the iris to be flat [19]. The iris periphery may be circumferentially tented anteriorly with anterior position of the visible posterior iris pigment layer [20]. Such forward tenting of the iris was previously described in 50% of PCG patients. Also, the smooth continuity of the anterior surface of the peripheral iris with the TM with or without tenting, seemed an important observation in PCG [21]. We also reported that IT (nasal, and temporal root) had a significant moderate positive correlation with age in both groups. This finding matched the conclusion of Nakakura et al., who stated that the IT increased with age in children. They studied the iris thickness in 41 children using swept source anterior segment OCT [22].
Regarding angle development in normal infants, SS was well identified in five eyes (22.7%) and was poorly identified in 15 (68.2%) eyes. Scleral spur location could be determined in 72% of the images in a cross-sectional observational study that used Visante; Carl Zeiss OCT, their study included 502 adult participants with no previous ophthalmic problems [17]. Again, by comparing our results to the histopathological changes previously described, SS was not frequently described in PCG, Shaffer described SS to be less prominent. The infrequent description of SS aroused the possibility of its near absence on pathologic examination, which could have an effect on the outflow of aqueous [4]. Barkan, was the first to describe the presence of a semitransparent membranous vertically oriented TM between the cornea and the anteriorly inserted iris [23]. In Our study five eyes (19.2%) had a hyper reflective membrane crossing the angle, from the iris to the area of TM and all of the cases of PCG showed anterior insertion of the iris.
Our study had some limitations, namely the small sample size and defining the angle in degrees, which is subjective to variations in iris configuration. Also, we were missing further quantitative measurements of the angle, which required special software that was not present in the device we used (RTVUE HH-OCT). We had some imaging artifacts from the eyelids and/or the manipulations; especially that imaging was done in naturally sleeping infants. Imaging difficulties due to cornea opacities or large globes were also encountered. Also, one of the limitations of our study was that the image grader was not masked to the diagnosis.
Our study showed that measuring the nasal and temporal angle widths as well as the iris thickness near the pupillary border using the HH-ASOCT can predict eyes with PCG from eyes with high sensitivity and specificity. Current findings confirmed that
PCG is a congenital open angle glaucoma. Iridotrabeculodysgenesis is clearly identified (with constant iris anterior insertion). Iris thinning could be a part of the pathology not a result of IOP elevation. The abnormal tissue obscuring the angle was seen in PCG infants of younger age. This could be of great help in understanding the pathophysiology of the disease, thus selecting the best surgical techniques. In conclusion, using HH AS-OCT, in office, is a helpful tool in the diagnosis and management of PCG. It may also help in predicting the prognostic factors for surgical success by correlating the OCT findings with the severity of the disease in addition, being a non-contact method that requires no sedation or anaesthesia it can be safely added to the diagnostic tools of PCG. Further studies should be conducted to assess the benefits of HH-ASOCT in describing postoperative angle changes following angle surgeries in PCG.
What was known before
-
Imaging anterior chamber angle in adults was performed using UBM or AS-OCT, but no data were available in infants having PCG.
What this study adds
-
Using HH AS-OCT permits, in office, thorough examination of the ACA in PCG infants and helps in understanding disease pathology, hence may assist in optimizing treatment.
References
Papadopoulos M, Cable N, Rahi J, Khaw PT.The BIG eye study investigators The British infantile and childhood glaucoma (BIG) eye study. Invest Ophthalmol Vis Sci. 2007;48:4100–6.
Mandal A, Chakrabarti D. Update on congenital glaucoma. Indian J Ophthalmol. 2011;59:148–57.
Chang TC and Cavuoto KM. Surgical management in primary congenital glaucoma: four debates. J Ophthalmol. 2013;2013:612708.
Maumenee AE. The pathogenesis of congenital glaucoma. A New Theory. Trans Am Ophthalmol Soc. 1958;56:507–70.
DeLouise VP, Anderson DR. Primary infantile glaucoma. Surv Ophthalmol. 1983;28:1–19.
Krishnadas R, Ramakrishnan R. Congenital glaucoma. a brief review. J Curr Glaucoma Pract. 2008;2:17–25.
Ahmed IIK. Anterior segment optical coherence tomography in glaucoma. J Curr Glaucoma Pract. 2009;3:14–23.
Pilat AV, Sheth V, Purohit R, Proudlock FA, Anwar S, Gottlob I. Hand‐held optical coherence tomography imaging in children with anterior segment dysgenesis. Acta Ophthalmol 2017;95:537–41.
Cauduro RS, Amaral Ferraz C, Morales MSA, Garcia PN, Lopes YC, Souza PH, et al. Application of anterior segment optical coherence tomography in pediatric ophthalmology. J of Ophthalmol. 2012;2012:6.
Thau A, Lloyd M, Freedman S, Beck A, Graejewski A, Levin AV. New classification system for pediatric glaucoma:implications for clinical care and a research registry. Curr Opin Ophthalmol. 2018;29:385–94.
Pavlin CJ, Harasiewicz K, Foster FS. Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol. 1992;113:381e9.
Pilat AV, Proudlock FA, Shah S, Sheth V, Purohit R, Abbot J, et al. Assessment of the anterior segment of patients with primary congenital glaucoma using handheld optical coherence tomography. Eye 2019;33:1232–9.
Izatt JA, Hee MR, Swanson EA, Lin CP, Huang D, Schuman JS, et al. Micrometer-scale resolution imaging of the anterior eye in vivo with optical coherence tomography. Arch Ophthalmol 1994;112:1584–9.
Ramos JLB, Li Y, Huang D. “Clinical and research applications of anterior segment optical coherence tomography—a review,”. Clin Exp Ophthalmol. 2009;37:81–89.
Shields CL, Mashayekhi A, Luo CK, Materin MA, Shields JA. Optical coherence tomography in children: analysis of 44 eyes with intraocular tumors and simulating conditions. J Pediatr Ophthalmol Strabismus. 2004;41:338–44.
El Shakankiri NM, Bayoumi NH, Abdallah AH, El Sahn MMF. Role of ultrasound and biomicroscopy in evaluation of anterior segment anatomy in congenital and developmental cataract cases. J Cataract Refract Surg. 2009;35:1893–905.
Sakata LM, Lavanya R, Friedman DS, Aung HT, Seah SK, Foster PJ, Aung T. Assessment of the scleral spur in anterior segment optical coherence tomography images. Arch Ophthalmol. 2008;126:181–5.
Merin S, Morin D. Heredity of congenital glaucoma. Br J Opthalmol. 1972;56:414417.
Maumenee AE. Surgery for congenital glaucoma-symposium on glaucoma. St Louis. 1959; CV Mosby Co, p. 212.
Shaffer RN. Pathogenesis of congenital glaucoma gonioscopic and microscopicanatomy. Trans Am Acad Ophthalmol Otolaryngol. 1955;59:297–308.
Chandler PA, Grant WM. Lectures on glaucoma. Philadelphia. Lea & Febiger 1965;315–6.
Nakakura S, Nagata Y, Shimizu Y, Kawai A, Tabuchi H, Kiuchi Y. Determination of iris thickness development in children using swept-source anterior-segment optical coherence tomography. PLoS One. 2019;14:e0217656.
Barkan O. Surgery of congenital glaucoma. Am J Ophthalmol. 1953;36:1523–33.
Acknowledgements
The authors wish to acknowledge Dr. Hala Elhilali, professor of Ophthalmology, Cairo University, for her valuable assistance and continuous guidance. Other Acknowledgments: None.
Author information
Authors and Affiliations
Contributions
WA performed the literature review, tabulated the data, and drafted the manuscript. AFE collected the clinical data, drafted and revised the manuscript. GG contributed to the study design, analyzed the data, and revised the manuscript. DEl-F contributed to the study design, cleaned and analysed the data, wrote, and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdeen, W., Esmael, A.F., Gawdat, G. et al. Anterior chamber angle features in primary congenital glaucoma infants using hand-held anterior segment-oct. Eye 36, 1238–1245 (2022). https://doi.org/10.1038/s41433-021-01583-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01583-1
This article is cited by
-
The correlation of anterior segment structures in primary congenital glaucoma by ultrasound biomicroscopy with disease severity and surgical outcomes
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)