Abstract
Objectives
To investigate the results of partial lamellar sclerouvectomy (PLSU) for anteriorly located uveal tumours.
Methods
We reviewed the tumour features, histopathologic findings, complications, visual acuity outcomes, eye preservation, metastasis, and mortality data of 56 cases with uveal tumours who underwent PLSU between February 1999 and February 2019.
Results
The mean largest tumour base diameters were 5.8 × 3.4 mm and the mean tumour thickness was 3.3 mm. Histopathologically, 30 (53.6%) eyes had malignant melanoma, 13 (23.2%) had nevus, 5 (8.9%) had iris stromal cyst, 4 (7.1%) had melanocytoma, 2 (3.6%) had Fuchs’ adenoma, 1 (1.8%) had iris pigment epithelial cyst, and 1 (1.8%) had invasive breast cancer metastasis. The most common postoperative complications included cataract in 21 (37.5%) eyes, vitreous haemorrhage in 15 (26.8%), scleral thinning in 10 (17.9%), and hyphema in 6 (10.7%). At a mean follow-up of 40.4 (range: 10–201) months, tumour recurrence was observed in 2/30 (6.7%) eyes with melanoma and 1/5 (20.0%) eye with iris stromal cyst. Eyes with recurrent melanoma were treated with enucleation. Liver metastasis developed in only 1 (3.3%) melanoma case. All patients were alive at the end of follow-up.
Conclusions
PLSU is a successful treatment method for many anteriorly located uveal tumours. In our series, the overall tumour recurrence and globe salvage rates were 5.4% and 96.4% respectively. Among melanoma cases, the metastasis rate was 3.3% and survival rate was 100%.
Similar content being viewed by others
Introduction
Surgical resection of uveal tumours has been used for uveal melanomas and other tumours of indeterminate diagnosis. There are two main resection techniques for intraocular tumours: exoresection and endoresection [1, 2]. Endoresection is usually done for tumours located posterior to the equator and without ciliary body involvement. On the other hand, exoresection is suitable in iris, ciliary body, and ciliochoroidal tumours [3].
Several investigators reported exoresection techniques under different names such as partial lamellar sclerouvectomy (PLSU), transscleral local resection, eye wall resection, and block excision [4,5,6,7,8]. There are several indications for PLSU surgery [1, 4, 8, 9]. First, removal is indicated for iridociliary tumours of indeterminate diagnosis that present with suspicious features, including pigment seeding, prominent vascularity, and increased thickness and base diameter. Second, iridociliary tumours with progressive course and documented growth, including leiomyoma, melanocytoma, and iris cysts need to be excised to prevent cataract, lens subluxation, corneal endothelial contact, and glaucoma. Third, plaque radiotherapy or proton beam radiotherapy for iridociliary melanomas may not be readily available in developing countries. Surgical resection may provide an alternative means of treatment in iris, ciliary body, and ciliochoroidal melanomas with tumour base diameter <15 mm and <3 clock hours of limbal involvement. Fourth, ciliochoroidal melanomas ≥8 mm in thickness require high radiation doses to the tumour, resulting in severe radiation complications. Surgical resection may be preferable under these circumstances.
Herein, we report our 20-year experience of PLSU in anteriorly located uveal tumour cases with respect to tumour features, histopathology, complications, visual acuity outcomes, eye preservation, metastasis, and mortality.
Materials and methods
We reviewed the clinical records of 56 patients with 56 affected eyes who underwent PLSU and follow-up from February 1999 to February 2019. The study was conducted according to the tenets of the Helsinki Declaration and approved by the Ethics Committee of Ankara University, Faculty of Medicine (Approval number: İ2-48-19). All patients underwent visual acuity and intraocular pressure (IOP) measurement, biomicroscopy and dilated fundus examination with indirect ophthalmoscopy. Tumour base diameter and thickness were determined by indirect ophthalmoscopy, A and B mode ultrasonography (USG), ultrasound biomicroscopy (UBM), and anterior segment optical coherence tomography depending on tumour location. Outcomes were tumour features, histopathologic examination results, visual acuity, complications, eye preservation, metastasis, and death. The frequency of complications in the first and second 10-year periods of our study were compared to each other.
The requirements for tumour removal using PLSU were as follows: (1) Iris, iridociliary, ciliochoroidal, and iridociliochoroidal melanomas diagnosed by clinical examination, USG, UBM, and anterior segment/fundus photography, (2) Anterior uveal tumours/cysts with pigment dispersion leading to IOP increase, prominent tumour vascularity, documented growth, associated cataract and corneal endothelial decompensation, (3) Tumour base diameter <15 mm and involving <3 clock hours of corneal limbus and (4) Patient desire to have the intraocular tumour removed rather than followed up with observation despite absence of compelling evidence for malignancy or growth.
The decision to proceed with PLSU versus plaque radiotherapy in cases with clinically established uveal melanoma diagnosis was made based on the discussion with the patients and their families. The patients were informed that glaucoma, retinopathy, and optic neuropathy rates were higher after plaque radiotherapy; retinal detachment (RD) and local tumour recurrence rates were higher after PLSU. Globe salvage, metastasis, and mortality rates were similar in both treatment groups. Risks of hypotensive general anaesthesia including death, stroke, heart attack, and cognitive function deficits were discussed with the patient. Many patients opted for plaque radiotherapy during the same period.
The surgical procedure in all cases was performed by the same surgeon (AKG) and involved a tedious and long learning curve [9]. Hypotensive general anaesthesia was used to keep the systemic blood pressure low. Informed consent was obtained from all cases including the complications that may occur from hypotensive general anaesthesia and PLSU surgery. Most patients underwent cardiology consultation to reveal any risk factors for hypotensive general anaesthesia. The hypotensive general anaesthesia protocol involved premedication with intravenous midazolam or an intramuscular mixture of aldolan and atropine. Subsequently, anaesthesia was given with a sleep dose of intravenous propofol followed by intermittent positive pressure ventilation with a mixture of air/oxygen and sevoflurane. Rocuronium was used for muscle relaxation and fentanyl for analgesia. Blood pressure was reduced slowly by titrating an infusion of sodium nitroprusside, remifentanil, or esmolol. Monitoring included electrocardiography, saturation, blood pressure, capnography, and depth of anaesthesia. Arterial catheterisation was performed by the anaesthesiologist for close blood pressure monitoring in patients with a cardiac medical history.
A slightly reverse Trendelenburg position was preferred to reduce bleeding. After a Williams lid speculum was inserted, a 270° limbal peritomy was done. Two/three rectus muscles around the area of the tumour were hooked and isolated with 2-0 silk sutures. If the tumour was under one of the rectus muscles, the overlying muscle was disinserted using a double-armed 6-0 vicryl suture. Using blunt dissection with Steven’s scissors, the conjunctiva and Tenon’s fascia were separated away from the globe in the quadrant of the tumour. Episcleral blood vessels were cauterised using bipolar diathermy. The margins of the tumour were localised by transillumination and outlined with a marking pencil around the tumour shadow. Subsequently, the margins of the anteriorly hinged scleral flap positioned 3–4 mm outside this mark were outlined on the sclera. The shape of the scleral flap was rectangular or hexagonal in most cases. With a #57 beaver blade, a groove was created to ~80–90% thickness of the sclera, and the scleral flap was then dissected and carried anteriorly to the corneoscleral limbus (Fig. 1a). Any bleeding from emissary vessels was controlled with bipolar cautery. If the tumour was in the iridocorneal angle, its shadow overlapped with the shadow of the pars plicata. In this case, the posterior margin of the tumour was marked at the posterior boundary of the pars plicata.
Partial lamellar sclerouvectomy technique for uveal tumours (a–d). a Creation of 80–90% thickness scleral flap with # 57 beaver knife. b Cutting through the sclera to expose the uveal tumour. c Excision of the tumour using a no-touch technique with Vannas scissors. d Suturing of the scleral flap back to its original position using 9–0 nylon sutures. Iridociliary melanoma (e–i). e Anterior segment photograph before partial lamellar sclerouvectomy shows the superiorly located iridociliary melanoma. f Anterior segment photograph 5 months after partial lamellar sclerouvectomy shows the broad peripheral iridectomy superiorly. g Histopathological examination after partial lamellar sclerouvectomy shows an infiltrative tumour originating from the iridociliary area. Ciliary processes (vertical arrow) and iris tissue (horizontal arrow) are visible in the upper right corner of the figure (haematoxylin and eosin stain × 2.2). h Histopathological examination after partial lamellar sclerouvectomy shows atypical pleomorphic epithelioid cells with a large and round oval vesicular nucleus containing a prominent large nucleolus. Melanin pigment and mitosis are also present (arrow) (haematoxylin and eosin stain × 89). i Immunohistochemical examination shows that many cells show nuclear Ki67 staining (horizontal and vertical arrows) (Ki67 × 50.7). These findings were consistent with a mixed spindle-epithelioid (predominantly epithelioid) cell uveal melanoma.
When the scleral flap was fully developed, transillumination was repeated. The margins of the tumour were outlined on the remaining inner scleral tissue with a marking pencil. At this point, ~1 ml of core vitreous was aspirated in a syringe using either a 22-gauge (G) needle or 23/25 G cutter operating in a single port 23/25 G pars plana vitrectomy (PPV) setup. A small circumferential incision using a 15° microsurgical knife was then made on the inner scleral fibres about 2–3 mm outside the margins of the tumour. Then, Vannas scissors were used to incise the sclera until the uveal tract was exposed (Fig. 1b). The uveal tract was cauterised using bipolar cautery until blanching and a grey colour change of the uveal tissues was achieved.
In uveal tumours involving the iris, a paracentesis port in the limbus was created ~90° from the area of the main incision, and viscoelastic was injected into the anterior chamber. The anterior chamber was then entered using a 15° microsurgical knife at the centre of the flap area, and the corneoscleral incision was laterally extended with Westcott scissors.
Subsequently, the uveal tumour was excised using a no-touch technique using Vannas scissors (Fig. 1c). The choroidal/ciliary part of the tumour was excised first, followed by excision of the iris part if the tumour had an iris component. The pupillary rim was spared, if possible. Care was taken to leave the underlying retina or, in the case of ciliary tumours, the nonpigmented ciliary pigment epithelium intact. The uveal tumour together with the overlying scleral fibres was carefully lifted off the surgical field using a ‘no-touch technique’ to avoid spilling tumour cells into the surgical field. If vitreous loss occurred, vitreous was removed with a 23 G cutter at the scleral surface. Following completion of the vitrectomy, the scleral flap was sutured to its original position with 9-0 nylon sutures (Fig. 1d). Balanced salt solution was injected into the eye via the limbal paracentesis port or through the pars plana to adjust the IOP, if necessary. Cellulose sponges were used to check if the wound was watertight. If there was any leak, more 9-0 nylon sutures were placed. At the end of scleral closure, dry vitrectomy for any remaining vitreous fibres at the wound edges was done with the 23/25 G cutter. Any previously detached rectus muscle was sutured to its original position/insertion, and the conjunctiva was reapproximated to the limbus with 7-0 vicryl sutures.
We performed adjunctive Ruthenium-106 (Ru-106) plaque radiotherapy with a 20 mm or 25 mm round plaque 1 month after PLSU in uveal melanoma cases with predominant ciliary body and choroidal involvement. We did not do plaque radiotherapy in melanomas where the main location of the tumour was in the iris with limited involvement of the adjacent ciliary body. We aimed to deliver an apex dose of 100 Grey to a 1 mm depth from the inner surface of the sclera during plaque radiotherapy.
Statistical analysis
All statistical analyses were performed using SPSS for Windows version 11.5 (SPSS Inc, Chicago, IL, USA). Normally distributed continuous variables were expressed as mean ± standard deviation while the continuous variables that do not have normal distribution were expressed as median (minimum-maximum). Also, categorical variables were summarised as counts (percentages). The comparison of complication rates between the first and second 10-year periods of our study was made with Pearson Chi-Square test and p value < 0.05 was considered as statistically significant.
Results
A total of 56 patients underwent PLSU for anteriorly located uveal tumours. Thirty (53.6%) patients were female and 26 (46.4%) patients were male. The mean age at presentation was 47.6 (19–83) years. Thirty-five cases presented with externally visible intraocular tumour, 14 with pain in the eye, and 7 with decreased vision. The tumour was located in the left eye in 36 (64.3%) cases and in the right eye in 20 (35.7%) cases.
Mean preoperative visual acuity was 0.60 (range: 0–1.9) and 20/80 (range: 20/20–20/1600) on the logMAR and Snellen scales, respectively. The tumour was located in both the iris and ciliary body in 23/56 (41.1%) eyes, in the iris/iridocorneal angle in 18/56 (32.1%), in the ciliary body in 8/56 (14.3%), in the ciliary body and choroid in 4/56 (7.1%), and in the iris, ciliary body, and choroid in 3/56 (5.4%). The tumour location was in the superior quadrant in 18/56 (32.1%) eyes, temporal quadrant in 14/56 (25.0%), inferior quadrant in 14/56 (25.0%), and nasal quadrant in 10/56 (17.9%). The mean largest tumour base diameters were 5.8 × 3.4 (range: 10.2 x 2.5) mm and the mean tumour thickness was 3.3 (range: 1.0–7.0) mm. In melanoma cases, the mean tumour thickness was 4.8 (range: 2.1–7.0) mm. Tumour thickness was ≥5 mm in 21 melanoma cases and <5 mm in 9. In non-melanoma cases, tumour thickness was ≥5 mm in 2 and <5 mm in 24. There was no retinal invasion in any of the eyes. Seven of 56 (12.5%) eyes had focal cataract corresponding to the tumour location.
PLSU was performed for clinically diagnosed uveal melanoma in 22/56 (39.3%) eyes. In 28/56 (50.0%) eyes, the diagnosis of uveal melanoma could not be ruled out or certain tumour features including pigment seeding with IOP increase, prominent vascularity, and associated cataract necessitated removal. Finally, PLSU surgery was performed for recurrent iris stromal cyst in 5/56 (8.9%) eyes and breast cancer metastasis in 1/56 (1.8%) eye. All 5 cases diagnosed with iris stromal cyst had failed previous aspiration/alcohol irrigation and demonstrated recurrence (Fig 2e). The patient with breast cancer metastasis had no other metastatic site and refused ocular external radiotherapy.
Total excision of the lesion with a narrow rim of surrounding healthy tissue was performed in all cases (Figs. 1e, f, 2a–d). Five out of 30 (16.7%) eyes with ciliary/ciliochoroidal/iridociliochoroidal melanoma underwent adjunctive Ru-106 plaque radiotherapy. Histopathologic examination revealed malignant melanoma in 30/56 (53.6%) eyes (Fig. 1g–i), nevus in 13/56 (23.2%) (Fig. 2g–j), iris stromal cyst in 5/56 (8.9%) (Fig. 2f), melanocytoma in 4/56 (7.1%), Fuchs’ adenoma in 2/56 (3.6%), iris pigment epithelial cyst in 1/56 (1.8%), and invasive breast cancer metastasis in 1/56 (1.8%). Melanoma cell type was spindle in 17/30 (56.7%) eyes, epithelioid in 7/30 (23.3%), and mixed in 6/30 (20.0%).
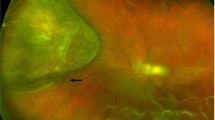
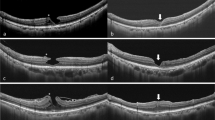
Iris melanoma (a, b). a Anterior segment photograph before partial lamellar sclerouvectomy shows an inferotemporally located pigmented iris melanoma in a pseudophakic eyes. b Anterior segment photograph at 3 months after partial lamellar sclerouvectomy shows the peripheral iridectomy area after complete tumour removal with sparing of the pupil. Traumatic iris stromal cyst (c–f). c Anterior segment photograph shows inferiorly located iris stromal cyst touching the corneal endothelium. Corneal opacification from prior trauma and possible endothelial decompensation is seen. d Anterior segment photograph 3 months after partial lamellar sclerouvectomy shows the inferior total iridectomy after complete cyst removal. e Swept-source anterior segment optical coherence tomography before surgery shows old corneal penetration site, defect in the corneal endothelium and posterior stroma, and anterior cyst wall touching the corneal endothelium. f Histopathological examination after partial lamellar sclerouvectomy shows the benign cystic formation in the iris stroma (star) (haematoxylin and eosin × 12.8). Histopathological examination of ciliary body nevus after partial lamellar sclerouvectomy (g–j). The tumour was excised because the possibility of melanoma could not be ruled out. g Ciliary body melanocytic lesion with ciliary processes on the right side of the figure (arrow) (haematoxylin and eosin × 6.7). h The bland looking melanocytic cells contain an oval nucleus with thin chromatin and no nucleolus (haematoxylin and eosin × 63). i After the melanin-bleaching, bland cells displaying no mitosis are more clearly visible (×90.5). j Immunohistochemical examination shows that the Ki67 proliferation index of the melanocytic cells forming the lesion is <1%, nuclear staining (arrow) is observed in 1 cell with Ki67 (Ki67 × 28.1).
Preoperative diagnosis was confirmed by histopathological examination in 22 melanoma, 5 iris stromal cyst, and 1 breast cancer metastasis cases after PLSU. Histopathological examination of the remaining 28 cases undergoing PLSU revealed nevus in 13 cases, melanoma in 8 cases, melanocytoma in 4 cases, Fuchs’ adenoma in 2 cases, and iris pigment epithelial cyst in 1 case.
During surgery, intraoperative minor bleeding occurred in most cases from the resection site and was controlled using cauterisation. One other major intraoperative complication was vitreous loss encountered in 18/56 (32.1%) eyes. Of these 18 eyes, minor vitreous prolapse was suspected at the flap margins in 15/18 eyes and intraoperative vitreous loss occurred in 3/18 eyes. Vitrectomy at the wound margins was performed in these eyes. Postoperative complications included cataract in 21/56 (37.5%) eyes, vitreous haemorrhage (VH) in 15/56 (26.8%), scleral thinning in 10/56 (17.9%), hyphema in 6/56 (10.7%), secondary glaucoma in 3/56 (5.4%), transient elevation of IOP in 3/56 (5.4%), peripheral anterior synechia in 3/56 (5.4%), posterior synechia in 3/56 (5.4%), ptosis in 2/56 (3.6%), bullous keratopathy in 1/56 (1.8%), RD in 1/56 (1.8%), and iridodialysis in 1/56 (1.8%). There were no reported complications related to hypothensive anaesthesia.
Twenty-two out of 56 (39.3%) cases underwent PLSU in the first 10 years and 34/56 (60.7%) cases in the second 10 years over the 20-year study period. In cases undergoing PLSU in the first 10 years, complications included cataract in 12/22 (54.5%) eyes, VH in 7/22 (31.8%), scleral thinning in 6/22 (27.3%), hyphema in 3/22 (13.6%), anterior synechiae in 2/22 (9.1%), posterior synechiae in 2/22 (9.1%), secondary glaucoma in 2/22 (9.1%), iridodialysis in 1/22 (4.5%), bullous keratopathy in 1/22 (4.5%), and ptosis in 1/22 (4.5%). In cases treated with PLSU in the second 10 years of the study period, complications included cataract in 9/34 (26.5%) eyes, VH in 8/34 (23.5%), scleral thinning in 4/34 (11.8%), hyphema in 3/34 (8.8%), transient elevation of IOP in 3/34 (8.8%), secondary glaucoma in 1/34 (2.9%), anterior synechiae in 1/34 (2.9%), posterior synechiae in 1/34 (2.9%), RD in 1/34 (2.9%), and ptosis in 1/34 (2.9%). In the second 10-year period, cataract, VH, scleral thinning, hyphema, anterior/posterior synechiae, and secondary glaucoma development rates were lower than in the first 10-year period. While the decrease in cataract in the second half was statistically significant (p = 0.034), decrements in other complications did not attain statistical significance.
Of 21 eyes that developed cataract during follow-up, phacoemulsification with posterior chamber intraocular lens (IOL) implantation was performed in 15 (71.4%) eyes. During phacoemulsification surgery, nucleus drop occurred in 1 eye which underwent vitrectomy and nucleus removal via vitrectomy and phacofragmentation. One eye developed bullous keratopathy after phacoemulsification surgery. PPV was performed for persistent haemorrhage in 1 of 15 (6.7%) eyes with VH and in 1 eye for RD. VH spontaneously cleared in the remaining 14/15 (93.3%) eyes. Nine eyes with scleral thinning remained stable and 1 eye required scleral patch graft surgery due to anterior staphyloma. Trabeculectomy surgery was performed in 1/3 (33.3%) eye which developed secondary glaucoma from hyphema.
Mean final visual acuity was 0.60 (range: 0–1.9) and 20/80 (range: 20/20–20/1600) on the logMAR and Snellen scales, respectively. Visual acuity improved ≥2 Snellen lines in 17 eyes, remained stable in 28 eyes, and deteriorated in 11 eyes. At a mean follow-up of 40.4 (range: 10–201) months, recurrence was observed in 3 (5.4%) eyes (2 eyes with melanoma and 1 with iris stromal cyst). In two melanoma cases, recurrence developed at 1 month and 13 months. In both cases, recurrent tumour involved the anterior chamber angle. Enucleation was performed in both eyes due to hyphema, secondary glaucoma, and a painful blind eye. The follow-up for these cases were 28 and 36 months. Liver metastasis developed in one of these cases 25 months after enucleation and 27 months after PLSU. In the iris stromal cyst case, recurrence was noted at 6 months but remained stable over the next 13 months of follow-up. Overall, globe salvage rate was 96.4%. There was no other case with known metastasis or death.
Discussion
In our series, we performed PLSU in melanoma and other suspicious uveal tumours where the epicentre of the tumour was in the iris or ciliary body with extension into the adjacent choroid. Shields et al. reported that PLSU can be used in ciliary body and/or peripheral choroid tumours <16 mm in largest tumour diameter if there is no evidence of retinal invasion or vitreous seeding [4]. Damato and Foulds reported that tumours with retinal invasion can also be treated with PLSU, because it was usually possible to preserve an intact retina during surgery, prevent RD by scleral buckle and photocoagulation, and prevent local tumour recurrence by plaque radiotherapy [10].
In the previously published papers on the subject, the most common histopathological diagnosis after PLSU was malignant melanoma (51.4–85.3%) [4, 11,12,13]. PLSU was also performed for adenoma of the nonpigmented ciliary epithelium, leiomyoma, medulloepithelioma, and low-grade adenocarcinoma of the retinal pigment epithelium [14,15,16,17,18,19]. In our series, malignant melanoma accounted for 53.6% (30/56) of cases. Other diagnoses were nevus, iris stromal cyst, melanocytoma, Fuchs’ adenoma, iris pigment epithelial cyst, and invasive breast cancer metastasis. Ramasubramanian et al. also reported that 5/37 (13.5%) paediatric cases treated with PLSU had iris cysts (four iris stromal cysts and one iris pigment epithelial cyst), attesting to the fact that iris cysts cannot sometimes be treated with less invasive methods [12].
The two major intraoperative challenges in PLSU surgery are the failure to create a scleral flap at desired thickness and difficulty in dissecting the uveal tissue without damaging the underlying retina or nonpigmented ciliary epithelium. If the flap is not of the desired thickness initially, as judged by the lack of the underlying blue colour of uvea, the plane of dissection can gently be deepened. To avoid scleral perforation, extreme care should be taken during the dissection and deepening of the scleral flap. The second challenge is the dissection of the uveal tissue without any vertical movement, to avoid perforation of the underlying retina/the nonpigmented ciliary pigment epithelium.
The incidence of postoperative complications after PLSU depends on the size and location of the tumour and surgical experience. The three most common complications are VH, cataract, and RD/proliferative vitreoretinopathy. Shields et al. reported that the most common complication was VH (79/95 eyes, 83.2%) and 5 (6.3%) eyes with VH required subsequent PPV surgery [4]. Lee et al. and Ramasubramanian et al. observed VH in 11/27 (40.7%) eyes and 11/37 (29.7%) eyes, respectively after PLSU [11, 12]. In our study, VH developed in 15/56 (26.8%) eyes and PPV was performed in 1 (6.7%) of these eyes. RD rates after PLSU were between 8.1% to 51.9% in previous reports [4, 11,12,13]. In our series, RD developed in 1/56 (1.8%) eye and this eye underwent PPV. Lee et al. reported that most iatrogenic retinal tear and RDs were present in earlier cases, suggesting a learning curve with surgery [11]. A comparison of complications encountered in the first versus the second 10-year periods of our study showed that the frequency of complications including cataract, VH, scleral thinning, hyphema, anterior/posterior synechiae and secondary glaucoma were less in the second half, reflecting the positive outcomes of the learning curve.
Focal cataract and notching of the lens by the overlying the tumour is an expected feature in anterior uveal tumours. Further, PLSU surgery itself and inadvertent intraoperative lens touch can accelerate cataract formation. Shields et al., Lee et al., and Ramasubramanian et al. reported cataract rates of 33.7%, 14.8% and 32.4%, respectively after PLSU [4, 11, 12]. Phacoemulsification surgery must be performed with care because of the risk of zonular deficiency after PLSU [20]. In our series, 15 of 21 (71.4%) eyes with varying degrees of cataract underwent phacoemulsification with posterior chamber IOL implantation. One eye had PPV and phacofragmentation due to nucleus drop at cataract surgery. Although cataract surgery is usually done after PLSU, Elizalde et al. presented a case which underwent combined cataract surgery and PLSU [14].
Other complications of PLSU include elevated IOP, cystoid macular oedema, retinal/subretinal haemorrhage, preretinal/subretinal fibrosis, choroidal detachment, posterior/anterior synechiae, iris neovascularization, hyphema, scleral thinning, corneal oedema, and blepharoptosis [4, 11, 12]. In our study, scleral thinning was found in 10/56 (17.9%) eyes, hyphema in 6/56 (10.7%), secondary glaucoma in 3/56 (5.4%), transient elevation of IOP in 3/56 (5.4%), peripheral anterior synechia in 3/56 (5.4%), posterior synechia in 3/56 (5.4%), ptosis in 2/56 (3.6%), bullous keratopathy in 1/56 (1.8%), and iridodialysis in 1/56 (1.8%).
As for the debate against performing PLSU, a preoperative detailed examination should be performed to save unnecessary eyes from this invasive surgery. In our series, it was not possible to make the preoperative diagnosis in all cases using clinical and ancillary testing methods, as outlined in the Results section. Although hypotensive anaesthesia may have potential complications, we have seen none in our series. Younger patients such as those with recurrent iris stromal cysts tend to do better with no adverse effects from hypothensive anaesthesia.
Recurrence after PLSU can arise from incomplete tumour removal or from microscopic residual tumour cells. The Collaborative Ocular Melanoma Study found intrascleral melanoma cells in 56% of the eyes that came to enucleation [21]. Kim et al. reported that of nine eyes with noncontiguous intraocular tumour recurrence after transscleral resection, surgical margins were positive in five, negative in two, and uncertain in two [22]. Char et al. found that positive margins were significantly more frequent after PLSU in posterior tumours compared to anterior tumours [13]. Damato et al. reported that multivariate predictors for recurrent melanoma after transscleral resection were epithelioid cell type, posterior tumour extension to <1 disc diameter of optic disc or fovea, large tumour diameter >16 mm, and lack of adjunctive plaque radiotherapy [23]. Recurrence rate was 7.7% in their series [23]. Fabian et al. reported four cases with extraocular relapse after previously resected iris melanoma at a mean of 21 years following initial surgery [24]. This report highlights the need for long-term follow-up for patients that previously underwent melanoma resection. Some authors recommended adjuvant radiotherapy of the tumour area to reduce recurrence [25, 26]. In our study, intraocular tumour recurrence was observed in 2 of 30 (6.7%) melanoma cases and in 1 of 5 (20.0%) iris stromal cyst cases at a mean follow-up of 40.4 months. Extraocular spread was not observed in any of our cases. We employed Ru-106 after PLSU in 5/30 (16.7%) eyes with predominant ciliary body and choroidal involvement.
Shields et al. performed enucleation after PLSU in 15 of 95 (15.8%) eyes, usually because of residual or recurrent tumour [4]. Ramasubramanian et al. reported the indications for enucleation in 9 out of 37 (24.3%) paediatric eyes undergoing PLSU as tumour recurrence in three eyes, prophylaxis for high-grade malignancy in five, and blind painful eye in one [12]. In our series, 2/30 (6.7%) eyes with melanoma recurrence, hyphema, secondary glaucoma, and a painful blind eye underwent enucleation. In total, 93.3% (28/30) of eyes with melanoma and 96.4% (54/56) of all eyes were salvaged.
Eventual metastasis development rate following PLSU is within the expected range for uveal melanoma cases. Damato et al. reported that after transscleral resection 52 of 332 (15.7%) cases expired from metastatic disease and multivariate predictors for metastasis were patient age >60 years at diagnosis, presence of epithelioid tumour cells, largest tumour diameter ≥16 mm, superior (upper) tumour location, and lack of adjunctive plaque radiotherapy [27]. Bechrackis et al. reported that after transscleral resection of large uveal melanomas the 5- and 10-year metastatic rates were 28% and 44%, respectively. Significant risk for metastasis included extraocular spread, tumour thickness, and local tumour recurrence [28]. In our study, liver metastasis developed in 1/30 (3.3%) melanoma case with intraocular recurrence and this patient was alive with treatment at the time of this writing. In a study comparing PLSU and Cobalt-60 plaque radiotherapy for ciliary body or choroidal melanomas, Augsburger et al. reported that the estimated 5-year survival was slightly higher in the resection group (85.2%) compared to the plaque group (81.8%), but the difference was not statistically significant [29].
In conclusion, our study shows that PLSU is useful in the treatment of anteriorly located uveal tumours with acceptable complications considering the learning curve of this difficult surgery. The recurrence rate was 5.4% (3/56) and globe salvage rate was possible in 96.4% (54/56) eyes. The metastasis rate was 3.3% among melanoma cases with a survival rate of 100% across the entire study cohort.
Summary
What was known before
-
Transscleral tumour resection via partial lamellar sclerouvectomy (PLSU) is a relatively well-known technique; however, there has been a paucity of papers on the subject. This is probably due to the fact that PLSU is not preferred by many ocular oncologists because it is a relatively difficult surgery. There has been a shift towards radiotherapy over PLSU for anterior uveal melanomas recently.
What this study adds
-
This study evaluates our experience with PLSU surgery over 20 years for anteriorly located uveal tumours including melanoma, nevus, iris stromal cyst, melanocytoma, and others. Radiotherapy is an alternative to PLSU in the management of anterior uveal melanomas where the diagnosis is certain; however, for tumours with indeterminate features PLSU is needed for both diagnostic and therapeutic purposes. Furthermore, excision of clinically diagnosed non-melanoma tumours by PLSU may be required to prevent complications including cataract, glaucoma, and corneal endothelial decompensation. Our results show that PLSU is useful in the treatment of anteriorly located uveal tumours with acceptable complications, recurrence, globe salvage, metastasis, and survival rates.
References
Gündüz K, Bechrakis NE. Exoresection and endoresection for uveal melanoma. Middle East Afr J Ophthalmol. 2010;17:210–6.
Damato BE. Local resection of uveal melanoma. Dev Ophthalmol. 2012;49:66–80.
Konstantinidis L, Groenewald C, Coupland SE, Damato B. Trans-scleral local resection of toxic choroidal melanoma after proton beam radiotherapy. Br J Ophthalmol. 2014;98:775–9.
Shields JA, Shields CL, Shah P, Sivalingam V. Partial lamellar sclerouvectomy for ciliary body and choroidal tumours. Ophthalmology. 1991;98:971–83.
Damato BE. Local resection of uveal melanoma. Bull Soc Belg Ophtalmol. 1993;248:11–7.
Peyman GA, Juarez CP, Diamond JG, Raichand M. Ten years experience with eye wall resection for uveal malignant melanomas. Ophthalmology. 1984;91:1720–5.
Naumann GO, Rummelt V. Block excision of tumours of the anterior uvea. Report on 68 consecutive patients. Ophthalmology. 1996;103:2017–27. 2027–8 discussion.
Shields JA, Shields CL. Surgical approach to lamellar sclerouvectomy for posterior uveal melanomas: the 1986 Schoenberg lecture. Ophthalmic Surg. 1988;19:774–80.
Kurt RA, Gündüz K. Exoresection via partial lamellar sclerouvectomy approach for uveal tumours: a successful performance by a novice surgeon. Clin Ophthalmol. 2010;4:59–65.
Damato B, Foulds WS. Indications for trans-scleral local resection of uveal melanoma. Br J Ophthalmol. 1996;80:1029–30.
Lee CS, Rim TH, Kwon HJ, Yi JH, Lee SC. Partial lamellar sclerouvectomy of ciliary body tumours in a Korean population. Am J Ophthalmol. 2013;156:36–42.e1.
Ramasubramanian A, Shields CL, Kytasty C, Mahmood Z, Shah SU, Shields JA. Resection of intraocular tumours (partial lamellar sclerouvectomy) in the pediatric age group. Ophthalmology. 2012;119:2507–13.
Char DH, Miller T, Crawford JB. Uveal tumour resection. Br J Ophthalmol. 2001;85:1213–9.
Elizalde J, Ubia S, Barraquer RI. Adenoma of the nonpigmented ciliary epithelium. Eur J Ophthalmol. 2006;16:630–3.
Ishiahara K, Hashida N, Asao K, Usui S, Maruyama K, Nishida K. Rare histological type of adenoma of the nonpigmented ciliary epithelium. Case Rep Ophthalmol. 2019;10:75–80.
Biswas J, Kumar SK, Gopal L, Bhende MP. Leiomyoma of the ciliary body extending to the anterior chamber: clinicopathologic and ultrasound biomicroscopic correlation. Surv Ophthalmol. 2000;44:336–42.
Palamar M, Shields CL, Marr BP, Eagle RC Jr, Shields JA. Retinal pigment epithelial tumour in a young Asian female. Eur J Ophthalmol. 2009;19:487–9.
Yan J, Liu X, Zhang P, Li Y. Acquired adenoma of the nonpigmented ciliary epithelium: analysis of five cases. Graefes Arch Clin Exp Ophthalmol. 2015;253:637–44.
Kaliki S, Shields CL, Eagle RC Jr, Vemuganti GK, Almeida A, Manjandavida FP, et al. Ciliary body medulloepithelioma: analysis of 41 cases. Ophthalmology. 2013;120:2552–9.
Lindquist TD. Capsulorhexis, phacoemulsification, and posterior chamber lens placement following iridocyclectomy. Ophthalmic Surg. 1992;23:44–6.
Histopathologic characteristics of uveal melanomas in eyes enucleated from the Collaborative Ocular Melanoma Study. COMS report no. 6. Am J Ophthalmol. 1998;125:745–66.
Kim JW, Damato BE, Hiscott P. Noncontiguous tumour recurrence of posterior uveal melanoma after transscleral local resection. Arch Ophthalmol. 2002;120:1659–64.
Damato BE, Paul J, Foulds WS. Risk factors for residual and recurrent uveal melanoma after trans-scleral local resection. Br J Ophthalmol. 1996;80:102–8.
Fabian ID, Thaung C, AlHarby L, Sisley K, Mudhar HS, Doherty RE, et al. Late solitary extraocular recurrence from previously resected ıris melanoma. Am J Ophthalmol. 2017;181:97–105.
Damato B. Adjunctive plaque radiotherapy after local resection of uveal melanoma. Front Radiat Ther Oncol. 1997;30:123–32.
Willerding GD, Cordini D, Moser L, Krause L, Foerster MH, Bechrakis NE. Neoadjuvant proton beam irradiation followed by transscleral resection of uveal melanoma in 106 cases. Br J Ophthalmol. 2016;100:463–7.
Damato BE, Paul J, Foulds WS. Risk factors for metastatic uveal melanoma after trans-scleral local resection. Br J Ophthalmol. 1996;80:109–16.
Bechrakis NE, Petousis V, Willerding G, Krause L, Wachtlin J, Stroux A, et al. Ten-year results of transscleral resection of large uveal melanomas: local tumour control and metastatic rate. Br J Ophthalmol. 2010;94:460–6.
Augsburger JJ, Lauritzen K, Gamel JW, DeBrakeleer DJ, Lowry JC, Eisenman R. Matched group study of surgical resection versus cobalt-60 plaque radiotherapy for primary choroidal or ciliary body melanoma. Ophthalmic Surg. 1990;21:682–8.
Acknowledgements
The authors acknowledge Hatice Kaykusuz, MD from the Anaesthesiology Department, Ankara University Faculty of Medicine and Funda Seher Özalp Ateş, Msc from the Biostatistics Department, Ankara University Faculty of Medicine for their contributions in the preparation of the paper. There are no sources of support including sponsorship (e.g. university, charity, commercial organisation) and sources of material (e.g. novel drugs) not available commercially.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirzayev, I., Gündüz, A.K. & Okçu Heper, A. Partial lamellar sclerouvectomy surgery for anteriorly located uveal tumour resection: a 20-year experience. Eye 36, 969–977 (2022). https://doi.org/10.1038/s41433-021-01545-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01545-7
This article is cited by
-
Local resection via partial lamellar sclerouvectomy for ciliary body tumors — a case series
BMC Ophthalmology (2024)