Abstract
Glaucoma drainage device (GDD)-related endophthalmitis is a devastating complication of device implantation. There are no guidelines in the literature to assist clinicians in deciding if the GDD should be explanted or if patients require pars plana vitrectomy (PPV). This study compares the outcomes of GDD explantation with device retention and also independently compares the outcomes of PPV versus intravitreal antibiotics alone in patients with GDD-related endophthalmitis. A literature search for studies discussing GDD-related endophthalmitis from 2005 to 2019 was performed; 30 articles were included. The visual acuity/anatomical outcomes were compared between GDD explantation and retention, and between patients that received a PPV and those that did not. These outcomes were combined with a medical records review of 13 patients with GDD-related endophthalmitis from an academic institution. A total of 88 eyes were included. 70.5% underwent GDD explantation, while 37.8% received a PPV. GDD explantation was associated with a lower rate of evisceration/enucleation when compared to GDD retention (4.8% versus 19.2%, OR 0.22, 95% CI 0.05–1.01, p = 0.05), but visual acuity outcomes were similar. No eyes that received an immediate vitrectomy became phthisic or required evisceration/enucleation, compared an evisceration/enucleation rate of 15.2% in eyes treated solely with intravitreal antibiotics (OR 1.18, 95% CI 1.04–1.33, p = 0.04). Explantation of the GDD and immediate vitrectomy are both associated with better anatomical outcomes in GDD-related endophthalmitis. Further research is needed to provide more definitive guidelines in the ideal management of these patients.
摘要
青光眼引流阀相关性眼内炎是植入物植入术后的严重并发症。目前文献中没有指南帮助临床医生决定是否应该取出GDD, 或者患者是否需要进行玻璃体切除术 (PPV) 。本文比较了在GDD相关眼内炎患者中采用PPV和单独使用玻璃体腔抗生素的临床结局。
我们对2005–2019年GDD相关眼内炎的文献进行了检索, 共纳入30篇文章。比较了GDD取出和保留以及接受PPV和未接受PPV患者的视力及解剖结果。这些结果与其它一学术机构对13例GDD相关眼内炎患者的病历资料进行了整合。
本文共纳入88只眼。70.5%的患者行GDD取出术, 37.8%患者行PPV术。与保留GDD相比, GDD取出术的患者眼球摘除率更低(4.8% vs 19.2%, OR 0.22, 95% CI 0.05–1.01, p = 0.05), 但两者的视力结果相似。立即行玻璃体切除术的眼没有一例出现炎症或需要眼球摘除, 而仅接受玻璃体内抗生素治疗的眼睛摘除率为15.2% (OR 1.18, 95% CI 1.04 – 1.33, p = 0.04)。
在GDD相关的眼内炎中, 摘除GDD术和直接行玻璃体切除术都有更好的解剖结果。未来需要进一步的研究来为患者理想的治疗提供更明确的指导方针。
Similar content being viewed by others
Introduction
Glaucoma drainage devices (GDDs) are widely used for the management of intractable glaucoma. Delayed endophthalmitis presenting months to years after surgery is a relatively uncommon complication of GDD surgery, but this complication can be visually devastating [1]. Endophthalmitis rates after GDD surgery are reported at 1–2%, although this risk is higher in pediatric patients [2, 3].
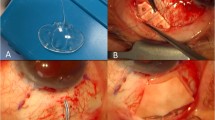
The risk of endophthalmitis after GDD implantation persists for years; there have been multiple descriptions of late-onset endophthalmitis from GDDs. GDD-related endophthalmitis has been described with all main types of devices, including the commonly used Baerveldt, Molteno, and Ahmed designs [1, 2]. An important risk factor for GDD-related endophthalmitis is exposure of the tube or plate, which occurs in ~6% of cases [3]. Thus, it is standard practice to cover the exposed GDD immediately after the exposure is identified to minimize the risk of endophthalmitis [1].
In contrast, there has been no consensus on whether the GDD needs to be explanted once endophthalmitis has already developed. Variable results have been reported with both explantation of the device as part of infection management and with retaining the device. The GDD can act as a reservoir of bacteria, thus precluding effective treatment of the infection with device retention. Conversely, explantation of the device can result in uncontrolled intraocular pressures and permanent vision loss from glaucoma [4]. In addition, several case reports from the 1990s demonstrate adequate infection control without explantation of the GDD [5, 6], leading some surgeons to try to retain the GDD [7].
Furthermore, there is no consensus on whether patients with GDD-related endophthalmitis should be treated with pars plana vitrectomy or solely with intravitreal antibiotics. The Endophthalmitis Vitrectomy Study, which studied the treatment of endophthalmitis after cataract surgery, demonstrated that patients with hand-motion visual acuity (VA) or better could be successfully treated without vitrectomy [8]. However, in trabeculectomy bleb-associated endophthalmitis, there are better VA outcomes in patients who undergo vitrectomy without stratification by VA [9]. Unfortunately, no such evidence-based guidelines exist for endophthalmitis related to GDD implantation.
The purpose of this review is to examine the literature relating to GDD explantation in endophthalmitis and to report the outcomes a case series of GDD-related endophthalmitis at an academic institution. In addition, we aim to compare the outcomes of patients treated with pars plana vitrectomy versus those treated with intravitreal antibiotics without vitreoretinal surgery.
Methods
Retrospective chart review
A retrospective chart review was performed, identifying all patients treated for GDD-related endophthalmitis at a large academic institution between 2014 and 2019. Patients were included if they had a GDD in place at the time of their endophthalmitis diagnosis. Patients were excluded if endophthalmitis clearly developed secondary to eye pathology unrelated to their GDD, such as a corneal ulcer. Patient charts were reviewed for VA data, causative organism, treatment modalities, and length of follow-up. The Institutional Review Board at the University of Florida, Florida, United States of America deemed that approval was not needed for this study. This study adhered to the guidelines of the Declaration of Helsinki.
Review of the literature
The following search terms were entered into www.pubmed.gov (United States National Library of Medicine, National Institutes of Health): “(Glaucoma Implant AND Endophthalmitis) OR (Glaucoma Drainage Device AND Endophthalmitis).” The last search was conducted on January 2, 2020. Results were limited to research studies conducted in humans between 2005 and 2019 that were written in English. This search yielded 186 articles. All articles underwent brief review. If the articles were deemed potentially relevant to this review, more extensive analysis of the article was performed. Thirty articles were subsequently met the inclusion/exclusion criteria below and were thus included.
Case reports, case series, and original studies were included; review articles were excluded if they did not include any primary data. Articles must have discussed whether the GDD remained in the eye, or if it was explanted, to be considered for inclusion. Literature that solely pertained to minimally invasive glaucoma surgery, and did not include glaucoma tube shunts, were also excluded. Studies discussing GDDs in both adults and children were included. Eyes that underwent primary evisceration or enucleation were excluded from analysis.
VA outcomes, incidence of phthisis, incidence of evisceration or enucleation, and the treatment each patient received were documented from each study, when available. VA was denoted at baseline (prior to endophthalmitis diagnosis), at the time of endophthalmitis diagnosis, and final VA (defined as VA at last follow-up, or the last VA reported in the study). Changes in VA were calculated by converting VA measurements to logMAR scale, then by comparing final VA to both baseline acuity and acuity at the time of endophthalmitis diagnosis. Only primary data (i.e., VA and anatomic outcomes) were extracted from the available literature to minimize risk of bias.
Statistical analysis
Because the distribution of the changes of VA is not normally distributed, a nonparametric Kruskal–Wallis test was used to compare the distribution between VA outcomes of those that retained the GDD and those that had it explanted. For the rates of evisceration/enucleation and phthisis, odds ratios with 95% confidence intervals were calculated from Proc Freq. Due to small sample sizes in some groups, the Fisher’s Exact test was used to test the association between the group and the rates of evisceration/enucleation and phthisis. All analyses were conducted using SAS 9.4 (NC, Cary).
Results
A total of thirteen patients treated at our center met the inclusion and exclusion criteria for retrospective chart review. Their baseline characteristics, VA, and treatments required are described in Table 1. As part of our institution’s practice pattern, all patients underwent explantation of the GDD as part of their endophthalmitis treatment. The exception to this is patient twelve, who was initially treated at another facility and referred to our center for evisceration after he had persistent endophthalmitis and scleral necrosis unresponsive to multiple surgeries at his prior facility. The average VA at baseline was logMAR 1.25 (8 eyes) in our cohort, logMAR 2.67 at endophthalmitis diagnosis (13 eyes), and logMAR 1.86 at last follow-up (12 eyes). Length of follow-up varied between 1 month to 5 years, with an average follow-up of 2 years, excluding two patients still undergoing active follow-up due to recent diagnosis of endophthalmitis. Four eyes (30.7%) had exposed GDDs at the time of diagnosis. In addition to explantation of the GDD in all patients except patient twelve, seven eyes underwent pars plana vitrectomy with injection of intravitreal antibiotics, while the remaining six eyes received intravitreal antibiotics without vitrectomy. Three eyes ultimately underwent evisceration—two for being blind, painful eyes, and a third for persistent infection with scleral necrosis. All three eyes that underwent evisceration had been treated with intravitreal antibiotics but without a vitrectomy. The underlying organism was identified in five patients; two eyes grew Pseudomonas aeruginosa, while one eye each was infected with coagulase-negative Staphylococcus, Aspergillus niger, and Neisseria meningitidis.
A summary of literature included in this study is included in Table 2; a total of thirty articles met inclusion and exclusion criteria. VA prior to the development of endophthalmitis, at the time of endophthalmitis, and at the final follow-up were included, when available. A total of 78 eyes were included in the 30 studies, many of which were case reports. Three of these eyes were excluded, as they underwent primary enucleation or evisceration. Fifty eyes (66.7%) underwent explantation of the GDD, while 25 eyes (33.3%) retained the GDD. Multiple studies commented that the GDD appeared grossly infected at the time of explantation, and the device plate and/or tube grew the same organism isolated from the vitreous sample [10,11,12].
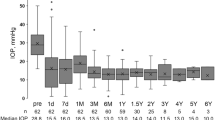
For the following analysis, our cohort was combined with the cases described in the literature. These patients were separated into two groups; Group 1 had the GDD explanted as part of endophthalmitis treatment (62 eyes/70.5%), while Group 2 did not undergo GDD explantation (26 eyes/29.5%). The average VA at baseline, prior to the development of endophthalmitis, was logMAR 1.35 in Group 1 (40 eyes), as compared to 0.92 in Group 2 (17 eyes). At the time of diagnosis of endophthalmitis, the average VA was logMAR 2.42 in Group 1 (28 eyes) and 2.51 in Group 2 (9 eyes). The timing of final VA varied both between and within studies, but this generally defined the VA at the last follow-up visit. The final VA was 2.14 in Group 1 (46 eyes) and 1.76 in Group 2 (19 eyes). The change in average logMAR VA was similar in both groups when comparing final VA to baseline VA (0.88 in Group 1/39 eyes, 0.85 in Group 2/17 eyes; p = 0.97). LogMAR VA in Group 1 improved by an average of −0.46 logMAR between the VA at time of endophthalmitis diagnosis and final VA (27 eyes), whereas Group 2 improved by an average of −0.98 logMAR (9 eyes) (p = 0.29).
We then compared the survival of eyes who developed GDD-related endophthalmitis. One eye in Group 1 became phthisical (1.6%), while one eye in Group 2 also became phthisical (3.8%) (OR 0.42, 95% CI 0.03–7.05, p = 0.52). Three eyes in Group 1 were enucleated or eviscerated (4.8%), compared to five eyes (19.2%) in Group 2 (OR 0.22, 95% CI 0.05–1.01, p = 0.05). Of note, one of the eyes that was eviscerated in Group 1 had the GDD explanted 1 week after the endophthalmitis diagnosis, not as part of the initial treatment.
The outcomes of treating endophthalmitis with solely intravitreal antibiotics versus vitrectomy were then compared independently. A total of 74 eyes underwent either a vitreous tap with injection of intravitreal antibiotics and/or antifungal agents without vitrectomy (“tap and inject”; Group 3) or received a vitrectomy, typically with concomitant intravitreal antibiotics and/or antifungal agents, at some point during their treatment (Group 4). Group 3 included 46 eyes (62.2%) and Group 4 included 28 eyes (37.8%). The remaining patients were managed with less common treatments, such as only systemic antibiotics, and thus were excluded from this subanalysis. There were two patients in Group 4 who were initially treated with a tap and inject, but then later received a vitrectomy for persistent endophthalmitis; these eyes were then excluded from the following analysis so that only eyes that received a tap and inject or immediate vitrectomy were compared to avoid confounding by delayed vitrectomy. One of the eyes that received a delayed vitrectomy (5 weeks after initial endophthalmitis diagnosis) became phthisical and ultimately received an evisceration. Seven eyes (15.2%) in Group 3 were ultimately enucleated or eviscerated; no eyes that received an immediate vitrectomy in Group 4 were eviscerated (OR 1.18, 95% CI 1.04–1.33, p = 0.04). One eye in Group 3 (2.2%), but no eyes that received an immediate vitrectomy in Group 4, became phthisical (OR 1.02, 95% CI 0.98–1.07, p > 0.99).
Discussion
Overall, the level of evidence related to guide clinicians on how to manage GDD-related endophthalmitis is weak. It is difficult to perform randomized control trials or prospective studies in this field due to the rare nature of this complication. While some studies discuss both removal and retention of these devices, there is generally no rationale provided as to which devices require removal. No study commented on the factors that influenced the authors’ decision to explant the GDD. Zheng et al. commented that only GDDs that were exposed were removed but did not specify if GDD exposure was the criteria for explantation [13]. Other authors successfully revised the eroded GDD without explantation [14]. Thus, management of the GDD during treatment of endophthalmitis lacks specific guidelines in the available literature.
In studies published since 2005 and including our institution’s case series, the GDD has been explanted in 70.5% (62 out of 88) of cases. Multiple studies have cultured the tube and/or plate and found that these were contaminated with the same organism isolated from vitreous aspirates. This supports the argument that the GDD can be a nidus for infection and should be removed as part of endophthalmitis treatment [7, 10,11,12, 15]. In a case report by Park et al., the GDD was initially retained, and the patient’s endophthalmitis was well-controlled with intravitreal and systemic antibiotics; however, within 10 days, the peritomy site again became infected [7]. The GDD was subsequently removed with resultant infection control. As a result, the authors argued for early explantation of the GDD. In this review, fewer eyes that had the GDD explanted became phthisical or required removal, indicating that GDD explantation is associated with better anatomical outcomes; the difference in evisceration/enucleation rates was statistically significant. Given the improved anatomical outcomes and multiple reports of the GDD being grossly infected with the endophthalmitis-causing organism, we argue that it is beneficial to remove the GDD.
However, there was no statistically significant difference in the change in VA from the time of endophthalmitis diagnosis to final VA between the patients that had the GDD explanted and those that did not, or in the change in VA from baseline to final VA. Thus, explanting the GDD is not associated with a difference in visual outcomes. Interpreting this data is challenging, as patients were not randomized to treatment, and VA data are missing from many of the studies published on this subject. In addition, while control of intraocular pressure after GDD explantation was typically not discussed, a few studies suggest that long-term intraocular pressure was still well-controlled without further surgery, possibly due to ciliary body damage from endophthalmitis [10, 16, 17].
Unlike other causes of post-operative endophthalmitis, such as cataract surgery, there is no study that delineates whether patients with GDD-related endophthalmitis require a pars plana vitrectomy as primary treatment of the infection. None of the literature clearly describes what influenced the surgeon’s decision to pursue a vitrectomy versus vitreous tap with intravitreal antibiotics as initial treatment of endophthalmitis; treatment appears to be mostly related to institutional preference and/or the perceived severity of the infection. Stewart et al. described a patient who was initially treated without a vitrectomy and had a recurrence of endophthalmitis within 1 week. As a result, the patient ultimately required a vitrectomy, leading the authors to argue for early vitrectomy and aggressive surgical management in these patients [15]. A few patients were treated with systemic antibiotics without direct intraocular antibiotics; however, these were rare cases and should not be considered standard of care [12, 18, 19]. In this review, no patients that received an immediate vitrectomy required an evisceration or enucleation, compared to 15.2% of patients who were treated with solely a tap and inject (p = 0.04). Rates of phthisis were similar between the two groups. Early PPV at the time of endophthalmitis diagnosis is associated with better anatomical outcomes, although more data are needed to be confident in this conclusion.
This review is limited by the relatively small number of patients, both in our cohort and patients reported in the literature since 2005. These small numbers reflect the relatively infrequent occurrence of endophthalmitis after GDD implantation. Further limiting our analysis is the fact that studies included in this review did not always report the VA, treatment modalities, or outcomes in these patients, further limiting sample sizes for each of the subanalyses. In addition, most studies did not provide a rationale for why treatment modalities (such as PPV or GDD explantation) were pursued, and no patients were randomized to either treatment. Thus, there is a risk of confounding. However, despite these constraints, this study aims to summarize the available evidence in this field over the past 15 years, as no such review currently exists for this potentially visually devastating outcome.
In conclusion, GDD-related endophthalmitis can be devastating and requires prompt management. Explanting the GDD removes the nidus for infection and is associated with lower rates of evisceration/enucleation, but similar rates of phthisis. VA outcomes are ambivalent regarding GDD removal, but this data is confounded by a lack of randomization to explantation versus retention of the GDD, making interpretation difficult. Similarly, early PPV in GDD-related endophthalmitis is associated with significantly lower rates of evisceration/enucleation but similar rates of phthisis, and thus early vitrectomy may be beneficial to prevent ultimate loss of the eye. Further studies directly comparing outcomes in GDD explantation to retention, and outcomes of PPV versus solely intravitreal antibiotics, would be helpful in providing more definitive, evidence-based, guidelines. However, until such data exists, we favor early vitrectomy with intravitreal antibiotics and explantation of the GDD based on outcomes from our case series and the current literature.
References
Gedde SJ, Scott IU, Tabandeh H, Luu KK, Budenz DL, Greenfield DS, et al. Late endophthalmitis associated with glaucoma drainage implants. Ophthalmology. 2001;108:1323–7. https://doi.org/10.1016/s0161-6420(01)00598-x.
Al-Torbak AA, Al-Shahwan S, Al-Jadaan I, Al-Hommadi A, Edward DP. Endophthalmitis associated with the Ahmed glaucoma valve implant. Br J Ophthalmol. 2005;89:454–8. https://doi.org/10.1136/bjo.2004.049015.
Levinson JD, Giangiacomo AL, Beck AD, Pruett PB, Superak HM, Lynn MJ, et al. Glaucoma drainage devices: risk of exposure and infection. Am J Ophthalmol. 2015;160:516–21.e2. https://doi.org/10.1016/j.ajo.2015.05.025.
Wentzloff JN, Grosskreutz CL, Pasquale LR, Walton DS, Chen TC. Endophthalmitis after glaucoma drainage implant surgery. Int Ophthalmol Clin. 2007;47:109–15. https://doi.org/10.1097/IIO.0b013e318037766a.
Nguyen QH, Budenz DL, Parrish RK. Complications of Baerveldt glaucoma drainage implants. Arch Ophthalmol. 1998;116:571–5. https://doi.org/10.1001/archopht.116.5.571.
Krebs DB, Liebmann JM, Ritch R, Speaker M. Late infectious endophthalmitis from exposed glaucoma setons. Arch Ophthalmol. 1992;110:174–5. https://doi.org/10.1001/archopht.1992.01080140024014.
Park SS, Rabowsky J. Early postoperative endophthalmitis after pars plana Ahmed valve placement with persistent extraocular infection. Ophthalmic Surg Lasers Imaging. 2007;38:404–5. https://doi.org/10.3928/15428877-20070901-09.
Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Endophthalmitis Vitrectomy Study Group. Arch Ophthalmol. 1995;113:1479–96.
Song A, Scott IU, Flynn HW, Budenz DL. Delayed-onset bleb-associated endophthalmitis: clinical features and visual acuity outcomes. Ophthalmology. 2002;109:985–91. https://doi.org/10.1016/s0161-6420(02)00965-x.
Rao A, Wallang B, Padhy TR, Mittal R, Sharma S. Dual infection by streptococcus and atypical mycobacteria following Ahmed glaucoma valve surgery. Semin Ophthalmol. 2013;28:233–5. https://doi.org/10.3109/08820538.2012.760621.
Tsui I, Uslan DZ, Hubschman J-P, Deng SX. Nocardia farcinica infection of a Baerveldt implant and endophthalmitis in a patient with a Boston type I keratoprosthesis. J Glaucoma. 2010;19:339–40. https://doi.org/10.1097/IJG.0b013e3181bd8987.
Chendran P, Seng Fai T, Wan Abdul Halim WH, Md. Din N. Pyogenic granuloma formation following Ahmed valve glaucoma implant. J Glaucoma. 2019;28:e162–4. https://doi.org/10.1097/IJG.0000000000001334.
Zheng CX, Moster MR, Khan MA, Chiang A, Garg SJ, Dai Y, et al. Infectious endophthalmitis after glaucoma drainage implant suurgery: clinical features, microbial spectrum, and outcomes. Retina. 2017;37:1160–7. https://doi.org/10.1097/IAE.0000000000001329.
Ranganath A, Hashim A. Late-onset endophthalmitis secondary to exposed glaucoma tube implant in a rare case of paediatric glaucoma. Case Rep Ophthalmol Med. 2011;2011:183647. https://doi.org/10.1155/2011/183647.
Stewart MW, Bolling JP, Bendel RE. Nocardia brasiliensis endophthalmitis in a patient with an exposed Ahmed glaucoma drainage implant. Ocul Immunol Inflamm. 2013;21:69–70. https://doi.org/10.3109/09273948.2012.736586.
Medina CA, Butler MR, Deobhakta AA, Bannit MR, Albini TA, Smiddy WE, et al. Endophthalmitis associated with glaucoma drainage implants. Ophthalmic Surg Lasers Imaging Retina. 2016;47:563–9. https://doi.org/10.3928/23258160-20160601-08.
Bayraktar Z, Kapran Z, Bayraktar S, Acar N, Unver YB, Gök K. Delayed-onset streptococcus pyogenes endophthalmitis following Ahmed glaucoma valve implantation. Jpn J Ophthalmol. 2005;49:315–7. https://doi.org/10.1007/s10384-005-0202-3.
Kassam F, Lee BE, Damji KF. Concurrent endophthalmitis and orbital cellulitis in a child with congenital glaucoma and a glaucoma drainage device. Digit J Ophthalmol. 2011;17:58–61. https://doi.org/10.5693/djo.02.2011.10.002.
Shah M, Relhan N, Kuriyan AE, Davis JL, Albini TA, Pathengay A, et al. Endophthalmitis caused by nontuberculous mycobacterium: clinical features, antimicrobial susceptibilities, and treatment outcomes. Am J Ophthalmol. 2016;168:150–6. https://doi.org/10.1016/j.ajo.2016.03.035.
Mandalos A, Sung V. Glaucoma drainage device surgery in children and adults: a comparative study of outcomes and complications. Graefes Arch Clin Exp Ophthalmol. 2017;255:1003–11. https://doi.org/10.1007/s00417-017-3584-2.
Mandalos A, Tailor R, Parmar T, Sung V. The long-term outcomes of glaucoma drainage devices in pediatric glaucoma. J Glaucoma. 2016;25:e189–195. https://doi.org/10.1097/IJG.0000000000000164.
Sridhar J, Kuriyan AE, Flynn HW, Smiddy WE, Venincasa VD, Miller D. Endophthalmitis caused by Serratia marcescens: clinical features, antibiotic susceptibilities, and treatment outcomes. Retina. 2015;35:1095–100. https://doi.org/10.1097/IAE.0000000000000509.
Li JY, Greiner MA, Brandt JD, Lim MC, Mannis MJ. Long-term complications associated with glaucoma drainage devices and Boston keratoprosthesis. Am J Ophthalmol. 2011;152:209–18. https://doi.org/10.1016/j.ajo.2011.01.034.
Elhefny E, Mokbel T, Abou Samra W, Kishk H, Mohsen T, El-Kannishy A. Long-term results of Ahmed glaucoma valve implantation in Egyptian population. Int J Ophthalmol. 2018. https://doi.org/10.18240/ijo.2018.03.11.
Pan Q, Jampel HD, Ramulu P, Schwartz GF, Cotter F, Cute D, et al. Clinical outcomes of gamma-irradiated sterile cornea in aqueous drainage device surgery: a multicenter retrospective study. Eye. 2017;31:430–6. https://doi.org/10.1038/eye.2016.230.
Huh ES, Aref AA, Vajaranant TS, de la Cruz J, Chau FY, Cortina MS. Outcomes of pars plana glaucoma drainage implant in Boston type 1 keratoprosthesis surgery. J Glaucoma. 2014;23:e39–44. https://doi.org/10.1097/IJG.0b013e31829e55f8.
AlHadlaq A, AlMalki S, AlShahwan S. Late onset endophthalmitis associated with unexposed glaucoma valved drainage device. Saudi J Ophthalmol. 2016;30:125–7. https://doi.org/10.1016/j.sjopt.2015.12.005.
Sridhar J, Kuriyan AE, Flynn HW, Miller D. Endophthalmitis caused by Pseudomonas aeruginosa: Clinical features, antibiotic susceptibilities, and treatment outcomes. Retina. 2015;35:1101–6. https://doi.org/10.1097/IAE.0000000000000469.
Salim N-L, Azhany Y, Abdul Rahman Z, Yusof R, Liza-Sharmini AT. Infedcted Baerveldt glaucomad rainage device by Aspergillus niger. Case Rep Ophthalmological Med. 2015;2015:1–3. https://doi.org/10.1155/2015/249419.
Eslami Y, Mohammadi M, Fakhraie G, Zarei R, Moghimi S. Ahmed glaucoma valve implantation with tube insertion through the ciliary sulcus in pseudophakic/aphakic eyes. J Glaucoma. 2014;23:115–8. https://doi.org/10.1097/IJG.0b013e318265bc0b.
Kwon HJ, Kerr NM, Ruddle JB, Ang GS. Endophthalmitis associated with glaucoma shunt intraluminal stent exposure. J Curr Glaucoma Pract. 2016;10:36–7. https://doi.org/10.5005/jp-journals-10008-1199.
Huang J, Lin J, Wu Z, Xu H, Zuo C, Ge J. Outcomes of Ahmed glaucoma valve implantation in advanced primary congenital glaucoma with previous surgical failure. OPTH. 2015:977. https://doi.org/10.2147/OPTH.S83820.
Robert M-C, Hamel P, Blondeau P, Lesk MR. Persistent leak after glaucoma aqueous shunt implantation. J Glaucoma. 2013;22:647–51. https://doi.org/10.1097/IJG.0b013e318255dbe7.
Turalba AV, Pasquale LR. Hypertensive phase and early complications after Ahmed glaucoma valve implantation with intraoperative subtenon triamcinolone acetonide. Clin Ophthalmol. 2014;8:1311–6. https://doi.org/10.2147/OPTH.S64257.
Roy AK, Senthil S. Conjunctival inclusion cyst following repair of tube erosion in a child with aphakic glaucoma, leading to endophthalmitis. GMS Ophthalmol Cases. 2015;5:Doc03. https://doi.org/10.3205/oc000025.
Trzcinka A, Soans FP, Archer SM, Moroi SE. Late-onset haemophilus influenzae endophthalmitis in an immunized child after Baerveldt implant. J Aapos. 2008;12:412–4. https://doi.org/10.1016/j.jaapos.2008.02.008.
Acknowledgements
The authors would like to thank Wei Xue, Ph.D., for her assistance with the statistical analysis.
Funding
The statistical analysis for this work was partially supported by the NIH National Center for Advancing Translational Sciences under award number UL1TR001427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Islam, Y.F.K., Blake, C.R. & Gibran, S.K. Management of endophthalmitis related to glaucoma drainage devices: review of the literature and our experience. Eye 35, 1850–1858 (2021). https://doi.org/10.1038/s41433-021-01462-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01462-9
This article is cited by
-
A novel, minimally invasive implant to assist in repeated intraocular drug delivery
Biomedical Microdevices (2022)