Abstract
Purpose
To quantify stereopsis and other visual functions in patients with unilateral branch retinal vein occlusion (BRVO) and to investigate vision-related parameters that affect stereopsis.
Design
Prospective observational study.
Subjects
Forty-five patients undergoing intravitreal ranibizumab (IVR) treatment for unilateral BRVO.
Methods
We examined stereopsis using the Titmus stereo test (TST) and TNO stereotest (TNO), best corrected visual acuity (BCVA), letter contrast sensitivity, severity of metamorphopsia and degree of aniseikonia before and 6 months after IVR.
Main outcome measures
Visual functions that affect stereopsis.
Results
Baseline stereopsis in patients with BRVO was 2.7 ± 0.6 (range, 1.6–3.5) in the TST and 2.8 ± 0.5 (range, 1.8–3.3) in TNO. TST and TNO scores were significantly correlated with BCVA and letter contrast sensitivity at baseline (P < 0.001) but not with other visual functions. IVR treatment significantly improved stereopsis, BCVA, and letter contrast sensitivity. After treatment, TST scores were significantly correlated with BCVA (P < 0.001), letter contrast sensitivity (P < 0.001), and aniseikonia (P < 0.01). TNO scores were significantly correlated with BCVA (P < 0.01) and letter contrast sensitivity (P < 0.01). TST and TNO scores after treatment were significantly correlated with BCVA at baseline (P < 0.01 for both).
Conclusions
Deterioration of stereopsis in patients with BRVO was associated with changes in visual acuity and contrast sensitivity after treatment. Initial visual acuity is a prognostic factor for posttreatment stereopsis.
Similar content being viewed by others
Introduction
Branch retinal vein occlusion (BRVO) is a common retinal disease, in which not only visual acuity but various visual functions, such as stereopsis, contrast sensitivity, metamorphopsia, and aniseikonia, are also impaired [1,2,3,4,5,6]. A study investigated binocular visual function following intravitreal ranibizumab (IVR) injection for BRVO and found that unilateral BRVO caused the deterioration of stereopsis [2].
Stereopsis is the ability to perceive depth of field based on the parallax between the images of both eyes. It is an important function in binocular vision. Visual acuity is a parameter that affects stereopsis. Stereopsis is frequently lost in patients with visual impairment in one eye [7,8,9,10,11]. A number of other factors affect stereopsis, including aniseikonia [12,13,14], eye dominance [12, 15], pupil size [14, 16], accommodation [11, 17] and amblyopia [11].
Several studies have found the deterioration of stereopsis in retinal disorders, including BRVO, epiretinal membrane (ERM) [18, 19], macular hole (MH) [20, 21], and after rhegmatogenous retinal detachment (RD) surgery [22]. We found a significant deterioration in stereopsis in patients with BRVO compared with normal subjects. IVR injections improved stereopsis in patients with BRVO; however, the improvement was not to a normal level. Stereopsis is a part of binocular function; therefore, unilateral metamorphopsia, contrast sensitivity and aniseikonia may affect stereopsis. However, to our knowledge, no studies have elucidated the details of vision-related parameters that cause stereopsis deficits in BRVO patients.
The purpose of this study was to quantify stereopsis and other visual function parameters, including visual acuity, contrast sensitivity, metamorphopsia and aniseikonia, in patients with unilateral BRVO and identify vision-related parameters that affect stereopsis.
Methods
This prospective study was approved by the Institutional Review Board of the University of Tsukuba Hospital and adhered to the tenets of the Declaration of Helsinki. Signed informed consent was obtained from all study subjects after the nature of the study was explained. Patients who were diagnosed with BRVO at the University of Tsukuba Hospital between April 2015 and May 2018 were included in the study. All patients were treatment-naïve without any history of treatment with intravitreal antivascular endothelial growth factor, intraocular corticosteroids, vitrectomy or retinal photocoagulation. The exclusion criteria were strabismus, moderate or severe cataract, any systemic disease that could affect ocular motility, anisometropia >2 dioptres and amblyopia.
This study was conducted after determining a reasonable sample size. In previous studies, the mean change was 0.66 (range, 2.72–2.06, standard deviation 0.50) in stereopsis [2] and 6.0 (range, 14.3–20.4, standard deviation 5.0) in contrast [4]. Power analysis, a sample size calculation technique, was performed along with paired t-test at a power of 0.8 and a significance level of 0.05, respectively. We analysed the sample size for significant differences in stereopsis and contrast and found 20 and 25 cases, respectively. Therefore, we decided to include >25 patients for this study.
Eligible patients were examined every month and treated with IVR injection pro ne nata for 6 months. IVR injections were administered starting from the time of diagnosis with additional ranibizumab injections if central retinal thickness was >300 μm or serous RD or subretinal haemorrhage was present. All patients were examined for best corrected visual acuity (BCVA), stereopsis, letter contrast sensitivity, severity of metamorphopsia and degree of aniseikonia at baseline and after 1, 2, 3, 4, 5, and 6 months.
BCVA was measured using the Landolt chart and expressed as the logarithm of the minimum angle of resolution (logMAR).
Stereopsis was measured using the Titmus stereo test (TST) and TNO stereotest (TNO) at a viewing distance of 40 cm with appropriate spectacle correction. To ensure that the patients were not using monocular clues in the TST, their responses were checked by inverting the stereo target and asking if the target appeared in front of or behind the page. The TST and TNO results were expressed as seconds of arc and we converted these values to logarithms for statistical assessment. We examined letter contrast sensitivity using the CSV-1000LV chart (Vector Vision, Greenville, OH, USA). This chart consists of 24 letters; 3 letters with the same contrast are shown, and the subject is asked to enter the letters that can be seen. The contrast is reduced in each subsequent triplet. If no letters are detected, the subject receives a score of 0, and the highest score is 24. The test was performed monocularly with an undilated eye and optimal eyeglass correction at a distance of 2.5 m. The severity of metamorphopsia was recorded using M-CHARTS (Inami Co., Tokyo, Japan). This chart has 19 double lines with dots, spaced at a visual angle of 0.2–2.0 degrees. If a continuous line is used instead of a dotted line, and the dot spacing is changed from fine to coarse lines, increasing the dot spacing will reduce the distortion of the line until the line appears to be continuous [23, 24]. If the patient recognised a straight line (0 degrees) as irregular or curved, we continued the test with M-CHARTS, where the intervals of the dotted line gradually changed from fine to coarse on subsequent pages. When the patient recognised a dotted line as straight, the visual angle separating the dots was determined to represent the patient’s metamorphopsia score. The test was performed monocularly with an undilated eye and optimal eyeglass correction at a distance of 30 cm. Vertical and horizontal meridians were assessed, and their mean values were analysed. We examined the degree of aniseikonia with the New Aniseikonia Test (NAT; Handaya, Tokyo, Japan). NAT measures aniseikonia by simply using a special book and red/green glasses. The book has the pictures of red and green semicircles presented side-by-side, wherein the distance and size increases by 1% each time from 1 to 24%. Patients with red/green glasses viewed the page from a distance of 40 cm and were instructed to select the pair in which both semicircles appeared to be the same size. The ratio of the semicircle sizes in the selected pair indicated the percentage of aniseikonia. We defined macropsia when the percentage of aniseikonia was >2% and micropsia when the percentage was <−2%. All ophthalmic examinations were performed by skilled orthoptists.
The mean and standard deviation were calculated to compare all vision-related parameters. The Wilcoxon signed rank test was used to examine differences in visual functions before and after treatment. Associations between stereopsis and other vision-related parameters, including BCVA, letter contrast sensitivity, metamorphopsia, and aniseikonia, were examined using the Spearman rank correlation test. All statistical analyses were performed by SPSS software 25.0 (SPSS, Chicago, IL, USA). A P value < 0.05 was considered to indicate statistical significance.
Results
Forty-five eyes of 45 patients (20 men and 25 women) with a mean age of 66.6 ± 11.4 years who were diagnosed with BRVO were included in the study. All patients had unilateral BRVO and were treated with IVR injections without complications such as RD, endophthalmitis, myocardial infarction or cerebral infarction.
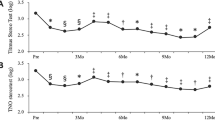
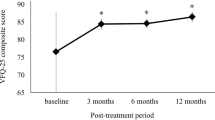
Table 1 shows visual functions before and after IVR treatment. IVR significantly improved BCVA (P < 0.001), stereopsis according to the TST (P < 0.001) and TNO (P < 0.001), and letter contrast sensitivity (P < 0.001). The severity of metamorphopsia and the degree of aniseikonia were not improved by IVR treatment. At baseline, stereopsis according to the TST was significantly correlated with BCVA (P < 0.001) and letter contrast sensitivity (P < 0.001). Similarly, the TNO score was significantly correlated with BCVA (P < 0.001) and letter contrast sensitivity (P < 0.001) (Table 2).
After IVR treatment, the TST score was significantly correlated with BCVA (P < 0.001), letter contrast sensitivity (P < 0.001), and degree of aniseikonia (P < 0.01), and the TNO score was significantly correlated with BCVA (P < 0.001) and letter contrast sensitivity (P < 0.001) (Table 3).
As shown in Table 4, stereopsis after treatment according to TST was significantly correlated with BCVA at baseline (P < 0.001) (Fig. 1A) but not with other visual functions. Similarly, stereopsis after treatment according to TNO was significantly correlated with BCVA at baseline (P < 0.001) (Fig. 1B) but not with other visual functions.
Discussion
IVR treatment in patients with BRVO improved not only their visual acuity but also stereopsis and letter contrast sensitivity. Several large clinical trials also showed that IVR improved visual acuity in patients with BRVO [25,26,27]. IVR treatment for BRVO [2] and vitrectomy for rhegmatogenous RD [19] and ERM [22] have been reported improve stereopsis. However, metamorphopsia and aniseikonia were not improved by IVR therapy. Sugiura et al. and Osaka et al. reported that eyes with BRVO often had persistent metamorphopsia after IVR treatment, even when visual acuity and retinal morphology were improved [6, 28].
A study revealed that stereopsis for BRVO patients and IVR treatment improved stereopsis albeit not to a normal level [2]. However, no study has clarified which visual functions affect stereopsis. Therefore, we designed this study to identify vision- related parameters that affect stereopsis. This is the first study to report vision-related parameters that affect stereopsis in patients with unilateral BRVO.
There were significant relationships between stereopsis (according to TST and TNO) and BCVA at baseline and after treatment in this study. Furthermore, TST and TNO scores after treatment were significantly correlated with BCVA at baseline. This indicates that initial visual acuity may be a prognostic factor for stereopsis after treatment. Stereopsis was correlated with visual acuity in patients after surgery for RD [29] and MH [20]. It is well known that stereopsis is related to visual acuity [7, 10, 11, 30]. Stereopsis was worse in subjects with a large difference in visual acuity between the two eyes, and stereopsis and the difference in visual acuity between the two eyes were correlated [7]. Goodwin et al. showed that stereopsis was reduced as soon as visual acuity, both monocular and binocular, was reduced by cycloplegia or fogging with spherical lenses in normal adult volunteers with normal binocular single vision [11]. On the basis of previous studies, stereopsis may be most affected by visual acuity. However, our results revealed that visual acuity is not the only factor affecting stereopsis. The degrees of disturbance of visual acuity and stereopsis have been shown to be significantly correlated. A healthy subject whose visual acuity in one eye was impaired to 100/200 by a convex lens could discriminate from circle 9 to circle 8 in the TST [31]. However, in the present study, BRVO patients whose visual acuity improved to 180/200 after IVR treatment could discriminate only circle 4 in the TST.
TST and TNO scores were significantly correlated with changes in letter contrast sensitivity before and after treatment. Several studies have reported a relationship between contrast sensitivity and stereopsis [31,32,33,34,35]. Stereopsis improves with increasing contrast, unless the increase is monocular [31]. Schor et al. reported that stereo thresholds were elevated by binocular suppression, which was evoked by interocular differences in contrast [32]. Halpern et al. found that stereopsis for conventional (first-order) stimuli improved with increasing contrast with an approximate slope of –0.5 on log–log axes [33]. When the contrast observed by one eye was reduced to produce unequal monocular contrasts, the disparity threshold rose more than that when the contrast observed by the two eyes was reduced by the same amount [34]. Simons et al. reported that stereoacuity in a number of common clinical tests was reduced twice as much by degradation of the contrast of one eye’s image as by an equal reduction of contrast of the image in both eyes [35]. Disturbance of contrast sensitivity resulting from retinal diseases might worsen stereopsis.
The TST score was significantly correlated with the degree of aniseikonia after treatment. Previous studies revealed a relationship between stereopsis and aniseikonia [12,13,14]. Rutstein et al. reported that retinally induced aniseikonia resulted in poorer stereopsis with ERM, RD, or age-related macular degeneration [36]. Even if 1 dioptre made experimental anisometropia (~1% of aniseikonia) in normal subjects, stereopsis broke down [37]. Therefore, aniseikonia in patients with BRVO may contribute to the impairment of stereopsis.
This study has several limitations. First, the sample size was small and the follow-up period was short. Further longitudinal studies with more subjects will be necessary to verify our findings. Second, although other factors are known to affect stereopsis, such as pupil size [14, 16], eye dominance [12, 15], and accommodation [11, 17], we did not evaluate these factors. However, the effects of pupil size and eye dominance on stereopsis are subtle, and it is unlikely that our conclusions will change.
In summary, we assessed visual functions that affect stereopsis in 45 patients with BRVO before and after IVR treatment. Deterioration of stereopsis was associated with changes in visual acuity and contrast sensitivity before and after treatment. Initial visual acuity is a prognostic factor for posttreatment stereopsis.
Summary
What was known before
-
Stereopsis is impaired in patient with retinal disorder such as BRVO, ERM, MH and RD. No one know which visual function is affect stereopsis in patient with BRVO.
What this study adds
-
Deterioration of stereopsis in patients with BRVO is associated with changes in visual acuity and contrast sensitivity from before to after treatment.
References
Rabena MD, Pieramici DJ, Castellarin AA, Nasir MA, Avery RL. Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina 2007;27:419–25.
Morikawa S, Okamoto F, Sugiura Y, Murakami T, Hiraoka T, Oshika T. Stereopsis after intravitreal ranibizumab injections for branch retinal vein occlusion. Ophthalmol Retin. 2019;3:777–83.
Noma H, Funatsu H, Harino S, Nagaoka T, Mimura T, Hori S. Influence of macular microcirculation and retinal thickness on visual acuity in patients with branch retinal vein occlusion and macular edema. Jpn J Ophthalmol. 2010;54:430–4.
Sugiura Y, Okamoto F, Murakami T, Morikawa S, Hiraoka T, Oshika T. Time course of changes in contrast sensitivity following intravitreal ranibizumab injection for branch retinal vein occlusion. Jpn J Ophthalmol. 2020;64:497–505.
Preti RC, Ramirez LM, Pimentel SL, Motta AA, Machado CG, Monteiro ML. Single intravitreal bevacizumab injection effects on contrast sensitivity in macular edema from branch retinal vein occlusion. Arq Bras Oftalmol. 2012;75:29–32.
Sugiura Y, Okamoto F, Morikawa S, Okamoto Y, Hiraoka T, Oshika T. Time course of changes in metamorphopsia following intravitreal ranibizumab injection for branch retinal vein occlusion. Retina 2018;38:1581–7.
Lam AK, Chau AS, Lam WY, Leung GY, Man BS. Effect of naturally occurring visual acuity differences between two eyes in stereoacuity. Ophthalmic Physiol Opt. 1996;16:189–95.
Donzis PB, Rappazzo JA, Burde RM, Gordon M. Effect of binocular variations of Snellen’s visual acuity on Titmus stereoacuity. Arch Ophthalmol. 1983;101:930–2.
Larson WL, Bolduc M. Effect of induced blur on visual acuity and stereoacuity. Optom Vis Sci. 1991;68:294–8.
Levy NS, Glick EB. Stereoscopic perception and Snellen visual acuity. Am J Ophthalmol. 1974;78:722–4.
Goodwin RT, Romano PE. Stereoacuity degradation by experimental and real monocular and binocular amblyopia. Investig Ophthalmol Vis Sci. 1985;26:917–23.
Erickson P, McGill EC. Role of visual acuity, stereoacuity, and ocular dominance in monovision patient success. Optom Vis Sci. 1992;69:761–4.
Katsumi O, Tanino T, Hirose T. Effect of aniseikonia on binocular function. Investig Ophthalmol Vis Sci. 1986;27:601–4.
Lovasik JV, Szymkiw M. Effects of aniseikonia, anisometropia, accommodation, retinal illuminance, and pupil size on stereopsis. Investig Ophthalmol Vis Sci. 1985;26:741–50.
Weinman J, Cooke V. Eye dominance and stereopsis. Perception 1982;11:207–10.
Pierce DM. Comparability of two methods of estimating real-depth acuity. Ophthalmologica 1975;171:224–35.
Kani W. Stereopsis and spatial perception in amblyopes and uncorrected ametropes. Br J Ophthalmol. 1978;62:756–62.
Asaria R, Garnham L, Gregor ZJ, Sloper JJ. A prospective study of binocular visual function before and after successful surgery to remove a unilateral epiretinal membrane. Ophthalmology 2008;115:1930–7.
Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Stereopsis and optical coherence tomography findings after epiretinal membrane surgery. Retina 2015;35:1415–21.
Hikichi T, Onodera A, Ishiko S, Fujio N, Mori F, Yoshida A. Stereo acuity in patients with unilateral macular hole and after unilateral macular hole surgery. Graefes Arch Clin Exp Ophthalmol. 2001;239:128–32.
Mireskandari K, Garnham L, Sheard R, Ezra E, Gregor ZJ, Sloper JJ. A prospective study of the effect of a unilateral macular hole on sensory and motor binocular function and recovery following successful surgery. Br J Ophthalmol. 2004;88:1320–4.
Watanabe H, Okamoto F, Sugiura Y, Hoshi S, Okamoto Y, Hiraoka T, et al. Stereopsis after successful surgery for rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 2014;252:1207–12.
Matsumoto C, Arimura E, Okuyama S, Takada S, Hashimoto S, Shimomura Y. Quantification of metamorphopsia in patients with epiretinal membranes. Investig Ophthalmol Vis Sci. 2003;44:4012–6.
Arimura E, Matsumoto C, Okuyama S, Takada S, Hashimoto S, Shimomura Y. Retinal contraction and metamorphopsia scores in eyes with idiopathic epiretinal membrane. Investig Ophthalmol Vis Sci. 2005;46:2961–6.
Brown DM, Campochiaro PA, Bhisitkul RB, Ho AC, Gray S, Saroj N, et al. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology 2011;118:1594–602.
Heier JS, Campochiaro PA, Yau L, Li Z, Saroj N, Rubio RG, et al. Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology 2012;119:802–9.
Tan MH, McAllister IL, Gillies ME, Verma N, Banerjee G, Smithies LA, et al. Randomized controlled trial of intravitreal ranibizumab versus standard grid laser for macular edema following branch retinal vein occlusion. Am J Ophthalmol. 2014;157:237–47.
Osaka R, Manabe K, Manabe S, Nakano Y, Takasago Y, Shiragami C, et al. Persistent metamorphopsia associated with branch retinal vein occlusion. PLoS ONE. 2018;13:e0204015.
Amemiya T, Takami H, Yoshida H, Harayama K. Binocular visual function after surgery for detached retina. Graefes Arch Clin Exp Ophthalmol. 1982;218:304–6.
Burian HM. Anomalous retinal correspondence. Its essence and its significance in diagnosis and treatment. Am J Ophthalmol. 1951;34:237–53.
Stevenson SB, Cormack LK. A contrast paradox in stereopsis, motion detection, and vernier acuity. Vis Res. 2000;40:2881–4.
Schor C, Heckmann T. Interocular differences in contrast and spatial frequency: effects on stereopsis and fusion. Vis Res. 1989;29:837–47.
Halpern DL, Blake RR. How contrast affects stereoacuity. Perception 1988;17:483–95.
Legge GE, Gu YC. Stereopsis and contrast. Vis Res. 1989;29:989–1004.
Simons K. Effects on stereopsis of monocular versus binocular degradation of image contrast. Investig Ophthalmol Vis Sci. 1984;25:987–9.
Rutstein RP. Retinally induced aniseikonia: a case series. Optom Vis Sci. 2012;89:e50–5.
Brooks SE, Johnson D, Fischer N. Anisometropia and binocularity. Ophthalmology 1996;103:1139–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morikawa, S., Okamoto, F., Murakami, T. et al. Visual functions affecting stereopsis in patients with branch retinal vein occlusion. Eye 36, 457–462 (2022). https://doi.org/10.1038/s41433-021-01452-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01452-x
This article is cited by
-
Binocular metamorphopsia in patients with branch retinal vein occlusion: a multi-center study
International Ophthalmology (2023)