Abstract
Background
To compare functional staging classifications in Vietnamese patients with primary open angle glaucoma (POAG) and chronic primary angle closure glaucoma (PACG).
Methods
A retrospective cross-section study was conducted at a national setting. Two hundred seven eyes of 207 patients were recruited. Patients were tested with standard automated perimetry. Field loss was generally classified in four stages (normal, early, moderate, and severe), using four classification strategies: (1) Hodapp–Parrish–Anderson (HPA), (2) enhanced Glaucoma Staging System (eGSS), (3) modified Glaucoma Staging System (mGSS) and (4) the Advanced Glaucoma Intervention Study (AGIS). AGIS as a standard method was used to judge the staging performance of the other three classifications in terms of agreement (Cohen Kappa—K) and association (Chi-Square Test—Cramer’s V).
Results
The agreement between AGIS and mGSS (K = 0.687; p < 0.001) and HPA (K = 0.686; p < 0.001) was substantial while that between AGIS and eGSS was slight (K = 0.103; p < 0.001). The association between AGIS and mGSS (V = 0.748; p < 0.001) and HPA (V = 0.748; p < 0.001) was greater than eGSS (V = 0.594; p < 0.001).
Conclusions
MGSS and HPA showed stronger agreement and closer association with AGIS than eGSS. We recommend mGSS should be used in managing a glaucoma clinic because of its simplicity and convenience over HPA and AGIS.
Similar content being viewed by others
Introduction
Changes are needed to improve patient throughput and clinic efficiency in current glaucoma clinics as most public sector glaucoma clinics are overbooked and unable to manage their patient load due to increased demand from an ageing population, increasing prevalence of glaucoma and reduced health budgets. Regular visual field testing and their clinical interpretation are crucial components of glaucoma care, but are time consuming and burdening the service. More reliable and rapid visual field analysis would improve clinic efficiency by triaging patients into broad severity categories and, by stratifying patients into severity groups, improve infrastructure and resource allocation. Patients with less severe glaucoma would have less frequent appointments and could be managed in community-based multi-disciplinary clinics, while those with more severe glaucoma would be managed in the higher acuity hospital based glaucoma clinic.
Since the first Glaucoma Staging System of American Medical Association was proposed in 1958, there have been approximately 20 glaucoma staging classifications, but no method has become widely recognized as the gold standard [1]. Some of the more popular staging systems include Hodapp–Parrish–Anderson (HPA) [1], The Advanced Glaucoma Intervention Study (AGIS) score [2], and the enhanced Glaucoma Staging System (eGSS) [3]. However, these staging systems have various issues including a lack of detailed categorization (HPA), difficulty implementing the system in clinical practice (HPA, AGIS) or difficulty differentiating between the normal and glaucomatous condition (eGSS).
Hirasawa et al. proposed a modified Glaucoma Staging System (mGSS) in 2013 based on the Bascom Palmer GSS. The advantage of mGSS over other staging systems was its capability of definitive diagnosis (using Anderson criteria [4, 5]) and good staging performance. MGSS was also suitable for daily practice since it was simply based on VFI compared with other methods. However, mGSS could not work with 10–2 test [6].
Whether mGSS is more useful than more popular approaches such as HPA [7] and eGSS [3] is still debated. The current study aimed to compare the mGSS, HPA, and eGSS, using AGIS as the standard system to judge other systems since AGIS has been used in previous studies as a standard comparator. A detailed overview of existing Glaucoma Staging Systems can be found in the Supplementary material.
Materials and methods
This retrospective study followed the tenets of the Declaration of Helsinki and was approved by Hanoi Medical University and Vietnam National Institute of Ophthalmology (VNIO) Ethics Committees. All participants were provided with informed consent and signed the consent form.
The medical records of sequential patients with primary open angle glaucoma (POAG) or chronic primary angle closure glaucoma (PACG) who attended the outpatient service of Glaucoma Department, VNIO with at least two appointments and two visual fields tests between 2011 and 2017 were reviewed. POAG was diagnosed based on characteristic optic disc changes and/or glaucomatous visual field loss demonstrated on the Humphrey Visual Field Analyzer (HFA) II—i (Humphrey Instruments, Inc., Zeiss Humphrey, San Leandro, CA) and an open anterior chamber angle on gonioscopy. PACG was diagnosed based on similar optic disc and/or visual field findings, and the current or previous presence of a narrow or closed drainage angle requiring an angle-widening intervention (such as a laser iridotomy or trabeculectomy).
Patients with incomplete medical records, without glaucoma, with secondary causes of glaucoma or substantial non-glaucomatous ophthalmologic co-morbidity, and those with unreliable visual fields were excluded from the study. We analyzed one eye per patient. When patients had two eligible eyes, one was selected at random. Data of every two consecutive patients with two eligible eyes were fully inputted in any pattern (right eye–left eye–right eye–left eye, right eye–left eye–left eye–right eye, left eye–right eye–right eye–left eye, or left eye–right eye–left eye–right eye). Eyes with even ordinal numbers were chosen.
Each patient had a thorough history and complete ocular examination performed. They were tested with standard automated perimetry (program 24–2, Swedish Interactive Thresholding Algorithm, HFA II—i, Carl Zeiss Meditec, Inc, Dublin, CA). Reliable visual field indices were set at fixation loss < 20%, false negatives < 33%, and false positives < 15% [8].
Each system has its own way of subdividing each stage into smaller sub-stages for the fine categorization to detect progression and therefore have different numbers of stages. To unify the staging methods, we followed the methodology of Ng et al. [9]. and Brusini et al. [10] and used a general, integrated classification (IC) system for glaucoma severity (normal, early, moderate, and severe) (Table 1). We assessed four different staging methods: HPA, eGSS, mGSS, and AGIS. The AGIS classification was used as the standard system to judge the staging performance of the other three classifications in terms of agreement and association because of its demonstrated effectiveness and reliability in staging glaucoma functional damages [2]. Cohen Kappa (K) was selected to assess the agreement among staging methods, and Chi-Square Test (Cramer’sV) was chosen to evaluate the association among them. Data were analyzed with SPSS online version (provided by The University of Sydney).
Results
From 578 patients attending the glaucoma outpatient clinic at VNIO between January 2011 and December 2017, 207 patients met the eligible criteria. All participants were Vietnamese and at the mean age of 50.8 ± 17.04 (18; 80) with more female than male (58% compared with 42%).
POAG was the predominant type of glaucoma, accounting for 73.4% of the study population. Table 2 details the pinhole visual acuity (PHVA) as this is the normal practice at VNIO, intraocular pressure (IOP), and visual field indices stratified by the type of glaucoma and enrolled eye.
The mean PHVA (logMAR), IOP, mean deviation (MD), pattern deviation (PSD), and visual field index (VFI) were 0.48 ± 0.39 (0; 2), 15.91 ± 3.93 mmHg (5; 34), −13.44 ± 7.94 dB (−30.1; −0.97), 7.1 ± 3.91 dB (1.02; 16.32), and 68.07 ± 26.34% (9; 100); respectively.
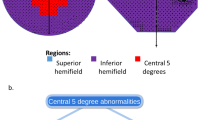
The distribution of glaucoma severity using the HPA and mGSS staging system was almost identical. HPA, mGSS, and AGIS ended with a roughly similar number of eyes graded with severe glaucoma, whereas eGSS had a much higher number of eyes with severe glaucoma compared with the other grading systems (Fig. 1a). Average VFI distribution across stages of HPA, mGSS and AGIS appreared to tie together compared with eGSS (Fig. 1b).
There was only slight agreement between eGSS and HPA (K = 0.088, p = 0.02) and mGSS (K = 0.105, p < 0.001). In contrast, there was almost perfect agreement and association between HPA and mGSS (K = 0.948, p < 0.001; Cramer’s V = 0.957, p < 0.001) (Table 3).
The agreement between AGIS and mGSS (K = 0.687, p < 0.001) and HPA (K = 0.686, p < 0.001) was substantial while the agreement between AGIS and eGSS was low (K = 0.103; p < 0.001). The level of association between AGIS and mGSS (Cramer’s V = 0.748, p < 0.001) and HPA (Cramer’s V = 0.748, p < 0.001) was also higher compared with eGSS (Cramer’s V = 0.594, p < 0.001) (Table 4).
Discussion
The current study judged the performance of HPA, mGSS, and eGSS by comparing systems with AGIS. Each classification system has its own strengths and weaknesses.
The level of agreement and association between HPA, mGSS and eGSS was significant. However, AGIS had stronger agreement and association with HPA (K = 0.686, V = 0.748) and mGSS (K = 0.687, V = 0.748) compared with eGSS (K = 0.103, V = 0.594). These results suggest that eGSS was less consistent with AGIS than HPA and mGSS.
Compared with the other three methods, eGSS had a higher percentage of eyes classified as having severe glaucoma, suggesting that eGSS overestimates the severity of glaucoma. This finding was similar to studies by Hirasawa [6] and Ng [9] in which eGSS tended to stage the progression more severely compared with others.
MGSS and HPA take into account paracentral defects (numerical scale) and Pattern Deviation Probability Plot. Like HPA and mGSS, AGIS takes into account peripheral and central defects (nasal area and hemifields) by scoring each test points. EGSS completely relies on MD and PSD, so cataract, aging changes and artefacts could influence the staging results (false positive diagnosis or overestimation). The consensus between AGIS and HPA and mGSS was stronger than that between AGIS and eGSS; thus, this result makes intuitive sense.
HPA has similar levels of agreement with mGSS, but has fewer severity catergories. EGSS is easy to use, but it could not differentiate between a normal and abnormal field and may even exaggerate the damage. Overall, mGSS is a better choice for day-to-day practice. Anderson criteria [4] needs to be used in stage 0 of mGSS to definitively diagnose glaucomatous visual field loss.
From a different view, due to the fluctuation among different tests, two patients with similar levels of disease might fall into either sides of a cutoff value and be treated differently. The innovation of perimetric technologies has paved the way for the employment of Guided Progression Analysis (GPA) as a replacement for traditional staging systems in many centers to detect glaucoma progression. Hence, the severity of glaucoma patients graded by mGSS should be carefully interpreted in combination with GPA to judge the progression to a new stage. In the future, software could be developed to automatically classify severity, using more complex and better validated systems, e.g., AGIS.
Staging systems are important for health management reporting, policy making, fund raising, health care resources optimizing, and patient education, as they provide a rapid and reliable assessment of glaucoma severity in individual patients at each visit. A simple and accurate staging system would aid trained health care workers (e.g., nurses) to assess the severity of glaucoma independently and then report to clinicians and managers. With this data, clinicians can shorten the intervals between visits for patients with rapidly progressing glaucoma. Figure 2 illustrates a currently used Glaucoma Staging System to classify the patient appointments at Sydney Eye Hospital (SEH), which is more complicated than mGSS. With this classification, administrators and glaucoma consultants at SEH can effectively manipulate the patient flow and prioritize urgent cases. Doctors can provide patients with an easy-to-understand quantitative measure of glaucoma severity by giving them the level of staging; hence, patients can get an insight into the severity of their glaucoma. For reasons disscussed above, precisely staging the progression of chronic diseases such as glaucoma has great potential to improve the efficiency of clinics and maximize the visual outcomes of patients.
There are limitations in this study. Although there were 578 medical records, only 207 records were eligible due to incomplete data and in particular, a lack of reliable visual field reports. Furthermore, there are few recent studies to compare results. As a retrospective review of medical records, there may have been selection bias, misclassification bias, and variable incomplete clinical data so our results need to be interpreted with caution. When reviewing previous papers of the same research topic, we did not find any analysis on the effects of prior cataract surgery. Hence, we did not record whether the patients had any history of cataract surgery. VNIO is the main referral eye hospital of the North Vietnam, and there is only one HFA II machine for the entire hospital. Therefore, the glaucoma department is always overloaded. Although the results are not recorded due to lack of time, patients are still corrected for near vision to perform the visual field test. According to Quigley, perimetric defects occurred when 25–35% ganglion cells had gone [11]; hence, agreements among a structural maker, for example Disc Damage Likelihood Scale, and other functional staging systems might be insignificant in terms of glaucomatous damage detection. Therefore, we did not analyse this relationship in our study.
The current study has several strengths. This study was conducted in VNIO, a major tertiary referral eye setting in Vietnam. As VNIO patients come from all provinces in Vietnam, the findings of this study are representatives of the pattern of glaucoma for the entire country, and are applicable to other eye care settings. The present study recruited 207 eyes of 207 patients from 578 outpatient records, which is comparable to other published studies of glaucoma such as 104 eyes [12], 200 eyes [3] and 121 eyes [10] of Brusini et al., and 235 eyes of Hirasawa et al. [6].
Previous studies only included patients with POAG [3, 6, 9, 10, 12, 13] while the current study included those with chronic PACG. Evidence indicates that PACG is predominant among Asian populations in general [14,15,16] and Vietnamese population in particular [17, 18]. Thus, by applying staging systems to chronic PACG patients, this study has enriched the previous findings.
In conclusion, mGSS, HPA, and eGSS all had significant association, and agreement with AGIS. However, mGSS and HPA had stronger agreement and closer association with AGIS than eGSS. The mGSS classification system has simplicity and convenience, highlighting the advantages of using this system to manage glaucoma patient flow in busy public sector clinics. MGSS offers the promise of more rapid and accurate patient management, which could enable the correct interventions in the correct patients at the correct time resulting in improved patient outcomes.
Summary
What was known before
-
The modified Glaucoma Staging System (GSS) could perform equally or even superiorly to Bascom Palmer GSS and enhanced GSS.
-
The mGSS was clinically applicable.
What this study adds
-
Confirming previous findings of Hirasawa et al.
-
Enriching those findings by recruiting not only POAG but also chronic PACG patients.
-
Highlighting the clinical importance of the staging system in managing the glaucoma patient flow, which was poorly discussed in previous publications.
References
Brusini P, Johnson CA. Staging functional damage in glaucoma: review of different classification methods. Surv Ophthalmol. 2007;52:156–79.
Advanced Glaucoma Intervention Study. 2. Visual field test scoring and reliability. Ophthalmology. 1994;101:1445–55.
Brusini P, Filacorda S. Enhanced Glaucoma Staging System (GSS 2) for classifying functional damage in glaucoma. J Glaucoma. 2006;15:40–46.
Chakravarti T. Assessing precision of Hodapp-Parrish-Anderson criteria for staging early glaucomatous damage in an ocular hypertension cohort: a retrospective study. Asia-Pac J Ophthalmol. 2017;6:21–7.
Anderson DRP, Patella Vincent Michae. Automated static perimetry. St. Louis: Mosby; 1999.
Hirasawa K, Shoji N, Morita T, Shimizu K. A modified glaucoma staging system based on visual field index. Graefe’s Arch Clin Exp Ophthalmol = Albrecht von Graefes Arch fur klinische und experimentelle Ophthalmologie. 2013;251:2747–52.
Hodapp E PRI, Anderson DR. Clinical decisions in glaucoma, 1st ed. St Louis: Mosby; 1993.
Tan NYQ, Tham Y-C, Koh V, Nguyen DQ, Cheung CY, Aung T, et al. The effect of testing reliability on visual field sensitivity in normal eyes: the singapore chinese eye study. Ophthalmology. 2018;125:15–21.
Ng M, Sample P, Pascual J, Zangwill L, Girkin C, Liebmann J, et al. Comparison of visual field severity classification systems for glaucoma. J Glaucoma. 2012;21:551–61.
Brusini P. Five-stage glaucoma damage classification using FDT indices. Acta Ophthalmol Scand Suppl. 2002;236:21–2.
Malik R, Swanson WH, Garway-Heath DF. ‘Structure-function relationship’ in glaucoma: past thinking and current concepts. Clin Exp Ophthalmol. 2012;40:369–80.
Brusini P, Tosoni C. Staging of functional damage in glaucoma using frequency doubling technology. J Glaucoma. 2003;12:417–26.
Kocak I, Zulauf M, Bergamin O. Evaluation of the Brusini glaucoma staging system for typing and staging of perimetric results. Ophthalmol J Int d’ophtalmol Int J Ophthalmol Z Augenheilkd. 1998;212:221–7.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Kapetanakis VV, Chan MP, Foster PJ, Cook DG, Owen CG, Rudnicka AR. Global variations and time trends in the prevalence of primary open angle glaucoma (POAG): a systematic review and meta-analysis. Br J Ophthalmol. 2016;100:86–93.
Cho HK, Kee C. Population-based glaucoma prevalence studies in Asians. Surv Ophthalmol. 2014;59:434–47.
Nguyen N, Mora JS, Gaffney MM, Ma AS, Wong PC, Iwach AG, et al. A high prevalence of occludable angles in a Vietnamese population. Ophthalmology. 1996;103:1426–31.
Peng PH, Manivanh R, Nguyen N, Weinreb RN, Lin SC. Glaucoma and clinical characteristics in Vietnamese Americans. Curr eye Res. 2011;36:733–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hoang, T.T., Van Bui, A., Nguyen, V. et al. Comparison of perimetric Glaucoma Staging Systems in Asians with primary glaucoma. Eye 35, 973–978 (2021). https://doi.org/10.1038/s41433-020-1012-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1012-z