Abstract
Background/Objectives
To identify risk factors for glaucoma-related central visual field (VF) deterioration after vitrectomy with internal limiting membrane (ILM) peeling for epiretinal membrane (ERM).
Subjects/Methods
A prospective cohort study consisting of cases with or without glaucoma (33 eyes of 33 patients in each group) who underwent vitrectomy with ILM peeling for ERM. Humphrey 10–2 VFs and ganglion cell complex (GCC) thickness were measured at baseline and about 3, 6, and 12 months postoperatively. Longitudinal changes in VF indices and factors associated with their postoperative changes were investigated using mixed-effects models, as was sectorwise total deviation (TD) analysis using six sectors consisting of outer/inner arcuate and cecocentral sectors in each hemifield.
Results
VF mean deviation significantly deteriorated postoperatively only in the glaucoma group (P < 0.001). Older age, longer axial length, preoperative worse mean deviation, and thinner GCC were significant risk factors for postoperative deterioration (coefficient ± standard errors: −0.139 ± 0.067, −0.740 ± 0.241, 0.16 ± 0.07, 0.050 ± 0.020; P = 0.038, P = 0.002, P = 0.024, P = 0.012, respectively). Sectorwise analysis revealed that TD in the superior/inferior outer arcuate sectors significantly deteriorated only in the glaucoma group. Preoperative worse TD and thinner GCC were significant risk factors for deterioration in the superior outer arcuate sector (0.65 ± 0.11, 0.08 ± 0.03; P < 0.001, P = 0.042, respectively).
Conclusions
Central VF deterioration, especially in the outer arcuate sectors, found to be glaucoma-related changes after vitrectomy with ILM peeling for ERM. Preoperative worse VF and thinner GCC were identified as risk factors for postoperative VF deterioration.
Similar content being viewed by others
Introduction
Pars plana vitrectomy (PPV) is the standard treatment for epiretinal membrane (ERM) to restore visual function. The time course for postoperative improvements has been shown for various aspects of visual function including visual acuity [1,2,3], metamorphopsia [1, 3], and aniseikonia [2, 3]. However, the visual field (VF) may become impaired after PPV for ERM especially when using internal limiting membrane (ILM) peeling [4,5,6].
Glaucoma, one of the most common causes of blindness worldwide, is sometimes found as a co-morbidity of macular disorders. On the other hand, ERM is a common macular pathology, and was reported to cause imaging artefacts in optical coherence tomography (OCT) in eyes with glaucoma [7]. Given that the global prevalence of glaucoma is predicted to increase in the future [8], the number of patients with glaucoma who undergo PPV for ERM will continue to increase. The central VF, which is often affected even in the early stages of glaucoma [9], has a significant impact on vision-related quality of life [10]. Therefore, the influence of ERM surgery on central VFs in eyes with coexisting glaucoma is an urgent issue to be addressed.
Postoperative VF deterioration in glaucomatous eyes was first reported in a small case series of patients with moderate to advanced glaucoma who underwent PPV for ERM or macular hole [11]. Recently, we also reported that PPV with ILM peeling for ERM or macular hole may cause VF damage within the central 10° in glaucomatous eyes [12]. However, we used Humphrey 24–2 VFs, which has 54 test points located in a 6° grid pattern in the central 24–30°, with only 12 test points within 10°.
The purpose of this study was to identify risk factors for glaucoma-related central VF deterioration after PPV with ILM peeling for ERM by comparing eyes with and without glaucoma using 10–2 VFs having 68 test points within 10°. Furthermore, we adopted a new 6-sector analysis for 10–2 VFs to reveal topographical characteristics of postoperative central VF changes.
Methods
Participants
This prospective cohort study (protocol ID: UMIN000035354) enrolled patients with ERM who underwent PPV with ILM peeling from May 2011 to June 2017 at Kanazawa University Hospital. The study protocol was approved by the Institutional Review Board of Kanazawa University Hospital, and was performed in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from each subject. Recruitment of patients with glaucoma started in May 2011, while that of patients without glaucoma was added from January 2015 in order to compare outcomes between two cohorts. Eighteen patients in the glaucoma group and 25 patients in the control group were also included in our previous study [12].
Ophthalmic examinations
ERM diagnosis was made by fundus examination, fundus photos and OCT imaging. Patients with other vision threatening diseases such as corneal diseases, visually significant cataract, uveitis, diabetic retinopathy, and macular degenerative diseases were excluded. Patients underwent preoperative ophthalmic examinations including measurement of best-corrected visual acuity (BCVA), slit-lamp examination, intraocular pressure (IOP) measurements using Goldmann applanation tonometry, axial length measurements (OA-1000, TOMEY, Tokyo, Japan), dilated fundus examination, fundus photography, VF tests (Humphrey VF Analyzer II, 24–2 and 10–2 Swedish interactive threshold algorithm, Humphrey-Zeiss instrument, Dublin, CA), and spectral-domain OCT scans (RS-3000 Retina Scan, Nidek Inc., Gamagori, Aichi, Japan). We did not enroll patients with poor quality OCT images due to image artefacts or low signal intensity in the preoperative examinations.
Glaucoma diagnosis
The criteria for glaucoma diagnosis were: (1) normal anterior segment with normal open-angle; (2) glaucomatous appearance of the optic disc (enlarged cupping and neuroretinal rim thinning) associated with retinal nerve fiber layer (RNFL) defects; and (3) reproducible VF defects in 24–2 VFs corresponding to the optic disc changes. Glaucomatous VF defects were defined as follows: (1) a cluster of three points with a probability <5% on a pattern deviation map in at least one hemifield including at least one point with a probability <1%; (2) glaucoma hemifield test results outside normal limits; or (3) pattern standard deviation <5%. Eyes in the control group had no glaucomatous optic disc abnormalities. Glaucoma types included were normal-tension glaucoma (IOP < 21 mmHg at all visits), primary open-angle glaucoma (IOP > 21 mmHg at ≥1 visits), and exfoliation glaucoma.
10–2 VF tests
The 10–2 VF tests were performed preoperatively and three times postoperatively. Postoperative VF tests of the operated eyes were scheduled at 3, 6, and 12 months in the control group, while the schedule was slightly modified in the glaucoma group because VF tests of the fellow eyes were also needed during the study periods in patients with bilateral glaucoma. VF results with fixation loss <20%, false positive error <15%, and false negative error <20% were considered to be reliable. Prior to preoperative 10–2 VF testing, all participants underwent 24–2 VF tests in both eyes for glaucoma diagnosis and for reducing VF learning effects [13]. When 10–2 VF results were unreliable or obviously abnormal, 10–2 testing was repeated and the second VF data were adopted.
For sectorwise VF analyses, total deviation (TD) was averaged within each of six sectors (superior outer [S/O] arcuate, superior inner [S/I] arcuate, superior cecocentral, inferior outer [I/O] arcuate, inferior inner [I/I] arcuate, and inferior cecocentral sectors; Fig. 1a). The six sectors were created referring to previous reports based on the orientation of the retinal ganglion cell (RGC) axon bundles toward the optic disc [14,15,16]. The anti-logged TD values for individual VF test points were averaged per sector then were logged to convert back to a dB scale to calculate average TD values [17].
a Each box indicates the 10–2 test points. The sectors are defined as follows: (1) superior outer arcuate, (2) superior inner arcuate, (3) superior cecocentral, (4) inferior outer arcuate, (5) inferior inner arcuate, and (6) inferior cecocentral sector. b Retinal view of the 10–2 test points adjusted for retinal ganglion cell displacement. The thickness of the ganglion cell complex was measured for each point (circular area with a radius of 0.8°). The outer circle shows the area of the central 10° from the fovea.
OCT measurement
Patients underwent OCT examination at each VF session. Macular raster OCT scans (128 vertical B-scans, each of which had 512 A-scans, over a 30 × 30° square area) were performed to measure ganglion cell complex (GCC; RNFL + ganglion cell layer + inner plexiform layer) thickness. We reviewed B-scan images consisting of raster scans, and manually corrected the segmentation lines for GCC as needed at the retinal locations for GCC thickness measurements. The segmentation line was set to the ERM surface where ERM was tightly attached to the retinal surface, while it was set to the retinal surface where ERM was apparently detached from the retina. GCC thickness at the retinal locations corresponding to each 10–2 VF test point, accounting for RGC displacement, was measured using a customized OCT software (Fig. 1b) [18, 19]. Sectorwise GCC thickness was obtained by averaging GCC thickness within each sector. We adopted only reliable OCT results without image artefacts or a low signal strength index ≤6). Using horizontal and vertical line scans across the fovea, ERM was classified into four stages according to the staging scheme [20]: stage 1, preserved foveal pit and well-defined retinal layers; stage 2, absent foveal pit and well-defined retinal layers; stage 3, an ectopic inner foveal layer and well-defined retinal layers; stage 4, an ectopic inner foveal layer and disrupted retinal layers.
Surgical procedures
PPV with small-gauge instruments was performed by a single surgeon (TH) as described previously [12]. Triamcinolone acetonide (MaQaid®, Wakamoto Pharmaceutical, Tokyo, Japan) was utilized in all cases. Briefly, the ERM was directly grasped and peeled with end-gripping forceps. All cases underwent ILM peeling. To visualize the residual ILM after ERM peeling, triamcinolone acetonide was reinjected, and brilliant blue G (BBG; ILM-Blue®, DORC International, Zuidland, The Netherlands) was used in recent cases. After staining, the residual ILM was directly grasped and peeled with end-gripping forceps within the area of ~10° eccentricity from the fovea. ERM and ILM peeling were usually initiated from the superior quadrant. Cataract surgery using phacoemulsification with intraocular lens implantation was combined with PPV in phakic patients.
Assessment of postoperative dissociated optic nerve fiber layer (DONFL) appearance
A DONFL appearance, characterized by numerous arcuate striae darker than the surrounding retinal surface [21], was determined using blue-filtered fundus photographs and en face OCT images obtained at all postoperative visits.
Statistical analyses
Preoperative demographic data were compared between two groups (i.e., glaucoma vs. control groups) using standard statistical procedures as indicated in Table 1. Linear mixed-effects models with subject-specific random effects were employed following analysis; sectorwise between-group comparisons of preoperative 10–2 TD and GCC thickness, longitudinal changes in BCVA, IOP, GCC thickness, 10–2 MD/PSD, and TD in each sector, relationship between GCC thickness and 10–2 TD in each sector, and multivariate analysis for factors associated with postoperative changes in 10–2 MD and sectorwise TD in each group. For the sectorwise analysis, values in different sectors of the same eye were treated as repeated measurements, and the sector order was included as a categorical variable in the interaction term with other variables accounting for the possible intersectoral correlation in the same eye [22]. The continuous variables in the interaction terms were centered at their mean values. To consider possible influence of the interval between surgery and VF tests in the analysis of longitudinal changes in variables, the interval was adopted as a covariate for subject-specific random slopes, and was also included as an independent variable in the multivariate analysis. The independent variables included in the multivariate analysis are shown in Supplementary Tables 1–3. Statistical analyses were performed with Stata software (version 16.0; StataCorp, TX) and SPSS (version 23.0; SPSS Inc., Chicago, IL). The statistical significance level was set as P < 0.05, and the Bonferroni correction for multiple comparisons was applied as indicated. The sample size was set to detect a difference of 0.5 standard deviations with an α error of 0.05 and a power of 80% for paired comparisons of preoperative and postoperative VFs.
Results
Sixty-six eyes of 66 patients were included in this study (33 eyes in the control group and 33 eyes in the glaucoma group). Patient characteristics in each group are shown in Table 1. The number of normal-tension glaucoma, primary open-angle glaucoma, exfoliation glaucoma was 25, 6, and 2, respectively. BBG was significantly more commonly used in the control group than the glaucoma group due to different enrollment periods for two groups. There were no significant intraoperative or postoperative complications in any cases. Two patients with exfoliation glaucoma had a history of phaco-trabeculotomy before PPV. None of the glaucomatous patients underwent additional glaucoma surgeries in the follow-up periods. The interval between surgery and each postoperative VF session did not differ significantly between two groups. Preoperative mean TD in the S/O, S/I, and I/O arcuate sectors was significantly lower in the glaucoma group than in the control group (P < 0.001 for each) (Supplementary Fig. 1A). Mean GCC thickness in the S/O and S/I arcuate sectors was significantly thinner in the glaucoma group than in the control group (P = 0.006 and P = 0.042, respectively) (Supplementary Fig. 1B).
DONFL was detected at the first postoperative visits in all of eight cases; one patient each for stages 1, 2, and 4 ERM in the glaucoma group, and one patient with stage 2, three patients with stage 3, and one patient with stage 4 ERM in the control group. The incidence rate of DONFL was not statistically different between different ERM stages (P = 0.36, Fisher’s exact test).
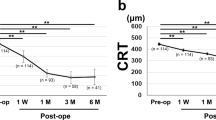
Regarding the longitudinal changes in parameters, BCVA significantly improved postoperatively in both groups (P < 0.001). IOP in the control group significantly decreased 3 months after surgery (P = 0.046), then recovered to the preoperative level thereafter. In the glaucoma group, IOP significantly increased 12 months after surgery (P = 0.032). GCC thickness significantly decreased in both groups (P < 0.001) (Supplementary Fig. 2). The 10–2 MD and PSD were stable in the control group, but significantly deteriorated postoperatively in the glaucoma group (P < 0.001) (Fig. 2).
a 10–2 mean deviation, b 10–2 pattern standard deviation. Estimated marginal mean from the linear mixed-effects models with an interaction term of group (i.e., glaucoma vs. control) and visual field session order as an independent variable was plotted for each group at each postoperative session. Error bars = 95% confidence interval. Solid and dashed lines indicate the control and glaucoma groups, respectively. f/u follow-up session. *P < 0.05 after Bonferroni correction.
Antiglaucoma medications were discontinued after surgery for all patients in the glaucoma group, and were added in the follow-up periods as needed. Therefore, medication score decreased at the 1st postoperative visit (1.3 ± 1.3 vs. 0.9 ± 1.2, P = 0.015), then returned to the baseline level thereafter.
Factors associated with 10–2 MD changes after PPV
In the multivariate analysis (Supplementary Table 1), MD changes were significantly worse in eyes with DONFL than in eyes without (P = 0.001), and preoperative worse 10–2 MD were significantly associated with MD improvement in the control group (P = 0.001). In the glaucoma group, older age, longer axial length, preoperative worse 10–2 MD and thinner GCC were significant risk factors for MD deterioration (P = 0.038, P = 0.002, P = 0.024, P = 0.012, respectively). ERM stages, baseline IOP, combined cataract surgery, and the interval between surgery and VF tests were not associated with MD changes in either group. Preoperative medication score and BBG usage were not associated with MD deterioration in the glaucoma group.
Sectorwise TD changes after PPV and their relationships with preoperative GCC thickness or TD values
In the glaucoma group, TD in the S/O arcuate sector was significantly deteriorated at all postoperative visits (P < 0.001, each), while, in the I/O arcuate sector, TD showed a transient worsening at the first postoperative visit (P < 0.001). In contrast, the control group showed a small but significant improvement in TD in the I/O and I/I arcuate sectors (I/O sector, P = 0.01–0.045 at three postoperative visits; I/I sector, P = 0.029 and P = 0.020 at 3 and 6 months, respectively) (Fig. 3).
a Superior outer arcuate, b superior inner arcuate, c superior cecocentral, d inferior outer arcuate, e inferior inner arcuate, and f inferior cecocentral sector. Estimated marginal means from the linear mixed-effects models are plotted for each postoperative session. Error bars = 95% confidence interval. Solid and dashed lines indicate the control and glaucoma groups, respectively. f/u follow-up session. *P < 0.05 after Bonferroni correction. TD total deviation.
The scatter plots for the relationship between postoperative TD changes and baseline values of GCC thickness or TD in all 10–2 VF sectors showed a TD decease of ≥5 dB occurred only in the glaucoma group (Fig. 4). Of note, no VF sectors with corresponding baseline GCC thickness of ≥150 µm had a TD decease of ≥5 dB, while even VF sectors with almost intact baseline TD values did.
TD changes in all 10–2 VF sectors of all patients at all postoperative sessions in the glaucoma (a, c) or control (b, d) groups were plotted against preoperative GCC thickness at the matched retinal locations (a, b) or baseline TD values (c, d). TD total deviation, VF visual field, GCC ganglion cell complex.
Factors associated with sectoral TD changes
Regarding factors associated with sectorwise TD changes in the control group, preoperative TD was negatively associated with postoperative TD changes in all sectors (P < 0.001), indicating that worse preoperative TD is linked with postoperative TD improvement. TD changes in the inferior cecocentral sector were significantly worse in eyes with DONFL than in eyes without (P = 0.042) (Supplementary Table 2). In contrast, preoperative TD in the S/O and I/I arcuate sectors and both superior and inferior cecocentral sectors was positively associated with postoperative TD changes in the glaucoma group (P < 0.001, P < 0.001, P = 0.03, P = 0.02, respectively), indicating that worse preoperative TD is predictive of postoperative TD deterioration. A thinner preoperative GCC was a significant risk factor for postoperative TD worsening in the S/O arcuate sector (P = 0.042, Supplementary Table 3).
Structure–function relationship in each sector
In the control group, GCC thickness in both preoperative and postoperative examinations had no clear correlations with TD in any sectors although some sectors showed significant but very weak correlations postoperatively. The eyes in the glaucoma group had more evident positive structure–function relationship postoperatively than preoperatively especially in the outer arcuate sectors (Supplementary Table 4).
Discussion
The present study demonstrated significant central VF deterioration, as evidenced by worsening of 10–2 MD and PSD, after PPV with ILM peeling for ERM only in eyes with glaucoma. The results corroborated our previous retrospective study using 24–2 VFs that showed the coexistence of glaucoma is a risk factor for postoperative central VF deterioration [12], which confirmed that central VF deterioration is a glaucoma-related adverse effect associated with surgery. The association of aging and longer axial length with 10–2 MD worsening in glaucomatous eyes was also in agreement with our prior study [12]. The 6-sector analysis revealed that outer arcuate sectors were the sites to be damaged in eyes with glaucoma. Furthermore, both worse VF and thinner GCC were the predictors of postoperative worsening of MD and TD in the S/O arcuate sector, indicating that eyes with advanced glaucoma are at higher risk of postoperative central VF deterioration.
In this study, sectorwise VF analysis was performed based on the orientation of the RGC axon bundles toward the optic disc given that the greatest mechanical stress generated by membrane peeling should be exerted on the retinal surface (i.e., RNFL). Direct mechanical damage to the RNFL caused by needles or forceps during membrane peeling has been shown to contribute to postoperative paracentral scotoma in eyes with macular hole [23]. We found that 10–2 VF deterioration in glaucomatous eyes was sector-dependent, and that the S/O and I/O arcuate sectors were the susceptible locations. These sectors include the macular area with thinner RNFL than other areas in healthy eyes [24]. The thin RNFL may be associated with vulnerability to mechanical damage caused by membrane peeling.
Intriguingly, these sectors showed different patterns of TD worsening, with sustained or transient worsening in the S/O or I/O arcuate sectors, respectively. One difference between these two VF sectors was that preoperative GCC was significantly thinner in the S/O arcuate (i.e., inferior macula) than in the I/O arcuate (i.e., superior macula, P = 0.02), while preoperative TD values in two sectors were almost the same. In glaucomatous eyes, these two sectors and the S/I arcuate sector had significantly lower TD values (i.e., glaucomatous VF defects) than in nonglaucomatous eyes. The S/O arcuate VF sector, which showed sustained TD worsening, had a thinner GCC than the I/O and S/I arcuate VF sectors, suggesting that inner retinal thickness may be an important determinant of retinal sensitivity deterioration by membrane peeling in the retinal area with glaucomatous VF defects. The initiation site of ILM peeling was in the I/O arcuate VF sector (i.e., superior macula). The transient worsening of TD in the I/O arcuate sector, but not in the S/I arcuate sector, indicates that the direct mechanical stress caused by the initiation of membrane peeling may cause reversible functional impairment of the RGCs.
ERM peeling without ILM peeling may be favorable for the prevention of VF deterioration. In order to facilitate ILM peeling, indocyanine green has commonly been used, although it was reported to have adverse effects on retinal sensitivity compared to BBG [25]. Even without indocyanine green, patients who underwent PPV with ILM peeling for ERM were found to have significantly delayed recovery of central retinal sensitivity and significantly greater number of absolute microscotomas in the central VFs compared with patients without ILM peeling [5]. A case series of ten patients with ERM showed that patients with decreased amplitudes in multifocal electroretinography after ILM peeling had new clusters of contiguous test points with increased threshold values in 10–2 VF testing [26]. However, it is rather difficult to remove an ERM while leaving the ILM intact, given that an ILM was present in all ERM specimens in this histological study [21]. Shimada et al. reported that only 34% of cases showed total ILM remaining after ERM peeling [27]. Furthermore, a meta-analysis reported that ILM peeling significantly reduced ERM recurrence without compromising the recovery of visual acuity [6]. Our present results from the control group, in which there was no significant deterioration of 10–2 VFs, support ILM peeling for ERM without using indocyanine green as a relatively safe and effective procedure, at least in nonglaucomatous eyes.
DONFL was originally characterized by Tadayoni et al. in a retrospective study showing that a DONFL appeared in blue-filtered photographs in 43% of ERM cases after PPV with ILM peeling [21]. Park et al. reported a DONFL appearance after PPV in 10% of ERM cases as determined by fundus photos and OCT B scans [28]. The incidence of DONFL may depend on the detecting methods. Alkabes et al. reported a 100% detection rate using en face OCT scans after PPV with ILM peeling for macular hole [29]. In the present study, a DONFL appearance was found in only 12% of cases even when using en face OCT scans at comparable time points for DONFL evaluation to previous studies [29,30,31,32]. Several studies have demonstrated that a DONFL appearance did not alter retinal sensitivity, as measured by microperimetry or 10–2 VF testing after PPV with ILM peeling for macular hole [30, 31]. However, Nukada et al. showed significant differences in retinal sensitivities between the area on the DONFL and areas away from it [32]. Although we found that postoperative changes in MD and TD in the inferior cecocentral sector were significantly worse in eyes with DONFL than in eyes without in the control group, the differences were small. Therefore, the negative effects of DONFL on postoperative VFs may be clinically insignificant.
We utilized the ERM staging system developed by Govetto et al. based on the existence of ectopic inner foveal layers to investigate the relationship between the severity of ERM and VF deterioration [20]. They demonstrated that the stage progressed over time, and that advanced ERM stages were associated with poor visual acuity preoperatively as well as postoperatively [33]. In our study, the existence of ectopic inner layers (i.e., stages 3 or 4) was not a significant factor for postoperative VF changes in either group in the multivariate analysis. However, more cases with stage 4 ERM may be needed to confirm our findings.
As for the structure–function relationship per sector, glaucomatous eyes showed more evident relationship postoperatively than preoperatively especially in the outer arcuate sectors. This implies that ERM-induced retinal thickening masked the glaucomatous structure–function relationship. Although we did not find clear structure–function relationship in the control group, a recent report showed postoperative GCC thickness was significantly correlated with 10–2 TD in most of Early Treatment of Diabetic Retinopathy Study (ETDRS) sectors in nonglaucomatous eyes [34]. They showed significant TD decrease and abnormal GCC thinning in some ETDRS sectors in eyes treated with indocyanine green for ILM staining (60% of cases) which may have adverse effects on retinal sensitivity [25]. In contrast, we did not use indocyanine green at all, and experienced no severe TD deterioration in any patients in the control group. The use of indocyanine green may be a reason for the controversial results between two studies.
This study has several limitations. The sample size was small, and the results were based on surgeries by a single experienced surgeon performed in Japanese patients with or without glaucoma, mainly normal-tension glaucoma. All glaucomatous eyes already had a scotoma in 10–2 VFs meeting the criteria proposed by Traynis et al. [9]. In their study, a cluster of three contiguous abnormal points (5%, 5%, and 1% or 5%, 2%, and 2%) within a hemifield on either TD or pattern deviation plots was regarded abnormal. Therefore, the issue whether intact 10–2 VFs in glaucomatous eyes deteriorate postoperatively more than those in nonglaucomatous eyes remains to be clarified.
BBG was not available in glaucoma patients who were enrolled in the early study phase, while it was used in all nonglaucomatous cases. Given that BBG usage had no influence on any results in the glaucoma group, the entry timing and BBG usage were not major factors for postoperative VF changes. Although there is no general consensus regarding 10–2 VF sectorization, three sector models for glaucomatous VF defects have been reported; ten sectors derived from the interpoint correlation of cross-sectional TD values [14], seven sectors based on pointwise VF progression at similar frequency and slopes [15], and four sectors developed from the structure–unction map in the macula taking into consideration RGC displacement [16]. Here, we used six vertically symmetrical sectors to facilitate comparisons between the superior and inferior hemifields in contrast to the vertically asymmetrical sectors used in the previous three reports, which may affect sectorwise results. Nonetheless, our sectorwise analysis successfully identified the topographical characteristics of postoperative changes in the 10–2 VFs.
The postoperative TD improvement in some sectors and preoperative worse VF sensitivity as a significant factor for postoperative VF improvement in the control group may be explained by the learning effects which may have masked postoperative VF deterioration, although all participants had at least two 24–2 VF testing prior to 10–2 VF testing which was repeated if unreliable or obviously abnormal. Castro et al. reported both MD and PSD significantly improved in the second session than in the first session in 24–2 VFs of healthy subjects with no perimetry experience [35]. However, in our control group, 10–2 PSD did not improve in the postoperative sessions. Furthermore, cataract surgery did not have any influence on VF changes. Thus, postoperative VF improvement in the control group may indicate a beneficial effect of ERM removal. In this regard, eyes with ERM stages 3 and 4, but not stages 1 and 2, showed significant improvement in 10–2 MD postoperatively in the univariate analysis (p = 0.008), indicating the presence of ERM-induced VF impairment in eyes with advanced ERM.
Finally, the interval between surgery and VF sessions was not a significant factor for VF changes during the 12-month postoperative period. We set the period to examine the direct effects of PPV on VFs. Within a shorter period, three VF sessions may be difficult to perform, while VF changes in a longer period may be more likely to be affected by glaucoma progression. However, a longer study period with more postoperative VF sessions is necessary to elucidate whether PPV with ILM peeling for ERM may accelerate glaucoma progression or not [36].
In conclusion, the central VF within 10 degrees, especially in the outer arcuate sectors, deteriorated after PPV with ILM peeling for ERM in eyes with glaucoma, while it remained stable in eyes without glaucoma. Eyes with advanced glaucoma, having a thinner GCC and worse VF, may be at greater risk for postoperative central VF deterioration.
Summary
What was known before
-
Pars plana vitrectomy (PPV) may cause visual field (VF) loss due to various reasons.
-
PPV with internal limiting membrane (ILM) peeling for epiretinal membrane (ERM) may result in VF deterioration in patients with coexisting glaucoma.
What this study adds
-
The central VF within 10 degrees, especially in the outer arcuate sectors, deteriorated after PPV with ILM peeling for ERM in eyes with glaucoma, while it remained stable in eyes without glaucoma.
-
Given that both worse VF and thinner ganglion cell complex were the predictors of postoperative central VF worsening, eyes with advanced glaucoma are at higher risk of postoperative central VF deterioration.
References
Kinoshita T, Imaizumi H, Okushiba U, Miyamoto H, Ogino T, Mitamura Y. Time course of changes in metamorphopsia, visual acuity, and OCT parameters after successful epiretinal membrane surgery. Invest Ophthalmol Vis Sci. 2012;53:3592–7.
Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Time course of changes in aniseikonia and foveal microstructure after vitrectomy for epiretinal membrane. Ophthalmology. 2014;121:2255–60.
Takabatake M, Higashide T, Udagawa S, Sugiyama K. Postoperative changes and prognostic factors of visual acuity, metamorphopsia, and aniseikonia after vitrectomy for epiretinal membrane. Retina. 2018;38:2118–27.
Uemura A, Kanda S, Sakamoto Y, Kita H. Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine green–assisted internal limiting membrane peeling. Am J Ophthalmol. 2003;136:252–7.
Ripandelli G, Scarinci F, Piaggi P, Guidi G, Pileri M, Cupo G, et al. Macular pucker: to peel or not to peel the internal limiting membrane? A microperimetric response. Retina. 2015;35:498–507.
Azuma K, Ueta T, Eguchi S, Aihara M. Effects of internal limiting membrane peeling combined with removal of idiopathic epiretinal membrane: a systematic review of literature and meta-analysis. Retina. 2017;37:1813–9.
Asrani S, Essaid L, Alder BD, Santiago-Turla C. Artifacts in spectral-domain optical coherence tomography measurements in glaucoma. JAMA Ophthalmol. 2014;132:396–402.
Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Traynis I, De Moraes CG, Raza AS, Liebmann JM, Ritch R, Hood DC. Prevalence and nature of early glaucomatous defects in the central 10° of the visual field. JAMA Ophthalmol. 2014;132:291–7.
Murata H, Hirasawa H, Aoyama Y, Sugisaki K, Araie M, Mayama C, et al. Identifying areas of the visual field important for quality of life in patients with glaucoma. PLoS ONE. 2013;8:1–7.
Moroi SE, Gottfredsdottir MS, Van Heck T, Musch DC, Johnson MW. Visual field results after vitreous surgery in a case series of patients with open-angle glaucoma. Ophthalmic Surg Lasers. 2000;31:380–6.
Tsuchiya S, Higashide T, Sugiyama K. Visual field changes after vitrectomy with internal limiting membrane peeling for epiretinal membrane or macular hole in glaucomatous eyes. PLoS ONE. 2017;12:e0177526.
Heijl A, Lindgren G, Olsson J. The effect of perimetric experience in normal subjects. Arch Ophthalmol. 1989;107:81–6.
Koseki N, Araie M, Yamagami J, Suzuki Y. Sectorization of central 10-deg visual field in open-angle glaucoma - An approach for its brief evaluation. Graefes Arch Clin Exp Ophthalmol. 1995;233:621–6.
De Moraes CG, Song C, Liebmann JM, Simonson JL, Furlanetto RL, Ritch R. Defining 10-2 visual field progression criteria: exploratory and confirmatory factor analysis using pointwise linear regression. Ophthalmology. 2014;121:741–9.
Hood DC, Raza AS, de Moraes CGV, Liebmann JM, Ritch R. Glaucomatous damage of the macula. Prog Retin Eye Res. 2013;32:1–21.
Hood DC, Anderson SC, Wall M, Kardon RH. Structure versus function in glaucoma: an application of a linear model. Invest Ophthalmol Vis Sci. 2007;48:3662–8.
Drasdo N, Millican CL, Katholi CR, Curcio CA. The length of Henle fibers in the human retina and a model of ganglion receptive field density in the visual field. Vis Res. 2007;47:2901–11.
Ohkubo S, Higashide T, Udagawa S, Sugiyama K, Hangai M, Yoshimura N, et al. Focal relationship between structure and function within the central 10 degrees in glaucoma. Invest Ophthalmol Vis Sci. 2014;55:5269–77.
Govetto A, Lalane RA, Sarraf D, Figueroa MS, Hubschman JP. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017;175:99–113.
Tadayoni R, Paques M, Massin P, Mouki-Benani S, Mikol J, Gaudric A. Dissociated optic nerve fiber layer appearance of the fundus after idiopathic epiretinal membrane removal. Ophthalmology. 2001;108:2279–83.
Araie M, Iwase A, Sugiyama K, Nakazawa T, Tomita G, Hangai M, et al. Determinants and characteristics of bruch’s membrane opening and bruch’s membrane opening–minimum rim width in a normal Japanese population. Invest Ophthalmol Vis Sci. 2017;58:4106–13.
Haritoglou C, Ehrt O, Gass CA, Kristin N, Kampik A. Paracentral scotomata: a new finding after vitrectomy for idiopathic macular hole. Br J Ophthalmol. 2001;85:231–3.
Ooto S, Hangai M, Tomidokoro A, Saito H, Araie M, Otani T, et al. Effects of age, sex, and axial length on the three-dimensional profile of normal macular layer structures. Invest Ophthalmol Vis Sci. 2011;52:8769–79.
Baba T, Hagiwara A, Sato E, Arai M, Oshitari T, Yamamoto S. Comparison of vitrectomy with brilliant blue G or indocyanine green on retinal microstructure and function of eyes with macular hole. Ophthalmology. 2012;119:2609–15.
Tari SR, Vidne-Hay O, Greenstein VC, Barile GR, Hood DC, Chang S. Functional and structural measurements for the assessment of internal limiting membrane peeling in idiopathic macular pucker. Retina. 2007;27:567–72.
Shimada H, Nakashizuka H, Hattori T, Mori R, Mizutani Y, Yuzawa M. Double staining with brilliant blue G and double peeling for epiretinal membranes. Ophthalmology. 2009;116:1370–6.
Park SUNHO, Kim YJ, Lee SJIN. Incidence of and risk factors for dissociated optic nerve fiber layer after epiretinal membrane surgery. Retina. 2013;36:1–5.
Alkabes M, Salinas C, Vitale L, Burés-Jelstrup A, Nucci P, Mateo C. En face optical coherence tomography of inner retinal defects after internal limiting membrane peeling for idiopathic macular hole. Invest Ophthalmol Vis Sci. 2011;52:8349–55.
Mitamura Y, Ohtsuka K. Relationship of dissociated optic nerve fiber layer appearance to internal limiting membrane peeling. Ophthalmology. 2005;112:1766–70.
Ito Y, Terasaki H, Takahashi A, Yamakoshi T, Kondo M, Nakamura M. Dissociated optic nerve fiber layer appearance after internal limiting membrane peeling for idiopathic macular holes. Ophthalmology. 2005;112:1415–20.
Nukada K, Hangai M, Ooto S, Yoshikawa M, Yoshimura N Jr, BH, et al. Tomographic features of macula after successful macular hole surgery. Invest Ophthalmol Vis Sci. 2013;54:2417–28.
Govetto A, Virgili G, Rodriguez FJ, Figueroa MS, Sarraf D, Hubschman JP. Functional and anatomical significance of the ectopic inner foveal layers in eyes with idiopathic epiretinal membranes: surgical results at 12 months. Retina. 2019;39:347–57.
Terashima H, Okamoto F, Hasebe H, Matsuoka N, Fukuchi T. Vitrectomy for epiretinal membranes: ganglion cell features correlate with visual function outcomes. Ophthalmol Retin. 2018;2:1152–62.
Castro DPE, Kawase J, Melo LAS. Learning effect of standard automated perimetry in healthy individuals. Arq Bras Oftalmol. 2008;71:523–8.
De Moraes CG, Liebmann JM, Levin LA. Detection and measurement of clinically meaningful visual field progression in clinical trials for glaucoma. Prog Retin Eye Res. 2017;56:107–47.
Acknowledgements
The authors thank Shiroaki Shirato M.D. for his helpful advice on the 10-2 VF sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsuchiya, S., Higashide, T., Udagawa, S. et al. Glaucoma-related central visual field deterioration after vitrectomy for epiretinal membrane: topographic characteristics and risk factors. Eye 35, 919–928 (2021). https://doi.org/10.1038/s41433-020-0996-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0996-8
This article is cited by
-
Structure–function analysis for macular surgery in patients with coexisting glaucoma
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Evaluation of postoperative visual function based on the preoperative inner layer structure in the epiretinal membrane
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)