Abstract
EEC staff were provided with rapidly changing personal PPE guidance by Public Health England (PHE) with specific subspecialty advice from the British Emergency Eye Care Society (BEECS) and the Royal College of Ophthalmologists (RCOphth) UK during the COVID19 pandemic. BEECS undertook a baseline survey of its members after the initial response from the RCOphth 16/3/20 mirroring Public Health England (PHE) advice and a follow- up survey after the guidance was updated on 9/4/20. A combined total of 84 responses were received. Improvements after RCOphth changes between the two surveys from hospital respondents showed increases in temperature screening (13%), scrub use (34%), use of aprons (31%), masks (4%), eye protection (35%), gloves (25%) and slit lamp guard (1%). Our findings demonstrate a positive and significant adaptation of PPE in response to change in guidance published by PHE, RCOphth and BEECS between 16/3/20 and 11/4/20. The COVID19 pandemic has rapidly taken over the normal activity of Ophthalmic departments creating unprecedented challenges. Following initial confusion and vulnerability expressed by EEC professionals to PPE guidance, most Trusts appear to have adapted and are doing similar things. The response has been swift and effective as a result of good team work and early advice from BEECS and the RCOphth. On the whole, management teams are listening.
Similar content being viewed by others
Introduction
The novel coronavirus disease 2019 (COVID19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was declared a global pandemic by the World Health Organisation on the 11th of March 2020 [1]. The Royal College of Ophthalmologists response for UK ophthalmic departments was to reduce activity and provide hospital services for sight-threatening emergencies due to the threat of fatal COVID19 complications among the UK population [2]. The college of optometry, similarly, provided guidance for practices to stop routine GOS services and only provide emergency eye services by accredited MECS/MECS type practices [3].
Emerging publications from China, where the disease was first reported, highlighted the increased risk of transmission of SARS-CoV-2 for health care workers working in close contact with infected patients [4]. Reports found SARS-CoV-2 present on ocular surfaces and a cause of conjunctivitis of varying incidence [5,6,7]. Emergency eye care (EEC) professionals come into close contact with patient’s ocular surfaces while managing ocular emergencies in both community and hospital settings, increasing their risk of acquiring COVID19 [5,6,7]. Personal protective equipment (PPE) are (is) used to reduce the risk of health care workers exposure to potentially infectious droplets while managing a patient infected with SARS-CoV-2 [8].
EEC staff were provided with rapidly changing personal PPE guidance by Public Health England (PHE) with specific subspecialty advice from the British Emergency Eye Care Society (BEECS) and the Royal College of Ophthalmologists (RCOphth) UK.
Aim of study
The aim of this study was to survey EEC professionals in primary and secondary care about (and evaluate) the provision and response of departments to information given with regard to PPE during the COVID19 pandemic period.
Methods
BEECS undertook a baseline survey of its members after the initial response from the RCOphth 16/3/20 mirroring Public Health England (PHE) advice and a follow-up survey after the guidance was updated on 9/4/20. See Table 1 for time line of events and RCOphth PPE guidance and Table 2 for survey questions.
Each survey was completed by BEECS members delivering EEC services in both primary and secondary care during the COVID19 pandemic. A total of 50 responses were received for the baseline survey and 34 for the follow-up survey.
Results
A combined total of 84 responses were received for the surveys sent.
Hospital respondents
Hospital respondents totalled 29 for survey 1 (20% stand alone eye unit, 52% University Hospital/Acute Trust and 27% District General Hospital) and 32 for survey 2 (19% stand alone eye unit, 44% University Hospital/Acute Trust and 34% District General Hospital).
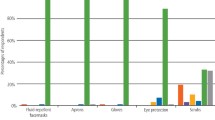
Figures 1, 2 demonstrate a change between the surveys for temperature screening with an increase of 13% noted and an increase of 34% in the use of scrubs to examine low- and high-risk COVID19 patients. Other changes noted was an increase in the use of aprons (31%), masks (4%), eye protection (35%), gloves (25%) and slit lamp guard (1%) (Table 3).
Hospital management were seen to be more receptive to the demands of EEC professionals after the 9/4/20 RCOphth guidelines were updated, an increase of 21% and 40% more were providing PPE advice. An improvement in the supply of PPE and relaxation on EEC professionals wearing personally acquired PPE by 11% and 11% respectively, for the same time period. See Table 4.
Optometrists
Twenty-one optometrists replied to survey 1–76% of which are affiliated to MECS/MECS type services.
See Table 3 for their PPE use.
Discussion
Our findings demonstrate a positive and significant adaptation of PPE in response to change in guidance published by PHE, RCOphth and BEECS between 16/3/20 and 11/4/20.
Initial responses for health care workers during the COVID19 pandemic from PHE meant Ophthalmology was not on Trust radars as a high-risk specialty leading to Ophthalmologists and AHP feeling vulnerable to exposure and objection to self provided protection. Early response by the RCOphth and BEECS included advice to install substantial guards to slit lamps, thereby creating a physical barrier to the transfer of aerosol droplets during close ocular examination [2]. Ninety-three percent of hospital EEC professions initially surveyed had slit lamp guards; however, not all units were compliant. With the initial guidance, many were forced to use temporary DIY homemade guards while awaiting robust options.
Prior to the change in PPE advice on 9/4/20, 17% of individuals experienced objection or threat of disciplinary action if they were seen to wear their own personally acquired PPE items. This reduced to 6% in the second survey, which may reflect the change in PHE recommendations and provision of additional PPE by the Government to the employers. There was an increase from 47% to 78% in respondents that were satisfied with the information they were given about PPE and from 50% to 60% in those that felt management listened to them about their views on PPE provision.
Importantly after the 9/4/20 update, there was an increase in satisfaction with information about PPE and more felt their hospital management took into account the clinicians’ views and listened to them about their views on PPE provision.
A reduction in the number of responses to our follow-up survey from the primary care ophthalmic practitioners (MECS and non-MECS practices) might reflect that many had to close their doors due to the lack of PPE, which was not prioritized in this sector. Those currently operating are providing telephone consultations and face to face emergency consultations where PPE has been provided.
Conclusion
The COVID19 pandemic has rapidly taken over the normal activity of Ophthalmic departments creating unprecedented challenges. Following initial confusion and vulnerability expressed by EEC professionals to PPE guidance, most Trusts appear to have adapted and are doing similar things. The response has been swift and effective as a result of good team work and early advice from BEECS and the RCOphth. Learning from other affected countries has been paramount when planning and adjusting to this new challenging situation. On the whole, management teams are listening and hopefully in the very near future our Primary care optometry colleagues will be provided with similar levels of PPE for continued collaboration in the management of ocular emergencies during this COVID19 global pandemic.
Summary
What was known before
Very little was known before as this is a novel infection. No health planning for this type of pandemic.
What this study adds
A positive and significant adaptation of PPE in response to change in guidance. Most Trusts appear to have adapted and are doing similar things.
References
WHO. www.WHO.int. Accessed April 2020.
Royal College of Ophthalmologists. www.rcophth.ac.uk. Accessed March 2020.
www.college-optometrists.org. Accessed April 2020.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–42.
Zhou Y, Zeng Y, Tong Y, Chen C. Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva. medRixiv. 2020. https://www.medrxiv.org/content/10.1101/2020.02.11.20021956v1.
Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020. https://doi.org/10.1001/jamaophthalmol.2020.1291.
Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020. https://doi.org/10.1016/s0140-6736(20)30313-5.
Li JO, Lam DSC, Chen Y, et al. Novel Coronavirus Disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104:297–8.
Acknowledgements
We acknowledge BEECS committee members for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shirodkar, Al., De Silva, I., Verma, S. et al. Personal Protective Equipment (PPE) use among emergency eye care professionals in the UK during the COVID19 pandemic. Eye 34, 1224–1228 (2020). https://doi.org/10.1038/s41433-020-0970-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0970-5