Abstract
Background
Naevomelanocytic lesions comprise an increasing workload in ophthalmic secondary care and, although largely benign, carry high risk of mortality in case of malignant transformation. Previous studies highlight the theoretical strength of virtual models in monitoring such lesions and the role of allied health professionals (AHPs). We aim to describe and validate a “real-world” functional clinical model utilising these particular resources.
Methods
New and existing follow-up patients from November 2016 to June 2019 with melanocytic lesions of the uveal tract and conjunctiva were directed into an optometrist-led, consultant-supported, clinic. Diagnostic tests included colour photography, autofluorescence, enhanced-depth imaging and ultrasound biomicroscopy. New patients were examined face-to-face initially, then virtually on subsequent visits. Suspicious lesions were referred to the consultant, with tertiary oncology referrals made as necessary. Clinical concordance between optometrist and consultant, patient satisfaction and outcomes of second opinion requests were audited.
Results
Eight hundred and twenty-five patient episodes were encountered: 419 new and 406 follow-up. Between July 1st and August 31st 2018, 72 cases were audited. There was 98.6% concordance between AHP and consultant for diagnosis and management. Referral for consultant second opinion was requested in 18(2%) clinical encounters, with 4(0.5%) referred on to the oncology centre, of which 3 received treatment. Of 65 patients responding to a patient satisfaction survey, 100% were satisfied with their experience and 95% were happy to continue monitoring by the AHP.
Conclusion
With robust training and assessment, AHP-led service models are a highly efficient in busy units, without compromising patient safety.
Similar content being viewed by others
Introduction
Ocular naevomelanocytic lesions are present in over 6% of the Caucasian population [1], with uveal melanomas comprising over 98% of malignancies, and the remaining 2% are of adnexal and conjunctival origin [2]. Of uveal malignancies, 90% of cases are choroidal melanomas, with 10% attributed to iris and ciliary body lesions [3, 4]. Current literature suggests rates of transformation from naevus to melanoma can be as high as 0.2% with greater than 50% mortality within 10 years for those affected, although early diagnosis and initiation of treatment can improve survival [5,6,7,8].
Naevomelanocytic lesions are increasingly referred into hospital eye services due to improvements in imaging modalities used (e.g. wide-field, non-mydriatic fundus cameras), increasingly comprehensive assessments carried out in the community and awareness of risks associated with delayed referral and treatment [9, 10]. However, secondary-care resources in the UK are also increasingly stretched for providing expert diagnosis, monitoring and recognising emerging features of malignancy [4, 11].
This combination of increased workload and potential for extreme morbidity necessitates a robust system which utilises clinician time effectively and reproducibly monitors salient parameters. The role of allied healthcare professionals (AHP) in clinical work is well established in ophthalmology, with published competency frameworks by the Royal College of Ophthalmologists (RCOphth) to support development of clinical skills in non-medical members of the ophthalmic multidisciplinary team [12]. The virtual review model is also increasingly used to monitor large cohorts of stable patients, particularly in the fields of medical retina and glaucoma [13, 14].
The success of a nurse-delivered, clinician-supervised review clinic for follow-up patients at the Liverpool Ocular Oncology Centre (LOOC) has previously been demonstrated [15]. More recently, Balaskas et al. proposed a virtual service model from a pilot study for managing naevomelanocytic lesions [16]. The authors retrospectively assessed concordance between decisions made by ophthalmologists in an outpatient setting and masked remote virtual review by both ophthalmologists and non-medical graders, showing good concordance between all groups, thereby laying the foundations for a functional clinic which utilises the benefits of such a model.
In this paper, we present real-world outcomes of our novel optometrist-led model for the assessment and monitoring of naevomelanocytic lesions which, at the time of writing and to our knowledge, is a nationally unique endeavour. Since its conception in November 2016, we present data on patient flow through the clinic and consultant involvement. In addition, we present outcomes from the first service audit.
Materials and methods
Patients
From November 2016 to date, all new referrals for ocular melanocytic lesions (conjunctival and uveal) from the community have been triaged into the AHP clinic pathway. Patients already under surveillance by other consultants within the same department were streamlined similarly, including those previously treated at LOOC for ocular melanoma and requiring lifelong monitoring.
Healthcare professionals
The lead AHP is an optometrist with 12 years’ experience working independently in both the virtual and outpatient glaucoma clinic within the department. This demonstrates a high level of competency identifying pathology of both the anterior and posterior segments, and interpretation of commonly used ophthalmic diagnostics. Specific training for assessing and monitoring melanocytic lesions was achieved through didactic lectures given by the supervising consultant with comprehensive discussions around images taken with all modalities used in the clinic. This included images with features of malignant transformation, melanomas prior to treatment and lesions post-treatment. Clinical training commenced with sessions of clinical shadowing with collaborative virtual review, followed by side-by-side supported clinical sessions where all face-to-face and virtual encounters were first carried out by the AHP and then reviewed by the consultant, with concurrent troubleshooting as needed until independence was achieved.
The supervising consultant (NK) primarily specialises in medical retina with a special interest in ocular oncology based on a clinical fellowship at the LOOC, where she was involved in the development of the prior mentioned nurse-led oncology clinic.
Imaging support, vital for more skill-dependant imaging modalities such as ultrasound biomicroscopy (UBM), is provided by the lead clinical photographer. Advanced ultrasound biomicroscopy skills were achieved through a hands-on national training course recognised by the RCOphth.
Equipment
At each visit, visual acuity is measured using Snellen acuity charts and intraocular pressure checked using the iCare rebound tonometer (TA01i, Revenio Group Corporation, Finland). Anterior segment and fundal photographs are taken using the VX-20 Retinal Camera (Kowa Company Ltd, Japan). Enhanced-depth imaging optical coherence tomography (EDI-OCT) and autofluorescence images are obtained using Spectralis HRA + OCT (Heidelberg Engineering Ltd, UK). UBM is performed using Eyecubed (Ellex Ltd, Australia). Goniophotos are taken using the CSO slitlamp SL990 (Construzione Strumenti Oftalmici, Italy). Images are viewed using a networked desktop and clinical notes were recorded on electronic patient records (EPR) via Medisoft (Medisoft Ltd, UK).
Clinic model
The clinic runs once weekly, with eight patients per session and a combination of both face-to-face and virtual assessments depending on clinical need. New patients have a face-to-face consultation with the AHP, with dilated fundoscopy, colour anterior segment/fundal photographs, EDI-OCT and autofluorescence of retinal lesions as baseline [17, 18]. UBM is performed on lesions appearing raised or if the whole lesion cannot be visualised [19]. Lesions involving the angle may require goniophotos. The necessary investigations are repeated at all subsequent visits, including documentation of visual acuity and development of symptoms.
Patients are migrated to virtual review directly after initial assessment if investigations can be performed satisfactorily and no suspicion of malignancy such as sub-retinal fluid, presence of pigment, thickness and ultrasound reflectivity [11]. When images cannot be adequately obtained (e.g. difficulty positioning, lesion outside of imaging field, etc), a face-to-face consultation is booked with the AHP. Virtual review involves the patient attending the department for imaging with documentation of acuity, intraocular pressure and symptomatic change. This information is reviewed within 1 week, a follow-up plan is made, and the patient is notified by post. Virtual review patients are also given a patient information leaflet explaining which tests will be performed, why they are being imaged, who will be reviewing their images, when they will receive their results and that necessary arrangements will be made if changes are noted. For face-to-face consultations, imaging and patient review occur during the hospital visit with follow-up plans discussed directly with the patient.
The first follow-up appointment for naevi that are diagnosed with confidence and no suspicious features is scheduled at 6 months, then annually thereafter. If a lesion remains unchanged for 5 years, the patient is discharged back to the care of their community optometrist [20]. At any stage, there is an option to refer to the consultant-supported aspect of the service for a second opinion, which involves a virtual review within 24 h and immediate referral to LOOC if indicated. Alternatively, if suspicious features are seen on first consultation, the patient is referred to the consultant where they may be watched closely in the consultant clinic, referred back for monitoring in the AHP pathway or referred to LOOC. Figure 1 shows patient flow through the service.
All patients enter the AHP-led arm (left side) of the pathway with a face-to-face assessment in the first instance, with subsequent follow-up in the same arm if suitable. Patients are referred into the concultant-led arm (right side) of the pathway if there are suspicious features which may require intervention. Patients can be migrated from one side to the other depending on need.
Quality assurance
Quality assurance is ensured both continuously and during designated audit periods. Continuous monitoring is achieved through blinded review by the consultant of around 10–15% of all patients seen in the AHP-led clinic through review of the EPR and respective images/scans. One session every 2 months is reviewed fully, and a random selection of records are reviewed on an ad-hoc basis.
Auditing of the service, in line with clinical governance requirements of the Trust, is also carried out every 2 years. During audit periods, all clinical encounters undergo blinded review to evaluate corroboration of diagnoses and outcomes, and these same patients are requested to fill in a patient satisfaction survey.
Results
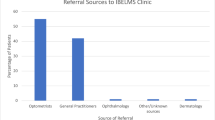
From November 2016 to June 2019, there were 825 clinical encounters totally, both virtual and face-to-face, of which 419 were new (including totally new referrals into the department and transfer of care from existing patient from other consultants) and 406 were follow-ups.
Audit of service
Between July and August 2018, 72 patient encounters were audited: 24 new and 48 follow-ups. All new referrals were seen face-to-face. Of the follow-ups, 47 (97.9%) were reviewed via the virtual pathway and 1 (2.1%) was seen face-to-face.
Correlation between AHP and consultant
There was 98.6% (71/72) agreement between AHP and consultant decisions regarding diagnosis and follow-up. One patient was diagnosed by the AHP as having an iris cyst based on clinical and anterior segment OCT findings (UBM was not available for examination) and, as no features of burgeoning malignancy were noted, the decision to discharge was made. Upon virtual review by the consultant, there was the differential diagnosis of naevus, hence 4 month follow-up was recommended to carry out UBM and clarify the diagnosis. No patients were deemed to require face-to-face follow-up. Table 1 summarises correlation between AHP and consultant.
Patient satisfaction
65/72 (90.3%) responded to an anonymised paper questionnaire presented either during consultation or whilst imaging was procured for the virtual clinic. Of these patients, 25 (38.5%) were new patients having a face-to-face consultation, 1 (1.5%) was being followed up face-to-face and 39 (60%) were virtual reviews.
A summary of patient responses is as follows:
-
26/26 (100%) patients surveyed following face-to-face consultation were happy with their clinical experience, although 1 patient reported a preference for consultation with a doctor.
-
39/39 (100%) were satisfied with their virtual review experience.
-
62/65 (95%) of patients were happy to continue being monitored by an appropriately trained AHP.
Referral for second opinion
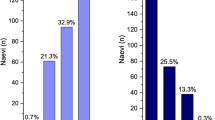
There have been 18 referrals for second opinion from the supporting consultant from November 2016 to June 2019, at a rate of ~7 per year. Four patients were eventually referred to LOOC.
All second opinion requests are emailed directly to the consultant allowing review of the EPR and relevant imaging, usually within 1–3 days, allowing urgent appointments to be made as necessary. The choroidal and ciliary body melanoma were referred directly to the consultant from their first assessment in the AHP clinic, with immediate referral to LOOC following consultant review. The iris melanoma had been monitored for several years as an indeterminate lesion and tertiary referral was instigated when malignant change became apparent. The choroidal osteoma had also been monitored long-term, but was referred to LOOC upon sudden development of sub-retinal fluid and reducing acuity.
Figure 2 describes the outcomes of the cohort of patients referred to the supporting consultant for second opinion.
Discussion
Our report is the first to detail real-world outcomes of an in-house model of an AHP-led service for ocular melanocytic lesions. Virtual and AHP supported models are developed to streamline workload, allowing stable cases to remain under surveillance and progressive cases to be directed to the supervising ophthalmologist. As mentioned above, a nurse-delivered ocular oncology follow-up clinic has been successfully utilised at LOOC [15], where reviews of suspicious and post-treatment lesions were carried out by a trained nurse, alternating with reviews by a doctor. We expanded further on this with all new referrals and follow-ups (i.e. diagnosis and subsequent monitoring) being carried out by the AHP unless there is evidence of change. Our clinic aims to give more clinical responsibility to our AHP, encouraging independent working with the option of consultant input as required. It follows, therefore, that the success of a clinic model such as ours depends on a level of confidence and experience on the part of the AHP, including a willingness to continue developing clinical skills, so that clinical decision-making does not become overwhelming. Of 825 patient encounters between November 2016 and June 2019, only 18 (2%) were referred for consultant opinion, of which 4 (0.5%) were referred to LOOC, showing that this clinic significantly reduces burden on the consultant clinic, especially as the majority of cases are stable and benign.
Work done previously by Balaskas et al. has shown good concordance between remote virtual reviews carried out by trained graders, remote virtual reviews by ophthalmologists and clinical assessment in an outpatient clinic by ophthalmologists (the gold standard) [16]. The results of our first nationally set-up AHP-led model shows that these findings can be replicated in in-house real-world settings and, furthermore, shows that combining virtual assessments with face-to-face outpatient assessments creates a complete patient pathway. Clinical agreement between our AHP and consultant is reported at 98.6% over the audit period, supporting the safety profile of the service. The inbuilt process checking correlation between clinical decisions in the form of regular blinded reviews of patient notes and biennial service evaluation audits, as described previously, also maintains safety parameters. In addition, our results show that any abnormal features which were detected were immediately highlighted to the consultant via an urgent email, with urgent outpatient review arranged as necessary. All cases referred to LOOC were sent without delay demonstrating that the additional step of AHP to consultant referral prior to tertiary referral does not result in negative outcomes for the patient. Patients themselves report overall satisfaction with the service through anonymised questionnaires during the audit period.
It is estimated that 320 patients annually, who would previously have been reviewed in the consultant clinic, are now seen virtually and in outpatients by the AHP, allowing consultant clinical time to be utilised more effectively. The current service model is able to manage the rate of new referrals and follow-ups, so it would be of interest to reassess the service as patient cohort and demand for appointments increases.
The next step in improved utility of clinical time and efficiency comes in the form of artificial intelligence. Retinal disease has in particular benefitted from research into incorporation of machine and deep learning models into the diagnostic process. Development of such models are imminently possible when diagnosis relies on pattern recognition, particularly based on imaging datasets. Thus, monitoring of lesions where images can reliably be procured could feasibly be carried out using artificial intelligence [21].
To conclude, at a time where demands on ophthalmic services are only increasing due to a changing demographic and increasing innovation, the development of processes to improve efficiency whilst maintaining patient safety is imperative. Our outcomes from this service are encouraging thus far and shows scope for expansion into other high-volume areas of ophthalmic service provision.
Summary
What was known before
-
Pilot studies that allied health professionals could potentially have a role in monitoring and identifying suspicious features of ocular melanocytic lesions.
What this study adds
-
This study reports on a novel clinic structure currently in practice, utilising both allied health professionals and a virtual review model.
References
Sumich P, Mitchell P, Wang JJ. Choroidal nevi in a white population- the blue mountains eye study. Arch Ophthalmol. 1998;116:645–50.
Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. cancer: Interdisciplinary International. J Am Cancer Soc. 1998;83:1664–78.
Egan KM, Seddon JM, Glynn RJ, Gragoudas ES, Albert DM. Epidemiologic aspects of uveal melanoma. Surv Ophthalmol. 1988;32:239–51.
Damato BE, Coupland SE. Ocular melanoma. Saudi J Ophthalmol. 2012;26:137–44.
Singh AD, Kalyani P, Topham A. Estimating the risk of malignant transformation of a choroidal nevus. Ophthalmology. 2005;112:1784–9.
Chien JL, Sioufi K, Surakiatchanukul T, Shields JA, Shields CL. Choroidal nevus: a review of prevalence, features, genetics, risks, and outcomes. Curr Opin Ophthalmol. 2017;28:228–37.
Pulido J. Choroidal nevus transformation into melanoma. Evidence-based. Ophthalmology. 2010;11:108–9.
Kaliki S, Shields CL, Shields JA. Uveal melanoma: estimating prognosis. Indian J Ophthalmol. 2015;63:93.
Brown K, Sewell JM, Trempe C, Peto T, Travison TG. Comparison of image-assisted versus traditional fundus examination. Eye Brain. 2013;5:1.
Damato EM, Damato BE. Detection and time to treatment of uveal melanoma in the United Kingdom: an evaluation of 2384 patients. Ophthalmology. 2012;119:1582–9.
Shields CL, Demirci H, Materin MA, Marr BP, Mashayekhi A, Shields JA. Clinical factors in the identification of small choroidal melanoma. Can J Ophthalmol. 2004;39:351–7.
The Royal College of Ophthalmologists. The common clinical competency framework for non-medical ophthalmic healthcare professionals in secondary care association of health professions in ophthalmology. 2016. https://www.rcophth.ac.uk/wp-content/uploads/2017/01/CCCF-HCPs.pdf. Accessed July 2019.
Kortuem K, Fasler K, Charnley A, Khambati H, Fasolo S, Katz M, et al. Implementation of medical retina virtual clinics in a tertiary eye care referral centre. Br J Ophthalmoly. 2018;102:1391–5.
Clarke J, Puertas R, Kotecha A, Foster PJ, Barton K. Virtual clinics in glaucoma care: face-to-face versus remote decision-making. Br J Ophthalmol. 2017;101:892–5.
Sandinha T, Hebbar G, Kenawy N, Hope-Stone L, Damato B. A nurse-led ocular oncology clinic in Liverpool: r of a 6-month trial. Eye. 2012;26:937–43.
Balaskas K, Gray J, Blows P, Rajai A, Flaye D, Peto T, et al. Management of choroidal naevomelanocytic lesions: feasibility and safety of a virtual clinic model. Br J Ophthalmoly. 2016;100:665–70.
Shields CL, Kaliki S, Rojanaporn D, Ferenczy SR, Shields JA. Enhanced depth imaging optical coherence tomography of small choroidal melanoma. Arch Ophthalmol. 2016;130:850–6.
Albertus DL, Schachar IH, Zahid S, Elner VM, Demirci H, Jayasundera T. Autofluorescence quantification of benign and malignant choroidal nevomelanocytic tumors. JAMA Ophthalmol. 2013;131:1004–8.
Kaiserman I, Kaiserman N, Pe’er J. Long term ultrasonic follow up of choroidal naevi and their transformation to melanomas. Br J Ophthalmol. 2006;90:994–8.
Thiagalingam S, Wang JJ, Mitchell P. Absence of change in choroidal nevi across 5 years in an older population. Arch Ophthalmol. 2004;122:89–93.
Grewal PS, Oloumi F, Rubin U, Tennant MTS. Deep learning in ophthalmology: a review. Can J Ophthalmol. 2018;53:309–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karthikeyan, A., Harthan, S., Mallanaphy, C. et al. Real-world outcomes of allied health professional-led clinic model for assessing and monitoring ocular melanocytic lesions. Eye 35, 464–469 (2021). https://doi.org/10.1038/s41433-020-0873-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0873-5