Abstract
Background/Objectives
To analyze the ophthalmic characteristics of congenital prepapillary vascular loop (PVL) and to propose a new morphologic classification dividing the loops into six types.
Subjects/Methods
Collaborative multinational multicentre retrospective study of PVL cases.
Results
There was a total of 49 cases (61 eyes), 37 unilateral (75.5%) and 12 bilateral (24.5%), 32 arterial type (65.3%) and 18 venous type (36.7%) (one patient had either kind in each eye). The mean number of loops per eye was 2.7 (range, 1–7). The loops were asymptomatic in 42 cases (85.7%). Other findings included: the presence of cilioretinal artery (14 cases), retinal vascular tortuosity (26 cases), amaurosis fugax (1 case), branch retinal artery occlusion (1 case) and vitreous haemorrhage (3 cases). Six morphologic loop types could be discerned based on elevation (flat vs. elevated), shape (figure of 8 or corkscrew with hyaline sheath), number (multiple or single), location (central or peripheral), lumen size (arterial vs. arteriolar) and presence of vascular tortuosity or vitreous traction.
Conclusions
PVL are usually asymptomatic and can be divided into six morphologic types with different pathogenesis during early embryogenesis.
Similar content being viewed by others
Introduction
Congenital retinal vascular anomalies include anomalous macular macrovessel, arterial–arterial or venous–venous crossing, triple branching, congenital tortuosity and prepapillary vascular loop (PVL) [1, 2]. The terms prepapillary or preretinal [3], vascular or spiral [4, 5] loops into the vitreous have been used interchangeably to characterize this rare anomaly first described in 1871 by Leibrich [6]. Initially, it was misdiagnosed as a variant of hyaloid vessels [4, 5]. One and a half century after its original description, fundus examination, fluorescein angiography [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33] and two histopathological examinations [3, 14] further reaffirmed the clinical impression that PVL originates from a branch of either retinal artery or vein ending at the disk or its immediate vicinity and projecting for a variable distance into the vitreous. Incidence of PVL has ranged from 1 in 2100 to 1 in 9000 in the western literature [17]. In Japan the prevalence was 0.115% [13] while in Africa it was 0.15% [7]. So far, PVL have been divided into arterial (more than 90%) or venous (less than 10%) [8]. The present study aims to analyze several ophthalmic characteristics of PVL concluding in a new morphologic classification.
Materials and methods
This is a retrospective international multicentre cross-sectional review of patients with an established diagnosis of congenital PVL. The study received Institutional Review Board from Rafik Hariri University Hospital. Inclusion criteria were submission of colour fundus photographs to the Reading Center, with or without fluorescein angiography, spectral-domain optical coherence tomography (SD-OCT) or OCT angiography (OCTA). Exclusion criteria included optociliary vessels, primary hyperplastic primary vitreous, arteriovenous communications of retina and other phacomatoses, optic nerve tumour, optic disc coloboma, morning glory syndrome, pseudotumor cerebri, cerebral tumours, peripapillary or extra-papillary vascular loops, central retinal artery or vein occlusion, diabetic retinopathy, carotid vascular disease, congenital heart disorder, retinopathy of prematurity, congenital glaucoma, optic disc cupping, haematologic disorder, intraocular surgery, laser photocoagulation, ocular trauma or new onset of vascular loops. Previously published cases of PVL were also excluded. Fluorescein angiography was a prerequisite especially in venous loops.
The English medical literature was reviewed from 1976 to June 2019 by using PubMed and the terms “prepapillary vascular loop” or “preretinal vascular loop”. Likewise, the same terms were searched using the search engines in Archives of Ophthalmology (1929–2019), American Journal of Ophthalmology (1918–2019) and British Journal of Ophthalmology (1917–2019). Fundus photographs, fluorescein angiograms and OCT were reviewed in these publications. Moreover, fundus photographs were reviewed on American Society of Retina Specialists (Retina Image Ban©) and American Academy of Ophthalmology (Image Gallery©) websites. This extensive review aimed solely at deciphering the various morphological features of PVL, leading to a classification that is then applied to this case series of previously unpublished PVL.
All loops from the collaborative group were classified accordingly by one of us (AMM) based on the colour photographs (type of loop) and fluorescein transits (arterial vs. venous). Retinal vascular tortuosity was subjectively assessed by one of us (AMM) as sinusoidal vessel twist [34]. While the classification was done by one grader, collaborators have independently agreed with the classification and presence of tortuosity (consensus reached). Complications of PVL were noted by the collaborators and documented by fundus photographs and/or fluorescein angiograms.
Results
Forty-nine patients from 23 medical centres in 12 countries from 4 continents fulfilled the inclusion criteria. All had colour fundus photographs submitted to the Reading Center except one surgical case with vitreous haemorrhage. Twelve patients had SD-OCT scans, while 4 patients had OCTA scans. The mean± standard deviation age at first presentation was 37.0 ± 17.6 years (range, 6–79). There was a slight female predominance with 24 women vs. 19 men (6 not specified). The majority were Caucasians: Caucasian 32 cases, African American 4 cases, Latin American 2 cases, Asian 1 case and Indian 1 case (race not specified in 9 cases). The ocular involvement was bilateral in 12, and unilateral in 37 equally divided into 18 right eyes and 19 left eyes. The majority of the loops was arterial in 32 subjects (65.3%) (38 eyes) and the rest venous in 18 subjects (36.7%) (23 eyes). One case had an arterial loop in the right eye and a venous loop in the left eye. The mean number of loops was 2.7 ± 1.5 (range, 1–7): 16 eyes showed 1 loop,12 eyes two loops, 12 eyes had three loops, 17 eyes had four loops, 2 eyes showed five loops and 2 eyes had seven loops.
Retinal vascular tortuosity was present in 26 patients and absent in 22 patients (1 not assessed as intraoperative finding). Cilioretinal artery was present in 14 subjects (16 eyes). Vitreous traction was demonstrated by SD-OCT in one case in both eyes with fellow eye having semi-loop at the disc. Fellow eye status included semi-loop in three eyes, abnormal vascular branching pattern in three eyes (trifurcation in one). and vein crossing over artery in four eyes. The loops were asymptomatic in 42 cases and symptomatic in the remaining 7 cases which included: Branch retinal artery occlusion and mild vitreous haemorrhage with finger counting—1 case; branch retinal vein occlusion with 20/40 (6/12)—1 case; dense vitreous haemorrhage and hand motion vision with PVL detected intraoperatively—1 case; transient mild vitreous haemorrhage with 20/20 (6/6)—2 cases; severe macular pucker—1 case; and amaurosis fugax—1 case. There was no macular or nerve fibre layer pathology by SD-OCT or OCTA in the cases scanned.
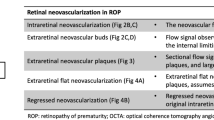
Review of the current series and previously reported cases [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33] (around hundred cases in the literature and on the registries of American Academy of Ophthalmology or American Society of Retina Specialists) allowed us to propose a new morphologic classification dividing the loops into six types (Fig. 1 and Table 1): Type 1—Flat central single intraretinal loop or twist (artery or vein) without associated findings—8 patients (Fig. 2); Type 2—Flat central intraretinal loop or twist (artery or vein) associated with generalized tortuosity of retinal vasculature—9 patients (Fig. 2); Type 3—Flat radial small loops (arteriolar or venular) most often multiple resemble angioma or Chinese letter—10 patients (Fig. 3); Type 4—vitreous loop without sheath in the form of figure of 8 single or multiple protruding into the vitreous cavity shape (artery or vein)—11 patients (Fig. 4). The loop track is along the Cloquet canal; Type 5—vitreous loop with fibrous overgrowth or hyaline sheath and most often Corkscrew shape (artery or vein) (Fig. 5)—10 patients. The fibroglial sheath appears to be a remnant of Bergmeister papilla. One variant of type 5 is when the vessels protruding into the vitreous are straight and ensheathed by glial tissue (Fig. 5). Associated retinal tortuosity may be present (Fig. 5); Type 6—any loop with vitreous traction demonstrated by SD-OCT—1 patient (Fig. 3).
Loop morphology divided into six types (Bottom): Type 1—Flat central single intraretinal loop or twist without associated findings; Type 2—Flat central intraretinal loop with generalized retinal vascular tortuosity; Type 3—Flat radial small loops (arteriolar or venular); Type 4—Loop protrude into vitreous as figure of 8; Type 5—Vitreous corkscrew loop; Type 6—Any loop with associated vitreous traction.
Top composite. Right eye semi-loop (arrowhead) (a) and left eye flat arterial loop type 1 (arrow) (b). Middle composite. Bilateral (c, d) venous type 2 loops and normal anatomy of retina and disc by optical coherence tomography angiography. Bottom composite. Retinal venous tortuosity with type 2 venous loop in right eye (e).
Left composite. Bilateral multiple sector of small corkscrew Type 3 venous loop (arrows) (a) (with permission from Image Bank© 2019 American Society of Retina Specialist) Right composite. Venous loop type 6 (arrows) in the right eye (b) with 20/20 vision and normal intravenous fluorescein angiography transit (c). Optical coherence tomography through the loop of the right eye demonstrates vitreous traction (white arrow) (d). The left eye shows vitreo-papillary traction (white arrow) without presence of a loop (e).
Top composite. Type 4 arterial loop right eye (a) and Type 4 venous loop left eye (b). OCT (c) and OCTA (vitreous scan) (d) demonstrate the left venous loop protruding into Cloquet canal. Bottom composite. Type 4 arterial loops as figure of eight configuration with 4 loops (left bottom) (e) and 7 loops. (right bottom) (f: right eye; g: left eye).
Left top composite. Left eye with Type 5 prepapillary arterial loop (arrow) (a, b) with cilioretinal artery and retinal vascular tortuosity. Left middle composite. Type 5 loop corkscrew arterial loop (white arrow) (c) with the direction of flow shown on fluorescein angiography by black arrows (d) (with permission from Image Gallery© 2019 American Academy of Ophthalmology and Image Bank© 2019 American Society of Retina Specialist). The loop is surrounded by a fibroglial sheath that is probably a remnant of Bergmeister’s papilla. Optic disc pallor and sheathing of cilioretinal artery are results of prior toxaemia of pregnancy 15 years earlier. Left bottom composite. Straight variant of type 5 loop (3 arrows) (e) follows the Cloquet canal into the vitreous and is surrounded by a glial sheath (with permission from Image Gallery© 2019 American Academy of Ophthalmology). Right top composite. Type 5 bilateral arterial loops. OCT shows different level of looping and fibroglial sheath. Severe tortuosity of the retinal vasculature with inferior peripapillary twisting of the artery over the vein in the right eye (arrowhead) (f) and arterial looping just above the disc in the left eye (arrowhead) (g). Right bottom composite. The right eye has Type 5 arterial loop (arrow) (h). The left optic disc has a semi-loop (arrowhead) (i).
Discussion
This report collected the largest variety of PVL in the literature. Besides the well-known division into arterial and venous, a new classification is proposed based on different morphologic appearances (Table 1). While distinct characteristic features define each type an overlap between the different types might exist and some cases could fit into more than one type. Type 1 refers to an isolated flat loop. Type 2 refers to a flat loop as part of a diffuse retinal vascular tortuosity. The retinal vascular tortuosity could be associated with the familial retinal tortuosity syndrome [35]. Type 3 refers to multiple flat small loops assuming a radial location and involving smaller arterioles. This is the prevalent loop in East Asia and Australia, as confirmed in our series and documented in the literature [9]. Types 3 to 6 involve elevated loops into the vitreous with vitreous traction (type 6) or loops advancing into the Cloquet canal mimicking a figure of eight (type 4) or corkscrew with dense hyaline sheath (type 5). Types 4 and 5 share quite similar clinical features resulting from blood stream turbulence and vascular torsion, such as localized retinal haemorrhage, preretinal haemorrhage and vitreous haemorrhage.
There are several known theories for the loop formation: retinal vascular tortuosity spectrum (probably from elastin deficiency [36] or variant of arterial tortuosity syndrome) [37], deficient internal elastic lamina [3, 14], genetic predisposition (autosomal dominant inheritance) [18, 19], vitreous traction on disc leading to loop formation early in life during embryogenesis and pure embryologic focal vascular defect. PVL are thought to be originated from the 100-mm stage of embryonic development when retinal angioblasts arise from the optic nerve head to vascularize the surrounding retina [38,39,40]. Before the fourth month of gestation, the retina is avascular with nutrients supplied by the hyaloid vasculature. At the fourth month (100-mm embryonic stage), the primitive vascular mesenchymal cells adjacent to the hyaloid artery start invading the retinal nerve fibre layer forming the primitive retinal arterial system with concomitant gradual regression of the hyaloid artery. In rare instances, instead of penetrating the nerve fibre layer, the developing vessel grows towards the vitreous within the Cloquet canal for a few millimetres and then turns back to the disc to form PVL. When the configuration is spiral, there is incomplete regression of the hyaloid artery system and a sheath covers the loop. It is possible that types 1–3 loops form earlier in embryogenesis than types 4 and 5.
A majority (>90%) of PVL are of arterial origin [8]. The loop can be near flat or can be elongated [4] extending up to 5 mm from the disc [15]. The longest PVL measured 7.88 mm [15]. The number of loops can vary from 1 to 7. Regenbogen and Godel [16] described an asymptomatic PVL with 6 spirals followed for 12 years. PVL can have 3 shapes: corkscrew (Fig. 5), figure of eight (Fig. 4) or the extremely rare hairpin turn (Fig. 5).
Up to 20% of arterial PVL are bilateral [8]. Blacks appear to have a higher incidence of PVL with less complications than Caucasians [7]. Asians appear to have predominantly type 3 PVL [9,10,11,12,13]. PVL can be familial (autosomal dominant inheritance) with two families reported [18,19,20]. Associated congenital anomalies have included retinal arterial–arterial communication [10, 11, 13, 21], retinal artery tortuosity [7, 22], trifurcation [12], venous retinal macrovessel [23], choroid vein tortuosity [24] and primary hypertrophic primary vitreous [25].
Complications have included vitreous haemorrhage (most self-resolving [27] but some requiring vitrectomy), retinal arterial occlusion [26, 28, 29, 31], preretinal haemorrhage [30] and subretinal haemorrhage [32]. Branch retinal artery occlusion occurs uniquely in arterial PVL and not venous PVL [26, 28, 29, 31]. Spontaneous vitreous haemorrhage after a strenuous activity have been reported due to PVL and is usually mild with spontaneous resolution. Rarely, the accompanying vitreous haemorrhage may be recurrent or severe thereby requiring vitrectomy. In one case anomalous vitreo-PVL adhesion with vitreous traction was noted by SD-OCT and this led to recurrent vitreous haemorrhage [33]. Vitreous traction on the loop has been also demonstrated by SD-OCT [41]. It is of note that kinking or twisting of cerebrovascular vessels have also been associated with occlusion of blood flow [36, 42].
The differential diagnosis of congenital PVL [29, 43] includes optociliary collateral veins in the context of retinal vein occlusion, retinal arteriovenous anastomoses [44], cilio-optic vein [45] and acquired loop following central retinal artery occlusion [46]. Young age, normal visual acuity, negative fluorescein angiography and absence of various systemic diseases help in the diagnosis of congenital PVL.
In conclusion, PVL is a localized ocular finding with no known systemic vascular association. Complications are uncommon. The loop tortuosity-induced flow alterations impose a high degree of stress on the endothelial cells of the loop resulting in thrombosis or rupture. PVL can be divided into six morphologic types based on location (second branch artery or third branch arteriole), loop elevation, loop shape, loop covering and vitreo-retinal traction.
Summary
What is known about topic
-
Prepapillary vascular loops were divided into arterial and venous loops.
What this study adds
-
Prepapillary vascular loop are classified into isolated flat loop with or without retinal vascular tortuosity, multiple radial flat loops, figure of eight loop, corkscrew loop and tractional loop.
References
Awan KJ. Arterial vascular anomalies of the retina. Arch Ophthalmol. 1977;95:1197–202.
Awan KJ. Anomalies of the retinal veins and their incidence. J Pediatr Ophthalmol. 1976;13:353–9.
Goldstin I, Wexler D. The preretinal artery. An anatomic study. Arch Ophthalmol. 1929;1:324–34.
Merrill UH, Wagener HP. Anomalous spiral looping of a retinal vein. Am J Ophthalmol. 1924;7:177–9.
Francis LM. Anomalous spiral looping of retinal artery. Am J Ophthalmol. 1921;4:202–3.
Liebreich R. Demonstrations of diseases of the eye: persistent hyaloid artery and vein. Trans Pathol Soc Lond. 1871;22:221–4.
Kaimbo Wa Kaimbo D. Frequency of prepapillary vascular loops in Congolese patients. J Fr Ophtalmol. 2016;39:711–5.
Degenhart W, Brown GC, Augsburger JJ, Magargal L. Prepapillary vascular loops. Ophthalmology. 1981;88:1126–31.
Hsieh YT, Yang CM. The clinical study of congenital looped/coiled peripapillary retinal vessels. Eye. 2005;19:906–9.
Nishimura T, Uyama M. Retinal vascular loop formation on the optic disc. Jpn J Clin Ophthalmol. 1982;36:1371–5.
Tamura M, Atsumi O, Yoshimoto H. Retinal vascular loop formation on the optic disc: retrospective study of eleven cases. Folia Ophthalmol Jpn. 1991;42:304–10.
Teramoto S, Ohno-Matsui K, Tokoro T, Ohno S. Peripapillary loops of venous origin are extremely rare. Jpn J Ophthalmol. 1999;43:422–5.
Makino S. Prevalence of prepapillary vascular loop. Scholars J Appl Med Sci. 2015;3:693–4.
Shakin EP, Shields JA, Augsburger JJ, Brown GC. Clinicopathologic correlation of a prepapillary vascular loop. Retina. 1988;8:55–8.
Mireskandari K, Aclimandos WA. Probably the longest prepapillary loop in the world. Retina. 2001;21:393–5.
Regenbogen L, Godel V. Spiral looping of retinal artery. J Pediatr Ophthalmol. 1977;14:117–9.
Romano PE. Prepapillary vascular loops. Clin Exp Ophthalmol. 2001;29:90–1.
Grossniklaus H, Thall E, Annable W. Familial prepapillary vascular loops. Arch Ophthalmol. 1986;104:1755–6.
Lambert HM, Sipperley JO, Shacklett DE. Autosomal dominant preretinal vascular loops. Retina. 1983;3:258–60.
Morán M. [Inherited (Pre)retinal arterial loop (author’s transl)]. Cesk Oftalmol. 1981;37:436–43.
Sugiuchi K, Mori K, Deguchi T, Yoneya S. [Chorioretinal malformation in vascular loop formation on the optic disc]. Nippon Ganka Gakkai Zasshi. 1998;102:215–20.
Punja K, Sharma S. Ophthaproblem. Prepapillary vascular loops. Can Fam Physician. 2002;48:41–50.
Soltau JB, Olk RJ, Gordon JM. Prepapillary arterial loop associated with vitreous hemorrhage and venous retinal macrovessel. Retina. 1996;16:74–5.
Giuffrè G, Lodato G. Prepapillary venous loops and choroidal veins tortuosity. Acta Ophthalmol. 2003;81:665–6.
Walland M. Prepapillary vascular loop associated with persistent hyperplastic primary vitreous. JAMA Ophthalmol. 2015;133:362.
Brown GC, Magargal L, Augsberger JJ, Shields JA. Preretinal arterial loops and retinal arterial occlusion. Am J Ophthalmol. 1979;87:646–51.
Brucker AJ, Michels RG, Fine SL. Congenital retinal loops and vitreous haemorrhage. Am J Ophthalmol. 1977;84:220–3.
Rahimy E, Rayess N, Talamini CL, Kaiser RS. Traumatic prepapillary loop torsion and associated branch retinal artery occlusion. JAMA Ophthalmol. 2014;132:1376–7.
Codenotti M, Fogliato G, De Benedetto U, et al. Simultaneous vitreous hemorrhage and branch retinal artery occlusion after prepapillary arterial loop rupture. J Fr Ophtalmol. 2013;36:e63–5.
Ding PC, Chen MT. Peripapillary arterial loop-case report. Kaohsiung J Med Sci. 1999;15:510–2.
Misra A, Flanagan DW, Martin KR. Recurrent transient visual loss due to intermittent occlusion of a prepapillary vascular loop. Br J Ophthalmol. 2008;92:431–2.
Fujiwara T, Machida S, Herai T, Tazawa Y. Case of subretinal hemorrhage that developed from a prepapillary vascular loop. Jpn J Ophthalmol. 2004;48:175–7.
Youssoufou Souley AS, Alsubari A, Chammout FZ, et al. [Prepapillary vascular loop with vitreous traction]. J Fr Ophtalmol. 2018;41:1002.
Owen CG, Rudnicka AR, Mullen R, et al. Measuring retinal vessel tortuosity in 10-year-old children: Validation of the computer-assisted image analysis of the retina (CAIAR) program. Investig Ophthalmol Vis Sci. 2009;50:2004–10.
Sutter FKP, Helbig H. Familial retinal arteriolar tortuosity: a review. Surv Ophthalmol. 2003;48:245–55.
Lee KE, Jeong EH, Yu HJ, et al. Cerebral infarction caused by a tortuous subclavian artery: a case report. Neurointervention. 2014;9:53–5.
Beyens A, Albuisson J, Boel A, et al. Arterial tortuosity syndrome: 40 new families and literature review. Genet Med. 2018;20:1236–45.
Fruttiger M. Development of the retinal vasculature. Angiogenesis. 2007;10:77–88.
Toma N. Anatomy of the ophthalmic artery: embryological consideration. Neurol Med Chir. 2016;56:585–91.
McLeod DS, Hasegawa T, Prow T, et al. The initial fetal human retinal vasculature develops by vasculogenesis. Dev Dyn. 2006;235:3336–47.
Raman R, Gella L, Kazi MS. Congenital preretinal arterial loop: Is it a misnomer? Oman J Ophthalmol. 2017;10:54–5.
Han HC. Twisted blood vessels: symptoms, etiology and biomechanical mechanisms. J Vasc Res. 2012;49:185–97.
Vedantham V, Ramasamy K, Namperumalsamy P, Cunningham ET. Double prepapillary arterial loops associated with superior branch macular artery occlusion. Ind J Ophthalmol. 2005;53:126–8.
Mansour AM, Walsh JB, Henkind P. Arteriovenous anastomoses of the retina. Ophthalmology. 1987;94:35–40.
Zaret CR, Choromokos EA, Meisler DM. Cilio-optic vein associated with phakomatosis. Ophthalmology. 1980;87:330–6.
Cohen SY. Acquired prepapillary arterial loop after central retinal artery obstruction. Arch Ophthalmol. 1998;116:1398–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mansour, A.M., Kozak, I., Saatci, A.O. et al. Prepapillary vascular loop-a new classification. Eye 35, 425–432 (2021). https://doi.org/10.1038/s41433-020-0859-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0859-3
This article is cited by
-
The RETA Benchmark for Retinal Vascular Tree Analysis
Scientific Data (2022)
-
The prevalance of congenital optic disc anomalies in Turkey: a hospital-based study
International Ophthalmology (2022)