Abstract
Trainee involvement in cataract surgery is vital to allow proper training of the next generation of ophthalmic surgeons. However, recent changes in the UK Law, coupled with open publication of National Cataract Dataset results, lead us to conclude that the status of being a trainee is itself a material risk that now needs to be divulged to patients during the consent process. The opinions of current trainee surgeons in the UK were sampled via questionnaire and clinical negligence counsel was involved in the authorship of the paper in order to analyse the legal issues at stake. Attitudes towards consent regarding trainee involvement in UK cataract surgery need to change.
Similar content being viewed by others
Introduction
The Law regarding consent has changed: the decision of Montgomery v Lanarkshire Health Board confirmed that clinicians are under a duty to warn their patients of ‘material risks’ to surgical procedures [1]. In this paper, we consider whether—in light of Montgomery and the current law on consent—clinicians are duty bound to discuss with patients the involvement of trainee surgeons in cataract surgery, given that there is a higher complication rate when trainees perform such surgery [2]. Does that proven statistical risk represent a ‘material risk’ of which the patient ought to be informed?
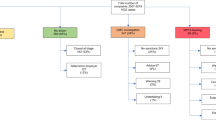
In surgery in general, it can be difficult to prove that trainee involvement in procedures results in worse peri- or post-operative outcomes, however, this is not the case for cataract surgery [3,4,5,6,7,8,9,10,11]. For several years information has been available on an NHS website from the associated National Cataract Dataset (NCD), which gives individuals’ complication rates and percentage risks: such information is now in the public domain and hence available to patients and lawyers (https://www.nhs.uk/Service-Search/Consultants/Indicators/Service/5550021). The publication of the UK NCD electronic multicentre audit highlighted that, among other factors, trainee surgeons performing operations are an independent risk factor for surgery. This risk will of course fluctuate depending on the seniority of the trainee (and patient comorbidities). In an individual case, depending on the risk factors, the increased risk of a complication occurring compared with a consultant operating could be as low as a 2% increased risk or as high as 30% [2]. In the majority of cases, the absolute difference in percentage risk between different surgeons will be very small—often only 2–5%—however, received wisdom teaches us that while patients understand that there is a small risk involved, the majority would prefer this risk to be reduced to its lowest possible level.
The Law
The decision of the Supreme Court in Montgomery v Lanarkshire Health Board marked a sea change in the law of consent [1]. Although there had been significant judicial movement towards a doctrine of ‘informed consent’ it was only with the Montgomery decision that the country’s most senior Court fully endorsed such an approach.
In the seminal case of Bolam, it was said that a clinician would not be negligent in taking consent, provided the doctor acted in accordance with ‘a practice accepted as proper by a responsible body of medical men skilled in that particular art’ [12]. Bolam was heard in 1957, and its language alone belongs to a different era. Not only are doctors (and lawyers) no longer to be presumed to be male, the doctor/patient relationship has evolved, and society has changed significantly since the case was decided.
The evolution of the doctor/patient relationship was reflected in some judicial decisions before Montgomery. In the 1984 case of Sidaway [13], the Law Lords began to wrestle with the idea of a doctrine of informed consent, which was already recognised in the United States, but which had never been a part of English jurisprudence. Most significant were the dissenting comments of Lord Scarman, who concluded that ‘English law must recognise a duty of the doctor to warn his patient of risk inherent in the treatment he is proposing: and especially so if the treatment be surgery…’. However, he went on, ‘Even if the risk be material, the doctor will not be liable if upon a reasonable assessment of his patient’s condition he takes the view that a warning would be detrimental to his patient’s health’. [13] This idea, that there would, on occasions, be reasons why a doctor might justifiably withhold information from a patient (where it might be detrimental to the patient’s wellbeing, including their mental wellbeing) is what is sometimes referred to as the ‘therapeutic exception’.
In 1992, the High Court of Australia also sought to address the conflict between the American doctrine and the English approach in the case of Rogers v Whitaker [14]. Maree Whitaker became essentially blind after a successful operation for an unsightly cataract in a previously traumatised and blind right eye caused sympathetic ophthalmia in her left eye. The skill and competency of Dr Rogers were not in question as a result of this rare (1 in 14,000) risk occurring, however, Ms Whitaker felt that Dr Rogers had failed in his duty of care by not informing her of the risk that sympathetic ophthalmia could develop. The High Court of Australia awarded damages to Mrs Whitaker as she had expressed concern that her ‘good eye’ not be harmed and Dr Rogers had not informed her of the potential risk to this eye as a result of the surgery. The High Court determined that a doctor has a duty to warn a patient of any material risks involved in a proposed treatment [14]. Arguably, then, Montgomery was long overdue. When the judgement was delivered, the GMC welcomed it as the law simply catching up with established guidance on consent.
Material risk
Montgomery made clear that patients are entitled to be informed of ‘material’ risks; the Supreme Court classified the test of materiality as ‘whether, in the circumstances of a particular case a reasonable person in the patient’s position would be likely to attach significance to the risk’ [1]. The test, then, is partly objective (‘the reasonable person’) and partly subjective (‘in the patient’s position’). While Montgomery centred on the materiality to a pregnant diabetic woman of the enhanced risk of a normal vaginal delivery, there are clear parallels to cataract surgery.
What, then, of the risk which attaches to a trainee performing cataract surgery? Some guidance is to be found in the GMC guidance on consent. GMC guidance section 9(e), for example, states that doctors must tell patients if the risks and benefits of an intervention ‘are affected by which organisation or doctor is chosen to provide care’ [15]. Cataract surgery is, however, unusual. Whereas in many other disciplines, there might be a senior surgeon assisted by a more junior one, with the junior participating in more steps as (s)he progresses in his/her experience and skill, cataract surgery is unusual in that it is a single operator procedure: even if a junior surgeon is not performing the whole case, there can be only one primary operator at any one time. This means that the risk of a complication occurring lies mainly with the surgeon performing the procedure at the time. This personalised risk of complications is highlighted in the NCD; complication rates are attributed to the individual surgeon (and hence grade of surgeon) [2].
This publication of individual complication rates puts trainee surgeons in a precarious position as it means that complication rates are ascribed to them individually as well and—as highlighted by the NCD—juniors tend to have a higher complication rate than senior surgeons performing the same cases. While this increase in absolute risk may be less for more routine cases, it can increase exponentially if the case has multiple risk factors (https://www.nhs.uk/Service-Search/Consultants/Indicators/Service/5550021) [2] .
Recent NICE Cataract Guidelines specifically mention that at the patient’s pre-operative appointment ‘the person’s individual risk of complications during or after surgery’ be discussed with them; included in this individualised risk would naturally be the person performing their operation, be they a trainee surgeon or not [16]. After submitting all relevant clinical details, including the grade of surgeon planned, modern electronic patient record software for cataract surgery typically provides the clinician with a percentage chance of a posterior capsule rupture (PCR) complication for a specific case. Such a figure would surely be very likely judged to be material to a patient, as PCR is associated with a substantial increase in the risk of visual loss and associated morbidity [2]. NICE guidelines also allow risk stratification to help choose which surgical list cases are allocated to; while this is an important part of risk minimisation for a population in general, considerations of consent and the materiality of risk must be individual, and not population specific [16].
What are trainees’ current opinions regarding UK cataract consent practice?
Patients’ and trainers’ opinions on the matter of trainee involvement in cataract surgery have been previously investigated and the outcomes of such investigations have highlighted how sensitive this issue is [17, 18]. As a part of our team’s work on this subject, we sought to investigate trainees’ opinions regarding UK current consent practice, as well as trainees’ attitudes, perspectives and concerns regarding discussing their involvement as an independent risk factor for surgery.
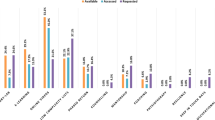
An invitation to participate in an online survey (SurveyMonkey software) was sent to all ophthalmology trainees working in the West Midlands region of the UK. Data were prospectively collected over a 5-month period (September 2018 to January 2019). Trainees were asked to respond anonymously to ten questions concerning their contemporaneous discussions with patients about trainee involvement in cataract surgery, allowing collation of what information they disclose and also their opinions on this issue.
The questions were designed to investigate whether trainee participation in surgery is discussed with patients or not, who discloses this to patients (e.g., consultants, the trainees themselves or other health professionals involved in the cataract surgery process) and how it is disclosed. Trainees were also asked to give their opinion regarding other aspects of surgery, such as two-tier waiting lists, unsupervised surgery and if they would be comfortable disclosing their complication rate. Free text comments were also included. Of the 54 trainees who were polled, 30 responded to the questionnaire. All who were invited to complete the questionnaire were current trainees within the West Midlands region. The questions posed and associated results are shown in Table 1.
Practical difficulties of taking consent from patients
Our questionnaire results highlight how difficult an area this can be to address in practice. The majority of trainees and also their consultants did not specifically discuss trainee involvement in cataract surgery and the vast majority did not discuss the potential increased risk of complications associated with trainee surgeons (even though such information is in the public domain and hence potentially available to patients and their legal advisers). There was an even split between respondents as to whether they would be comfortable discussing their own complication rate or not with patients; this concern is understandable and is highlighted by the comments left by the respondents, with concerns regarding whether patients would decline to have the operation done, if they thought it would be done by a trainee.
Some respondents felt that there was implied consent by virtue of either the trainee taking consent, or the venue being a teaching hospital. It can be risky to assume, however, that consent to trainee involvement is implied in either scenario.
Can a patient specify their choice of surgeon?
Clearly in the private sector, this is not an issue. However, in 2015 case of Jones v Royal Devon & Exeter NHS Foundation Trust, the Court found that there had been a breach of duty where the surgeon who performed the operation was not the surgeon that the Claimant had expected [19]. The case was decided in the County Court, and it does not therefore carry as much weight as if it were a decision of the higher courts, but it is of interest nonetheless. The patient had sought to bring her spinal decompression surgery forward, but had been told that if she did so, it would not be her named consultant who would operate. After some discussion with her GP, she decided to wait until her named consultant was available, only to find out on the day of surgery that her operation was to be performed by a trainee. The consent form, which had been signed by the Claimant, specifically recorded that another surgeon might perform the surgery, but the Judge found that her decision to proceed—taken on the day of the surgery—was too late to amount to informed consent, and said that ‘a decision (to consent to the operation) taken so far down the line is unlikely to be taken freely’. The evidence of the Claimant was that she felt unable to object to the change of surgeon as she felt she had reached ‘the point of no return’ on the day of surgery [19].
Some of our questionnaire’s respondents commented that one reason for not obtaining consent to trainee involvement in surgery was because they could not guarantee who would be performing the operation, although this seems to us to be a spurious reason for not discussing trainee involvement. In practice, for many eye units across the UK, patients are seen in a pre-operative clinic and placed into a general waiting list ‘pool’. This means that for a large number of patients, the clinician whom they saw in clinic will not be the surgeon they meet on the day of surgery. For many, the day of surgery may also be the first time they are met by a trainee and therefore realise that the named consultant on their appointment letter may not be the individual undertaking the surgery. If patients are not adequately informed that a trainee surgeon may be performing their surgery in advance, as well as the potential increased risk that this poses, it could be argued that the consent has been invalidated, should a trainee undertake that surgery.
Do patients object to the involvement of trainees?
A survey of cataract surgery patients in 2008 highlighted that while 70% of patients are generally accepting of trainees operating as a part of their training, only 57% of patients were happy to be operated on by a supervised surgical trainee and 22% were happy to be operated on by an unsupervised trainee [17]. Yet, in clinical practice we do not see such high numbers of patients objecting or even walking away on the day of surgery when faced with the prospect of a trainee doing their operation. Is this because patients feel they have reached ‘the point of no return’ (referred to by the Claimant in Jones [19]) when they reach the surgical unit? If this were the reason, the validity of the consent process could certainly be open to challenge.
The timing of consent
It is now widely accepted, in medical and legal circles, that consent is a process and that, as such, it should take place over a period of time. As per the observations in Jones, it is unsatisfactory to take consent from patients on the day of the procedure [19]. Nonetheless, and in spite of the GMC guidance which advocates an adequate ‘cooling off’ period for patients giving consent to a procedure, a national trainers’ survey conducted in 2012 found that 60% of respondents were still taking consent on the day of surgery [15, 18].
How, in practice, should we take consent?
So how should we be obtaining consent from our patients in a way that discloses trainee involvement (and the possible risk that may be entailed with that) without discouraging patients? The future of the NHS depends on training opportunities and competent new surgeons coming through the ranks.
Clinicians would not, of course, wish to scare patients with the statistics. In Sidaway, Lord Scarman commented that ‘a doctor acting in the best interests of his patient would be concerned lest a warning might frighten the patient into refusing an operation which in his view was the best treatment for the patient’. He went on, ‘The doctor should have the opportunity of proving that he reasonably believed that disclosure of the risk would be damaging to his patient or contrary to his best interest’: the concept of the therapeutic exception [13].
Could the therapeutic exception be invoked so as to leave out of the consent process the particular risks, which attach to a trainee surgeon? It does not seem to us proper to use the therapeutic exception in such a way—it is, after all, something which is to be invoked where the information might do harm to the patient and it would surely be difficult—particularly in the current judicial climate—to assert that arming a patient with information might do them harm. Furthermore, there is a school of thought that the therapeutic exception has no place in the current state of the law surrounding consent [20].
Studies investigating whether patients would agree to undergo cataract surgery after being informed that a trainee would be actively involved show a huge disparity in consent rates from 16 to 95.3% [17, 21, 22]. Research has shown that patients’ attitudes to trainee involvement depend not only on the information, which is given to patients, but also on how such information is imparted. One study comparing different techniques of consent to trainee involvement in cataract surgery produced different consent rates, depending on the approach to consent. A purely written consent form with no verbal discussion or recommendation saw a low rate of consent of 21%, which contrasted with techniques where a verbal discussion was had with the patient (86% for one technique and 67% for the other). The highest consent rate was achieved by a surgeon delivering a broadly scripted, yet reassuring statement regarding trainee participation, involving the patient more in the decision-making process by explaining why training was important, as well as the reassurance of close supervision [22, 23]. This highlights the importance of how we describe trainee participation and shows that, with clear explanation and patient involvement, high consent rates to trainee participation can be achieved.
Unsupervised surgery may be considered essential for more senior trainees nearing the completion of training in order to simulate working conditions similar to what they will experience as a consultant, with 97% of trainees in our questionnaire reporting that unsupervised surgery was important to their training. Unsupervised surgery by trainees is not, however, popular with patients, with only 22% of patients happy for this to occur [17]. Part of this may be due to the label of ‘trainee’, which can cover doctors from foundation level to consultant-in-waiting, the previous distinction of SHO, registrar and senior registrar having greater discriminatory power. In 2017, Petravick et al. investigated levels of patient and family member comfort with US trainees’ (non-ophthalmic) surgery [24]. They broke this up into six steps of surgery (e.g., preparing and draping, critical steps, etc.) and four levels of experience: medical student, intern, resident and fellow; not surprisingly, respondents were much happier with residents and fellows performing more parts of the surgery. While a decline was seen in the comfort levels if a senior surgeon was absent from the theatre, a significant difference was still seen between the comfort levels of a more junior trainee compared with a more senior trainee performing the operation [24]. Making the grade of the trainee clear to patients during the consent process may reassure them and make them more likely to give consent freely. While the NCD only makes a differentiation between consultant and trainee, it would be interesting to see a breakdown of risk according to grade of trainee as it is likely that senior trainees would have comparable complication rates to their consultant counterparts [2]. Such information could indeed prove useful in reassuring patients undergoing unsupervised trainee surgery.
Of course, estimates of the risk of cataract surgery may also vary between consultant surgeons too. For many UK consultant cataract surgeons, this information is freely available online, however, such information may mislead patients still further (https://www.nhs.uk/Service-Search/Consultants/Indicators/Service/5550021). Patients may assume that they have minimised their complication risk by utilising the tool to seek the ‘safest’ surgeon, however, if a trainee performs the surgery on the day instead, the data quickly become at best irrelevant and at worst frankly misleading. This could be compounded by the ‘best’ surgeons (entirely reasonably) being allocated the least able trainees.
Two-tier waiting lists?
A two-tier waiting list solution may address the issue, whereby patients are given the choice of a consultant-only list, likely with a longer delay to surgery, or a training list, likely with a shorter wait. In a previous study of patients’ attitudes to trainee surgeons performing cataract surgery, 79% of patients stated they would prefer to wait longer for their surgery if it meant a consultant would perform it [17]. In our questionnaire, only 33% of respondents felt that a two-tier list should be offered, however, which is in stark contrast with patients’ wishes, the main concern of clinicians being the negative impact it may have on training opportunities. Not only might the number of training cases be fewer were patients allowed this choice, but the burden it would create on hospitals could potentially make it unsustainable. The mix of cases might also become less appropriate as those with more prominent visual symptoms and therefore denser, more complex cataracts may end up on the training lists in disproportionate numbers, as such patients might prefer their operation to be done sooner. For more senior trainees this may not be an issue, but for more junior trainees it might mean opportunities to operate would be further reduced and their development into competent surgeons subsequently stunted, without further consideration.
Conclusion
Trainee involvement in cataract surgery is certainly a material risk and needs to be divulged to patients as such. As our discussion has shown, consent for trainee involvement cannot be implied simply because a line is placed in the consent form or leaflet; it cannot also be implied simply because the patient is having their operation in a teaching hospital. The fear of patients saying no to trainee involvement is understandable, however, rather than being seen as a sensitive topic it should be something that we should aspire to discuss openly with our patients. Patients should be encouraged by the fact that they are having their operation performed in a training hospital where the level of supervision and cover is potentially high, as well as such facilities perhaps being best equipped to deal with potential complications.
Surgical risk may be higher with trainee involvement, however, this can be minimised with judicious case selection according to the surgical grade of the trainee. While tools, such as the risk calculator described in the NCD, can be used in case selection, the choice of individual surgeon will depend on the trainee’s experience, as well as an assessment by their supervisor of their suitability to perform the operation. Only in this way can we ensure that trainees continue to develop their skills appropriately so that they are suitably prepared to tackle the challenging cases that a consultant surgeon will be faced with. Trainees should be able to feel that they are working in a supportive environment without fear of reprisal from patients who feel their consent was not properly obtained.
References
Montgomery v Lanarkshire Health Board [2015] SC 11 [2015] AC 1430.
Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye. 2009;23:31–7. https://doi.org/10.1038/sj.eye.6703049.
van der Leeuw RM, Lombarts KM, Arah OA, Heineman MJ. A systematic review of the effects of residency training on patient outcomes. BMC Med. 2012;10:65 https://doi.org/10.1186/1741-7015-10-65.
Storey R, Frampton C, Kieser D, Ailabouni R, Hooper G. Does orthopaedic training compromise the outcome in knee joint arthroplasty? J Surg Educ. 2018;75:1292–8. https://doi.org/10.1016/j.jsurg.2018.02.011.
Robson AJ, Wallace CG, Sharma AK, Nixon SJ, Paterson-Brown S. Effects of training and supervision on recurrence rate after inguinal hernia repair. Br J Surg. 2004;91:774–7.
Saxena A, Virk SA, Bowman SRA, Jeremy R, Bannon PG. Heart valve surgery performed by trainee surgeons: meta-analysis of clinical outcomes. Heart Lung Circ. 2018;27:420–6. https://doi.org/10.1016/j.hlc.2017.10.009.
Sheyn D, Bretschneider CE, Canfield D, Duarte M, Mangel JM, Mahajan ST. Impact of trainee involvement on complication rates following pelvic reconstructive surgery. Female Pelvic Med Reconstr Surg. 2018. https://doi.org/10.1097/SPV.0000000000000575.
Harris IA, Lin C. Orthopaedic trauma surgery performed by unsupervised and supervised trainees: complication rates compared. J Orthop Surg. 2007;15:264–6.
Hawkins W, Moorthy K, Tighe D, Yoong K, Patel R. With adequate supervision, the grade of the operating surgeon is not a determinant of outcome for patients undergoing urgent colorectal surgery. Ann R Coll Surg Engl. 2007;89:760–5.
Ferrah N, Stephan K, Lovell J, Ibrahim J, Beiles B. Post-operative complications following emergency operations performed by trainee surgeons: a retrospective analysis of surgical deaths. World J Surg. 2018;42:2329–38. https://doi.org/10.1007/s00268-018-4465.
Wong K, Duncan T, Pearson A. Unsupervised laparoscopic appendicectomy by surgical trainees is safe and time-effective. Asian J Surg. 2007;30:161–6.
Bolam v Friern Hospital Management Committee [1957] 1 WLR 582.
Sidaway v Board of Governors of the Bethlem Royal Hospital [1985] AC 871.
Rogers v Whitaker [1992] HCA 58.
General Medical Council. Consent: patients and doctors making decisions together. London: GMC; 2008.
Cataracts in adults: management—NICE Guidance NG77. 2017.
Moodie JJ, Masood I, Tint N, Rubinstein M, Vernon SA. Patients’ attitudes towards trainee surgeons performing cataract surgery at a teaching hospital. Eye. 2008;22:1183–6.
Steeples L, Mercieca K, Smyth K. Consent for cataract surgery training: a national trainers’ survey. Eye. 2012;26:666–70. https://doi.org/10.1038/eye.2012.2.
Jones v Royal Devon & Exeter NHS Foundation Trust [2008] EWHC 558.
Cave E. The ill-informed: consent to medical treatment and the therapeutic exception. Common Law World Rev. 2017;46:140–68.
Nguyen T, Silver D, Arthurs B. Consent to cataract surgery performed by residents. Can J Ophthalmol. 2005;40:34–7.
Gan KD, Rudnisky CJ, Weis E. Discussing resident participation in cataract surgery. Can J Ophthalmol. 2009;44:651–4.
Sharda RK, Sher JH, Chan BJ, Kobetz LE, Mann KD. A comparison of techniques: informed consent for resident involvement in cataract surgery. Can J Ophthalmol. 2012;47:113–7.
Petravick ME, Edgington JP, Idowu OA, Shi LL, Lee MJ. It all depends on who does what: a survey of patient and family member comfort with surgical trainees operating. J Surg Educ. 2017;74:1001–6. https://doi.org/10.1016/j.jsurg.2017.05.014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Qadir, M.O., Abdallah, Y., Mulholland, H. et al. Montgomery in, Bolam out: are trainee surgeons ‘material risks’ when taking consent for cataract surgery?. Eye 34, 1334–1340 (2020). https://doi.org/10.1038/s41433-020-0785-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0785-4
This article is cited by
-
Material risk: vitreoretinal surgery, evisceration, enucleation and sympathetic ophthalmia—where are we currently?
Eye (2023)
-
Comment on: Montgomery in, Bolam out: are trainee surgeons ‘material risks’ when taking consent for cataract surgery?
Eye (2022)
-
Response to: ‘Montgomery in, Bolam out: are trainee surgeons “material risks” when taking consent for cataract surgery?’
Eye (2021)