Abstract
Purpose
To compare the efficacy of topical 0.03% tacrolimus in combination with systemic corticosteroids versus systemic mycophenolate mofetil (MMF) and corticosteroids in preventing corneal allograft rejection after repeat keratoplasty.
Methods
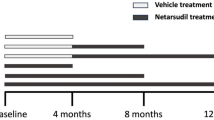
This prospective, randomized clinical trial enrolled 63 consecutive eyes of 63 patients who underwent repeat keratoplasty after a failed penetrating keratoplasty. Group 1 (32 eyes) received MMF orally 1 g twice daily for the first 6 months and then 1 g daily for the next 6 months, and group 2 (31 eyes) received topical 0.03% tacrolimus four times a day for 12 months. All patients were treated with topical and oral corticosteroids postoperatively. The participants were observed closely for signs of graft rejection, and the rates of rejection-free graft survival were calculated and compared between the two groups at postoperative month 12.
Results
The groups were balanced in patient’s age and risk factors for graft rejection (e.g., original diagnosis, number of previous grafts, and quadrants of corneal vascularization). Endothelial graft rejection occurred in 5 eyes (15.6%) of group 1 and 6 eyes (19.4%) of group 2 (P = 0.75). Irreversible endothelial graft rejection resulting in graft failure occurred in 3 eyes of each group (P = 0.99). The rate of rejection-free graft survival was 84.4% in group 1 and 80.6% in group 2 at postoperative month 12 (P = 0.74).
Conclusion
Topical 0.03% tacrolimus was as effective as systemic MMF as adjuncts to topical and systemic corticosteroids in reducing endothelial graft rejection with 12 months follow up after repeat keratoplasty.
Similar content being viewed by others
Introduction
Repeat keratoplasty continues to be an important indication for corneal transplantation in many centers, and it accounts for up to 41% (varying from 6 to 41%) of all keratoplasty cases performed [1]. In contrast to first-time grafts that enjoy high survival rate in so-called “low-risk” eyes (90% at 5 years and 82% at 10 years), only 18% of re-transplanted corneas survive at 5 years [2, 3]. The most common cause of graft failure in repeated corneal transplantation is immunologic rejection [1, 4, 5]. Same recipient factors play a role in graft rejection in both the initial grafts and regrafts; however, regrafts suffer from additional risk factors that have been acquired as a result of the original transplant surgery such as inflammation, corneal angiogenesis, peripheral anterior synechia formation, and progression of glaucoma [4]. In addition, a previously failed graft increases the risk of rejection in the subsequent transplants due to more efficient immunization against the donor antigens [6].
Systemic immunosuppression with mycophenolate mofetil (MMF) has been reported to be efficient and improve corneal graft prognosis considerably in high-risk grafts including repeat keratoplasty [7,8,9,10,11]. MMF is the bioavailability-enhanced prodrug of the active substance mycophenolic acid that inhibits the de novo synthesis of guanosine nucleotides by reversibly inhibiting inosine monophosphate dehydrogenase [12]. This leads to selective inhibition of B- and T-lymphocyte proliferation, as they are dependent on de novo purine synthesis [12]. This therapeutic option, however, is associated with some complications, such as infection, leukopenia, anemia, gastrointestinal disturbances, arterial hypertension, and hyperlipidemia [13]. These complications, some of which are life-threatening, may outweigh any benefits from graft survival; therefore, it makes this approach inappropriate for many patients with high-risk corneal transplants.
The local administration of immunosuppressives has the benefit of limiting the drug toxicity to the eye; therefore, some topical immunosuppressive medications have been advocated for reduction of immunologic rejection in high-risk grafts. Tacrolimus (FK506) is a macrolide antibiotic produced by Streptomyces tsukubaensis [14]. It is a member of the calcineurin inhibitor family with a potent immunosuppressive activity. Similar to cyclosporine, tacrolimus inhibits the initial phase of T-cell activation resulting in inhibition of IL-2 transcription and T-cell signal transduction. Additionally, cytokine release of TNF-α, IFN-γ, and other interleukins is also affected by tacrolimus [15, 16]. Topical tacrolimus has been effectively used in inflammatory anterior segment diseases, including nummular adenoviral keratitis, atopic keratoconjunctivitis, and Thygeson’s superficial punctate keratitis [17]. Some studies have shown the ability of tacrolimus to reduce immunologic graft rejection in human high-risk corneal transplantation [18, 19]. These studies, however, are retrospective, with different disease backgrounds and follow-up times. Herein, we report the one-year outcomes of a prospective randomized clinical trial in which the efficacy of topical tacrolimus was compared to systemically administered MMF in conjunction with topical and systemic corticosteroids for prevention of corneal graft rejection after repeat keratoplasty.
Materials and methods
This prospective, randomized clinical trial (Identifier; NCT04147390) enrolled 63 consecutive eyes of 63 patients who were scheduled for repeat corneal transplantation following failed primary penetrating keratoplasty (PK). The study was performed according to the 1964 Declaration of Helsinki and the study protocol was approved by the Ethics Committee, affiliated with the Shahid Beheshti University of Medical Sciences in Tehran, Iran. The informed consent form was signed by all the patients after the purpose of the intervention was explained.
Exclusion criteria included uncontrolled increase in intraocular pressure, active herpetic keratitis and corneal ulcer, limbal stem cell deficiency, and a history of limbal stem cell transplantation. In addition, age less than 18 years, pregnancy, a history of malignant disorders, abnormal liver or kidney function, the presence of poorly controlled systemic hypertension and diabetes mellitus, systemic infections, active peptic ulcer disease, and any gastrointestinal disorders led to patient exclusion.
Preoperative evaluation
A thorough medical history was taken, and physical and laboratory examinations, including blood pressure, cell blood count, urea, creatinine, and liver function tests, were performed for each patient. Preoperatively, uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA), and manifest refraction (when possible) were measured. Other preoperative examinations included slit-lamp examination, applanation tonometry, and dilated fundus examination. The data compiled included patient’s sex, age at the time of initial and the most recent keratoplasty, indication for initial keratoplasty, number of transplants, history of glaucoma surgery, history of herpetic keratitis, topical and systemic medications taken at the time of enrollment, quadrants of peripheral corneal neovascularization, lens status prior to the last grafting, donor characteristics, and the donor trephine size.
Surgical technique
No active matching for donor and recipient MHC antigens were performed. All donor corneas were stored in Optisol GS medium (Bausch and Lomb, Rochester, NY, USA) at 4 °C. Repeat keratoplasty consisted of Descemet stripping automated endothelial keratoplasty (DSAEK) and PK. DSAEK was chosen when the failed graft was edematous without significant opacities and vascularization, and when there was no significant iridocorneal adhesion. To perform DSAEK, a Descemet stripper was used to remove the Descemet membrane and endothelium. An 8.0-mm-diameter Barron donor punch (Katena, Denville, NJ, USA) was used to cut the donor tissue from the endothelial side. The anterior chamber was formed using an anterior chamber maintainer, and the donor lamella was inserted through a 3.5-mm posterior limbal incision using the pull-through technique with a Busin glide. An air bubble was injected to unfold and attach the donor tissue to the posterior surface of the cornea.
Repeat PK was performed in the presence of significant graft scars, significant graft vascularization, and anterior chamber disorganization. The size of the recipient trephine (Hessburg–Barron suction trephine, Katena Products, Denville, NJ, USA) was selected 2.5 mm less than the vertical diameter of cornea. The recipient cornea was cut until perforation occurred. Subsequently, right and left transplantation scissors were used to completely excise the cornea. The donor tissue was punched out using a Barron donor punch (Katena Products). Donor–recipient disparity was 0.25 or 0.50 mm and the suturing technique consisted of 16 separate 10-0 nylon sutures. Subconjunctival betamethasone (4 mg) and cefazolin (100 mg) were injected at the completion of surgery in all eyes.
Postoperative course
All patients received topical 0.5% chloramphenicol 4 times a day for 15 days, topical 0.1% betamethasone 6 times a day, tapered over 6 months and maintained once daily indefinitely, and oral prednisolone 1 mg/kg/day, tapered and discontinued during 6 weeks. On postoperative day 1, the patients were randomly assigned to one of the two groups by drawing a lot. Group 1 was treated with MMF (CellCept, Roche Pharma AG, Grenzach Wyhlen, Germany) 1 g twice daily for 6 months; thereafter, they received 1 g MMF daily for the next 6 months. This regimen was devised based on the dose of the medication employed in similar studies in addition to standard protocols for renal transplantation [7,8,9,10,11]. Group 2 patients received topical 0.03% tacrolimus 4 times a day for 12 months.
The follow-up examinations were scheduled at 1 day, 7 days, 2 weeks, 1 month, and then every month thereafter, and in-between on an as-needed basis. All patients were followed up for 1 year. A complete ocular examination was performed at each follow up and the donor grafts were assessed for signs of endothelial rejection which was defined by the presence of keratic precipitates with or without graft edema in a previously clear graft. Graft edema without keratic precipitates was differentiated from graft failure by edema reversal after initiation of corticosteroids. Each episode of graft rejection was treated in the same manner using topical 0.1% betamethasone every 1 h during waking hours with its ophthalmic ointment during sleep in combination with 1 mg/kg/d oral prednisolone. Oral prednisolone was continued for 2 weeks and topical betamethasone was gradually weaned over 2 weeks after rejection reversal, which was defined as complete resolution of graft edema, keratic precipitates, and anterior chamber reaction. Persistent graft edema after 2 months of rejection episodes was considered irreversible rejection. The topical and systemic immunosuppressive drugs were discontinued at this time point.
In patients who received oral MMF, blood pressure, cell blood counts, and renal and liver function test were monitored every month during the first 3 months and then every 2 months thereafter to check for drug toxicity. Blood level monitoring of MMF was not performed.
Statistical analyses
Considering α error = 5%, power = 80%, difference in rejection rates between the two groups = 35% (based on previous reports in similar studies), the sample size was calculated to be 29 patients in each study group. SPSS statistical software version 24 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. A Kolmogorov-Smirnov test and a Q-Q plot were used to determine parameters with normal distribution. Normally distributed parameters were expressed in mean and standard deviation and compared between the study groups using Student t test. Parameters without normal distribution were presented in median and interquartile range and compared using Mann–Whitney U test. Chi-square and Fisher’s exact tests were applied to compare binomic variables. The differences between the groups were corrected for the baseline differences using binary logistic regression. The main outcome measure in this study was the rate of rejection-free graft survival which was calculated and compared between the groups using Kaplan–Meier survival curve and log-rank test, respectively. Our study design was intention-to-treat mode and the survival rates were calculated for all participants enrolled in the study. A p value <0.05 was considered statistically significant.
Results
This study enrolled a total of 63 consecutive eyes of 63 patients who were scheduled for repeat keratoplasty. Thirty-two patients randomly received systemic MMF (group 1), and topical 0.03% tacrolimus was prescribed in 31 patients (group 2). Mean patient’s age at the time of initial keratoplasty was 46.9 ± 20.2 years (range, 16–79 years) in group 1 and 46.9 ± 17.4 years (range, 16–80 years) in group 2 (P = 0.99). Mean patient’s age at the time of last keratoplasty was 54.1 ± 18.0 years (range, 20–86 years) and 51.8 ± 17.6 years (range, 18–83 years) in groups 1 and 2, respectively (P = 0.61). The study groups were balanced in the technique of repeat keratoplasty which consisted of DSAEK (9 eyes of group 1 and 13 eyes of group 2) and PK (23 eyes of group 1 and 18 eyes of group 2, P = 0.30). The surgery was keratoplasty alone in 61 patients; 1 eye of group 1 received intracapsular cataract extraction and 1 eye of group 2 had extracapsular cataract extraction and posterior-chamber intraocular lens (IOL) implantation at the time of repeated corneal transplantation. Table 1 compares baseline data between the study groups. No significant differences were found between the two study groups in patient’s sex, indication for surgery in initial keratoplasty, number of grafts per patient, history of glaucoma and herpes simplex keratitis, quadrants of corneal neovascularization, lens status prior to the last keratoplasty, and indication for last keratoplasty (Table 1). Of 40 pseudophakic eyes, 37 had a posterior-chamber IOL, whereas 1 eye of group 1 and 2 eyes of group 2 had an iris-claw anterior-chamber IOL. Intraocular pressure was controlled preoperatively in all eyes with history of glaucoma; 7 eyes (21.9%) of group 1 and 6 eyes (19.4%) of group 2 received anti-glaucoma medications preoperatively (P = 0.97). The two groups were comparable in donor characteristics including postmortem time, endothelial cell density, donor quality, and donor trephine size (Table 2).
Five patients were excluded from group 1; corneal graft melted 1 month postoperatively in one case, another patient developed corneal graft ulcer 2 months postoperatively, one had rhegmatogenous retinal detachment necessitating vitreoretinal surgery at postoperative month 6, and two cases discontinued MMF at postoperative months 2 and 6 due to gastrointestinal disturbances. Six patients withdrew from group 2; two had primary graft failure, corneal graft melted 1 month postoperatively in one case, another patient developed corneal graft ulcer 5 months postoperatively, one had rhegmatogenous retinal detachment necessitating vitreoretinal surgery at postoperative month 10, and one patient discontinued the topical tacrolimus 4 months postoperatively due to the ocular irritation (Fig. 1). None of the patients were lost for the follow-up. The underlying reason for graft melting and ulcer encountered in this cohort was abnormal graft epithelialization and not related to the medications the patients received. Primary graft failure encountered in 2 eyes was thought to be due to donor tissue characteristics.
Of the remaining cases, 11 experienced endothelial graft rejection reactions during the study period; 5 (15.6%) of group 1 and 6 (19.4%) of group 2 (P = 0.75). Table 3 presents the characteristics of the patients who developed immunologic rejection during the study. All patients in group 1 with graft rejection underwent PK, whereas in group 2, three patients received DSAEK and another three underwent PK. With the exception of one patient (case 2 in Table 3), who had two episodes of graft rejection, all others experienced only one episode of rejection. In the patient with multiple rejections, the first episode completely resolved after treatment; however, the second episode led to the graft failure. Mean time to the episode of rejection was 3.8 ± 2.6 months (range, 1–7 months) in group 1 and 5.5 ± 3.1 months (range, 2–10 months) in group 2 (P = 0.35). Three of 5 graft rejections (60%) in group 1 and 3 of 6 graft rejections (50%) in group 2 were irreversible and led to graft failure (P = 0.99), indicating nonsignificant difference between the study groups in reversibility of rejection episodes.
Rejection-free graft survival is exhibited by Kaplan–Meier survival plots in Fig. 2. The design of our study was intention-to-treat mode and the rate of rejection-free graft survival was calculated for all 63 patients. This rate was 84.4% in group 1 and 80.6% in group 2 at postoperative month 12 (P = 0.74). We also calculated the rate for patients who completed the one-year follow-up of the study (27 eyes of group 1 and 25 eyes of group 2; per-protocol analysis). This analysis shows a similar result with a rejection-free graft survival of 81.5% in group 1 and 76.0% in group 2 at postoperative month 12 (P = 0.68).
A Intention-to-treat analysis (n = 63); the rejection-free graft survival rate was 84.4% in the group that received oral mycophenolate mofetil (group 1) and 80.6% in the group that received topical 0.03% tacrolimus (group 2) 12 months after repeat keratoplasty (P = 0.74). B Per-protocol analysis (n = 52); the rejection-free graft survival rate was 81.5% in group 1 and 76.0% in group 2 at postoperative month 12 (P = 0.68).
At the last postoperative examination, BSCVA was 1.11 ± 0.79 logMAR (range, 0.28–3.0 logMAR) in group 1 and 1.17 ± 0.71 logMAR (range, 0.18–3.0 logMAR) in group 2 (P = 0.78). Postoperatively, five patients (15.6%) of group 1 and four patients (12.9%) of group 2 required medications to control intraocular pressure (P = 0.47). No significant difference was found between the study groups in preoperative and postoperative intraocular pressure (Table 4). Compared to preoperative values, we did not observe any significant increase in intraocular pressure in any study groups postoperatively (Table 4).
Premature withdrawal of the drug was judged necessary in two cases (6.3%) of group 1 after 2 and 6 months postoperatively due to gastrointestinal disturbances. No cases of group 1 had abnormal laboratory results or elevated blood pressure. In group 2, one patient (3.2%) discontinued tacrolimus after 3 months postoperatively due to eye irritation and burning sensation on drop instillation. Slit-lamp examination using diffuse light and cobalt blue light showed no signs of ocular toxic reactions, including conjunctival congestion, edema, or graft epithelial abnormalities, in any cases of group 2.
Subgroup analyses
Subgroup analyses were performed to compare the results between PK and DSAEK cases separately. Two eyes that underwent concurrent lens procedures were excluded from the subgroup analyses. The distribution of original diagnoses leading to primary corneal transplantation was not significantly different between eyes that received systemic MMF versus those that received topical 0.03% tacrolimus in the PK or DSAEK subgroup (P = 0.41 and 0.15, respectively). Similarly, no significant difference was observed between the two treatment groups regarding patient’s age, preoperative risk factors for graft rejection, rate of graft rejection, and rejection-free graft survival when the outcomes were compared in the PK and DSAEK patients separately (Tables 5 and 6). We performed post hoc power analysis to determine the study power for the detection of observed difference in rejection rates between eyes that received systemic MMF versus topical tacrolimus in each subgroup; the study power was calculated 78 and 41% in the PK and DSAEK subgroups, respectively.
Discussion
Topical and systemic corticosteroids are currently the gold standard for the prevention of corneal allograft rejection after low-risk keratoplasty because they have a good anterior chamber penetration and provide effective immunosuppression [20]. Numerous ocular adverse reactions, however, have been associated with topical steroids, including predisposition to opportunistic infections, impaired wound healing, increased intraocular pressure, and cataract formation [21]. In addition, they are not adequate to prevent immunologic rejection in patients with high-risk grafts, and the rejection rates remain unacceptably high despite frequent application of topical steroids in this population [22]. Therefore, steroid-sparing medications with less toxic side effects have been explored recently.
The rate of graft rejection in the PK subgroup of the present study (19.5%) was lower than that previously reported from our center when we had not employed immunosuppression after repeat PK (35.4%) [23]. This observation which is in line with the results of previous studies indicates that both topical and systemic immunosuppression can improve immune reaction-free graft survival following repeat keratoplasty [7,8,9,10,11, 18, 19, 24, 25]. Systemic MMF is a potent immunosuppressive agent, and several studies confirm that it considerably reduces the number of immune graft rejections in high-risk keratoplasties [7,8,9,10,11]. A systematic review of four studies (including 3 randomized clinical trials and 1 case series) which evaluated the effects of systemic MMF on the rate of graft rejection after high-risk corneal transplantation demonstrated an 89.05% rejection-free graft survival at one year with 91.7% of those episodes being reversible [26]. Similarly, in our study, the rejection-free survival rate was 84.4% at postoperative month 12 in the MMF group, but only 40% of immune reactions were successfully reversed. In addition, all patients of group 1 experienced episodes of rejection while taking systemic MMF. According to the earlier studies, an immune rejection was prevented during administration of systemic MMF, and graft rejection tended to occur after the cessation of the drug [9, 11, 24]. The less favorable effect of MMF in our cohort is due to the higher number of regrafts and the immunologic rejection as the predominant mechanism of graft failure when compared to the previously published studies.
There are limited reports of the effectiveness of topical tacrolimus in preventing rejection in high-risk grafts. Dhaliwal et al. [18] used tacrolimus eye drops in combination with topical steroids in four patients with high-risk graft and reported no new episodes of graft rejection. In addition, Magalhaes et al. [19] retrospectively compared the combination of topical 0.03% tacrolimus and 1% prednisolone to prednisolone eye drops alone in high-risk keratoplasty and reported a significantly lower rate of irreversible graft rejections in the former group (19.4%) than in the latter group (44.4%). The rate of rejection episodes, however, was comparable between the two groups (38.8% in the tacrolimus plus prednisolone group versus 61.1% in the prednisolone-alone group) [19]. In a prospectively randomized clinical trial, Reinhard et al. [25] compared topical 0.06% tacrolimus with topical corticosteroid in patients with normal-risk corneal transplants. All participants received systemic fluocortolone [25]. At postoperative month 12, all patients of the tacrolimus group were free from graft rejection reactions, in contrast to 84% of patients in the corticosteroid group [25].
We established two groups with similar high-risk characteristics and observed no remarkable differences between the MMF and tacrolimus groups in the rate of immune graft rejection and rejection reversal. These results indicate that topical 0.03% tacrolimus in combination with systemic corticosteroids can be as effective as systemic MMF in reducing the rate of endothelial graft rejection after repeat keratoplasty while not carrying the risks of systemic immunosuppressive therapy. In addition, the logistics and cost of postoperative immunosuppression are decreased with topical tacrolimus since it does not require frequent consultation with internal medicine physicians or strict laboratory monitoring of liver and renal functions. The major side effect of systemic MMF is gastrointestinal disturbances caused by the enterohepatic circulation of the drug and can lead to poor compliance [9]. This complication led to premature withdrawal of the medication in 6.3% of our patients. We did not encounter abnormal laboratory results or other reported complications, including infection, leukopenia, anemia, arterial hypertension, and hyperlipidemia. The major drawback of topical tacrolimus is ocular irritation which led to cessation of the medication in one of the cases (3.2%) in our cohort. Other reported adverse effects of topical tacrolimus, including superficial punctate keratitis, corneal epithelial erosion, and the development of slight superficial corneal haziness, were not encountered in the present study [25]. Since tacrolimus is compounded without using preservative, the local adverse reactions are likely caused by the drug itself. In their study, Reinhard et al. [25] used topical 0.06% tacrolimus, double the concentration used in our study, and reported that local side effects resulted in premature withdrawal of the drug in 40% of cases. In another study that used topical 0.03% tacrolimus, 11.1% of patients reported mild discomfort and none of them discontinued the medication due to its ocular side effects [19]. Similar to the results of previous studies, there was no increase in intraocular pressure, related to tacrolimus use, in the present study [25].
Our present study has two limitations: lack of data on the rejection rate after cessation of immunosuppression and the difference in the repeat keratoplasty technique. Theoretically, systemic MMF may induce immune tolerance that prolongs graft survival even after drug discontinuation; however, this is not the case with topical tacrolimus since it does not affect the regional lymph nodes and spleen where sensitization to corneal allograft antigens takes place. Therefore, longer follow ups are required to determine if the rate of graft rejection remains comparable between the two groups after the cessation of the medications. The fact that we chose DSAEK as a method of regrafting in some patients could undermine the validity of our study; this is partially attributable to a significantly lower rate of rejection after DSAEK compared to PK [27]. However, it should be noted that endothelial keratoplasty in high-risk setting has a guarded prognosis [28]. In addition, since DSAEK has become one of the viable options in repeat keratoplasties, it should not be looked upon as a weakness of our study but of a mere change in the trends of surgical technique worldwide. Furthermore, subgroup analyses revealed comparable outcomes between eyes that received systemic MMF and those that received topical tacrolimus in the PK and DSAEK subgroups. We recognize, however, that combining the results of the PK and DSAEK cases could reduce the validity of our findings due to different PK and DSAEK graft survivals. In addition, the results of post hoc power analysis demonstrate that the current study is not strong enough to detect differences between these two treatments in the endothelial keratoplasty group. Therefore, further studies are warranted to compare the efficacy of systemic MMF and topical 0.03% tacrolimus in preventing corneal allograft rejection after repeat keratoplasty in PK and DSAEK cases separately. These studies should determine the rejection rate after cessation of immunosuppression.
In conclusion, our results demonstrate that topical 0.03% tacrolimus in conjunction with systemic corticosteroids can be as effective as systemic MMF in reducing corneal allograft rejection up to 12 months after repeat keratoplasty, which is reflected in the fact that equal number of cases in each group developed graft rejection and eventually had graft failure.
Summary
What was known before
-
Systemic immunosuppression with mycophenolate mofetil (MMF) has been reported to be efficient and improve corneal graft prognosis considerably in high-risk grafts including repeat keratoplasty.
-
Some studies have shown the ability of tacrolimus to reduce immunologic graft rejection in human high-risk corneal transplantation.
What this study adds
-
Topical 0.03% tacrolimus in combination with corticosteroids was as effective as systemic MMF in reducing endothelial graft rejection with 12 months follow up after repeat keratoplasty.
-
This drug represents a promising alternative therapy in high-risk corneal grafts with previous history of failure.
References
Al-Mezaine H, Wagoner MD, King Khaled Eye Specialist Hospital Cornea Transplant Study Group. Repeat penetrating keratoplasty: indications, graft survival, and visual outcome. Br J Ophthalmol. 2006;90:324–7.
Thompson RW Jr, Price MO, Bowers PJ, Price FW Jr. Long-term graft survival after penetrating keratoplasty. Ophthalmology. 2003;110:1396–402.
Tan DT, Janardhanan P, Zhou H, Chan YH, Htoon HM, Ang LP, et al. Penetrating keratoplasty in Asian eyes: the Singapore Corneal Transplant Study. Ophthalmology. 2008;115:975–82.
Weisbrod DJ, Sit M, Naor J, Slomovic AR. Outcomes of repeat penetrating keratoplasty and risk factors for graft failure. Cornea. 2003;22:429–34.
Yu AL, Kaiser M, Schaumberger M, Messmer E, Kock D, Welge-Lussen U. Perioperative and postoperative risk factors for corneal graft failure. Clin Ophthalmol. 2014;8:1641–7.
Liu Y, Hamrah P, Zhang Q, Taylor AW, Dana MR. Draining lymph nodes of corneal transplant hosts exhibit evidence for donor major histocompatibility complex (MHC) class II-positive dendritic cells derived from MHC class II-negative grafts. J Exp Med. 2002;195:259–68.
Reinhard T, Mayweg S, Sokolovska Y, Seitz B, Mittelveifhaus H, Engelmann K, et al. Systemic mycophenolate mofetil avoids immune reactions in penetrating high-risk keratoplasty: preliminary results of an ongoing prospectively randomized multicentre study. Transpl Int. 2005;18:703–8.
Reis A, Reinhard T, Voiculescu A, Kutkuhn B, Godehardt E, Spelsberg H, et al. Mycophenolate mofetil versus cyclosporin A in high risk keratoplasty patients: a prospectively randomised clinical trial. Br J Ophthalmol. 1999;83:1268–71.
Birnbaum F, Mayweg S, Reis A, Bohringer D, Seitz B, Engelmann K, et al. Mycophenolate mofetil (MMF) following penetrating high-risk keratoplasty: long-term results of a prospective, randomised, multicentre study. Eye. 2009;23:2063–70.
Szaflik JP, Major J, Izdebska J, Lao M, Szaflik J. Systemic immunosuppression with mycophenolate mofetil to prevent corneal graft rejection after high-risk penetrating keratoplasty: a 2-year follow-up study. Graefes Arch Clin Exp Ophthalmol. 2016;254:307–14.
Birnbaum F, Böhringer D, Sokolovska Y, Sundmacher R, Reinhard T. Immunosuppression with cyclosporine A and mycophenolate mofetil after penetrating high-risk keratoplasty: a retrospective study. Transplantation. 2005;79:964–8.
Allison AC, Eugui EM. Mycophenolate mofetil and its mechanisms of action. Immunopharmacology. 2000;47:85–118.
Daniel E, Thorne JE, Newcomb CW, Pujari SS, Kacmaz RO, Levy-Clarke GA, et al. Mycophenolate mofetil for ocular inflammation. Am J Ophthalmol. 2010;149:423–32.
Tanaka H, Kuroda A, Marusawa H, Hashimoto M, Hatanaka H, Kino T, et al. Physicochemical properties of FK-506, a novel immunosuppressant isolated from Streptomyces tsukubaensis. Transpl Proc. 1987;19:11–16.
Shaw KT, Ho AM, Raghavan A, Kim J, Jain J, Park J, et al. Immunosuppressive drugs prevent a rapid dephosphorylation of transcription factor NFAT1 in stimulated immune cells. Proc Natl Acad Sci USA. 1995;92:11205–9.
Tamura K, Fujimura T, Iwasaki K, Sakuma S, Fujitsu T, Nakamura K, et al. Interaction of tacrolimus(FK506) and its metabolites with FKBP and calcineurin. Biochem Biophys Res Commun. 1994;202:437–43.
Joseph MA, Kaufman HE, Insler M. Topical tacrolimus ointment for treatment of refractory anterior segment inflammatory disorders. Cornea. 2005;24:417–20.
Dhaliwal JS, Mason BF, Kaufman SC. Long-term use of topical tacrolimus (FK506) in high-risk penetrating keratoplasty. Cornea. 2008;27:488–93.
Magalhaes OA, Marinho DR, Kwitko S. Topical 0.03% tacrolimus preventing rejection in high-risk corneal transplantation: a cohort study. Br J Ophthalmol. 2013;97:1395–8.
Shimazaki J, Iseda A, Satake Y, Shimazaki-Den S. Efficacy and safety of long-term corticosteroid eye drops after penetrating keratoplasty: a prospective, randomized, clinical trial. Ophthalmology. 2012;119:668–73.
McGhee CN, Dean S, Danesh-Meyer H. Locally administered ocular corticosteroids: benefits and risks. Drug Saf. 2002;25:33–55.
Young AL, Rao SK, Cheng LL, Wong AK, Leung AT, Lam DS. Combined intravenous pulse methylprednisolone and oral cyclosporine A in the treatment of corneal graft rejection: 5-year experience. Eye. 2002;16:304–8.
Zare M, Aslani M, Azimzadeh A, Esfandiari H, Valizadeh M. Indications and outcomes of repeat penetrating keratoplasty. Ir J Ophthalmol. 2011;23:44–50.
Birnbaum F, Reis A, Böhringer D, Sokolowska Y, Mayer K, Voiculescu A, et al. An open prospective pilot study on the use of rapamycin after penetrating high-risk keratoplasty. Transplantation. 2006;81:767–72.
Reinhard T, Mayweg S, Reis A, Sundmacher R. Topical FK506 as immunoprophylaxis after allongeneic penetrating normal-risk keratoplasty: a randomized clinical pilot study. Transpl Int. 2005;18:193–7.
Bali S, Filek R, Si F, Hodge W. Systemic immunosuppression in high-risk penetrating keratoplasty: a systematic review. J Clin Med Res. 2016;8:269–76.
Anshu A, Price MO, Price FW Jr. Risk of corneal transplant rejection significantly reduced with Descemet’s membrane endothelial keratoplasty. Ophthalmology. 2012;119:536–40.
Keane MC, Galettis RA, Mills RA, Coster DJ, Wiliams KA. A comparison of endothelial and penetrating keratoplasty outcomes following failed penetrating keratoplasty: a registry study. Br J Ophthalmol. 2016;100:1569–75.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Faramarzi, A., Abbasi, H., Feizi, S. et al. Topical 0.03% tacrolimus versus systemic mycophenolate mofetil as adjuncts to systemic corticosteroids for preventing graft rejection after repeat keratoplasty: one-year results of a randomized clinical trial. Eye 35, 2879–2888 (2021). https://doi.org/10.1038/s41433-020-01375-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01375-z
This article is cited by
-
Immunosuppressive Therapy for High-Risk Corneal Transplant
Current Ophthalmology Reports (2022)