Abstract
Background/Objectives
To evaluate biometric changes throughout the anterior chamber during accommodation and presbyopia using single image acquisition swept-source anterior-segment optical coherence tomography (AS-OCT).
Subject/Methods
Anterior-segment images were obtained using a new swept-source AS-OCT device (ANTERION, Heidelberg Engineering) from healthy volunteers (n = 71) across two centers in this prospective observational case series. In one image acquisition, cornea through posterior lens, including the ciliary muscle on both sides of the right eye, was imaged. Subjects undertook no accommodative effort and −1, −3, and −5 D of target vergence. Two-way repeated measures ANOVA modeling was performed for ciliary muscle measurements, lens parameters, aqueous depth (AD), and pupil diameter (PD). The first ANOVA factor was accommodative stimuli, and the second factor included age and refractive status.
Results
Maximum ciliary muscle thickness increased with accommodative stimuli (p < 0.001), while the distance from the scleral spur to the maximal point on the ciliary muscle and posterior ciliary muscle thickness (CMT2) decreased (p < 0.001–0.002). Older individuals showed no accommodative changes for ciliary muscle parameters, lens thickness, lens vault, PD, and AD (p = 0.07–0.32). Younger- and middle-aged eyes showed statistically significant accommodative structural alterations for these endpoints (p < 0.001–0.002), but with different patterns, including early loss of CMT2 contraction in middle-aged eyes. Within the middle-aged group, myopic eyes maintained better capacity for accommodative structural change.
Conclusions
Swept-source AS-OCT demonstrated multiple simultaneous anterior-segment biometric alterations in single acquisition images, including early loss of posterior ciliary muscle function and better maintained capacity for anterior-segment structural change in myopia.
Similar content being viewed by others
Introduction
Accommodation refers to the process where the eye changes the crystalline lens’s shape and optical power to maintain a clear image of objects at various viewing distances. When people become older, they experience presbyopia, which is defined as the point when the physiological age-related reduction in the eye’s focusing range reaches a level such that clarity at near is insufficient [1].
Multiple hypotheses exist for how the eye accommodates and presbyopia arises [2]. Critical anatomical structures include the ciliary muscle and phakic lens. In vitro studies have shown age-related changes to the ciliary muscle [3]. Nonhuman primate research has used a mid-brain stimulation model that allows for controllable and reproducible accommodation and disaccommodation that was then assessed by goniovideographic imaging [4,5,6]. Overall, these findings supported Helmholtz theory of accommodation [7] in which circumferential ciliary muscle contraction leads to a relaxation of lens zonules and rounding up of the lens to increase refractive power. In live humans, accommodation research has utilized different imaging modalities such as Scheimpflug slit lamp camera systems [8], magnetic resonance imaging [9], ultrasound biomicroscopy (UBM) [10], and optical coherence tomography (OCT) [11,12,13,14,15,16,17,18,19,20,21,22].
UBM and OCT have been particularly important for studying the anterior segment and accommodation. However, each has limitations. UBM requires ocular contact and thus a highly skilled technician. UBM is incapable of imaging the entire anterior segment (from cornea epithelium to posterior lens capsule and including the ciliary muscle on both sides of the eye) in one capture. Alternatively, anterior-segment OCT (AS-OCT) is noninvasive and provides higher resolution imaging [23,24,25,26]. However, OCT technology also has limitations. Time-domain OCT is slow with lower resolution, and while spectral-domain OCT improved resolution and speed, there is a loss of imaging depth due to the shorter-wavelength light source. Since each imaging modality has weaknesses, accommodation research in human subjects has often combined imaging from multiple devices or modalities to nonconcurrently acquire data about different parts of the accommodative apparatus at different times. Simultaneous high-resolution imaging of the entire accommodative process in live subjects from one device has not been performed.
In this study, we hypothesize that multiple parts anterior segment can be simultaneously assessed to discover new mechanistic aspects of accommodation and presbyopia. We utilize a novel swept-source AS-OCT that combines a longer wavelength light source (~1300 nm), fast imaging speed, and image averaging to improve visualization of anterior-segment structures from the cornea to the posterior lens capsule and the ciliary muscle on both sides of the eye. We use this device to conduct a prospective observational study and compare morphologic changes in the accommodative apparatus in response to stepwise accommodative stimuli in healthy adults over a range of ages and refractive status.
Methods
Study design
Healthy volunteers were recruited at University of California, Los Angeles (UCLA) and University of Southern California (USC). This study followed the tenets of the Declaration of Helsinki and was approved the USC (#HS-17-00684) and UCLA (#19-000621) IRBs. All participants signed informed consent. Inclusion criteria were: an ocular examination within three months prior to enrollment, having no ocular pathology, and having best-corrected distance visual acuity of at least 20/25. Exclusion criteria included a history of ocular trauma/surgery. Only the right eye of each participant was included. Objective refraction was obtained using a KR-1W Wave-Front Analyzer (Topcon Group, Tokyo, Japan), and subjective refraction was subsequently determined. Contact lens use was stopped one day prior to imaging.
AS-OCT imaging protocol
Images were obtained using a new swept-source AS-OCT (ANTERION, Heidelberg Engineering GmbH, Heidelberg, Germany, software v.1.2). The ANTERION has been shown to provide biometric measurements of superficial and deep ocular structures including the ciliary body and full lens thickness from single images with excellent measurement repeatability and reproducibility [27, 28]. Images were obtained in dark ambient lighting (0.02 lx at the imaging plane) by a trained ophthalmologist (XX) following a standardized imaging protocol. Subjects were positioned using a combined head and chin rest for primary gaze. Subjects were instructed to fixate on an internal fixation target while making it as clear as possible with the left eye occluded. The right eye was imaged in a relaxed state by applying the spherical equivalent refraction using an internal lens system (range: −15 to +15 D [D = diopters], ±0.5 D increments). Additional acquisitions were acquired after adjusting the internal lens system to be at −1, −3, and −5 D target vergence from the relaxed state to simulate 1, 3, and 5 D of required accommodation. Acquisition parameters were wavelength: 1300 µm; A-scan rate: 50,000 Hz; resolution in tissue: <10 μm axially × 30 μm laterally; scan pattern: radial scan; number of B-scans: 6; number of A-scans per B-scan: 768; scan length: 16.5 mm; and scan depth: 14 ± 0.5 mm. Images were tracked using the cornea light reflex, centered on the corneal vertex, for image averaging (6 B-scans averaged). After image acquisition, examination quality was assessed by in-built software based on the following endpoints: blinking, motion, fixation, tear-film irregularity, refraction correction, tracking, and imaging segmentation. If a result of “pass” was not obtained for any of the above, the acquisition was repeated.
AS-OCT image post processing and data analysis
AS-OCT images from the horizontal meridian and across the corneal vertex were analyzed. Measurements for pupil diameter (PD), lens thickness, and aqueous depth (AD) were automatically provided by the device. For lens vault measurements, investigators (XX and GC) masked to the condition marked the temporal and nasal scleral spurs on the image for the software to provide values.
For ciliary muscle, all measurements were manual. The first step was to segment the scleral–ciliary muscle tissue boundary by extending the posterior cornea segmentation line using internal software. The swept-source AS-OCT applied Snell’s law using the relative indices of refraction for the anterior and posterior corneal surfaces and at the iris and lens surfaces at 1300 µm to correct the OCT image. In addition, the changing speed of light within tissue was accounted for by appropriate scaling of sections of the A-scan according to the refractive index. Then, CMTMAX (maximum ciliary muscle thickness; the distance of a line between the maximum ciliary muscle apex to the scleral–ciliary muscle border that is perpendicular to this border), SSMAX (the distance between the scleral spur to the maximum ciliary muscle apex), and CMT2 (ciliary muscle thickness 2 mm posterior to the scleral spur) were manually measured by graders (XX and GC) masked to the conditions, as previously described [14,15,16, 18, 22, 29,30,31].
Statistical analysis
Given that presbyopia is widely known to begin in middle age, subjects were divided into three groups (young: 20–40 [n = 31]; middle: 41–60 [n = 28]; and old: >60 years of age [n = 12]). Power analysis (85% power at 0.05 alpha; based on ciliary muscle contractile velocity across age groups [32]) predicted needing ~10 subjects per group. Sample was then expanded in some cases to better study refraction within an age group. Refractive status was defined as (hyperopia [spherical equivalent]: +0.50 D and greater; emmetropia: −0.50 D to +0.25 D; and myopia: −0.75 D and greater). Statistical analyses were performed using SPSS (SPSS for Windows, v. 26.0, IBM-SPSS, Chicago, IL). The assumption of the normal distribution for continuous parameters was checked using the Shapiro–Wilk’s W test, while homogeneity of variance was examined using Levene’s test.
The difference in ciliary muscle thickness (CMTMAX, SSMAX, and CMT2) was assessed for both accommodative demand and location (nasal vs. temporal) using a two-way repeated-measurement ANOVA model. Both temporal/nasal aspects and four accommodative step stimuli (relaxed, −1.0, −3.0, and −5.0 D) were analyzed as within-subject factors. Greenhouse–Geisser correction was applied wherever the sphericity assumption was violated.
The differences in each mean parameter (CMTMAX, SSMAX, CMT2, lens thickness, lens vault, AD, and PD) were also compared across four accommodation levels to each of the following factors to determine their influence on the relationship using a two-way repeated-measurement ANOVA model: (a) age (three groups: 20–40, 41–60, and >60 years) and (b) refractive status (three groups: hyperopia, emmetropia, and myopia). These factors were analyzed as fixed effects between-subject factors, while accommodative stimuli (relaxed, −1.0, −3.0, and −5.0 D) were analyzed as a within-subjects factor. Greenhouse–Geisser correction was applied whenever the sphericity assumption was violated. Furthermore, the interaction effects between (a) age and (b) refraction with accommodative stimuli were also tested in each model. Post hoc tests with Bonferroni correction within each model were performed to detect potential subgroup differences based on the model estimates. p < 0.05 was considered statistically significant.
Results
This prospective observational study included 71 healthy and phakic volunteers (33 females and 38 males) between 23 and 74 years of age (median [quartiles]; 41 [23–74]). Swept-source OCT imaging of the anterior segment of the eye undergoing accommodation was performed, simultaneously showing the iris, PD, AD, lens vault, lens thickness, and ciliary muscle (Fig. 1). Both nasal and temporal sides of the anterior chamber and ciliary muscle could be simultaneously visualized (Fig. 1). In a younger eye (34-year-old male), multiple structural changes were observed during accommodation. Qualitatively, the ciliary muscle expanded inward and anterior, the lens became thicker, the lens shifted anterior, and the pupil underwent miosis (Clip 1). In an older eye (63-year-old male) these changes were less apparent (Clip 2).
Anterior-segment anatomy with scleral spur (SS; yellow dots), angle recess (red dots); AD aqueous depth (distance from posterior cornea to anterior lens capsule); PD pupil diameter; LV lens vault (the perpendicular distance between the anterior pole of the crystalline lens to a horizontal line joining the two scleral spurs); and LT lens thickness. The insert focuses on the ciliary muscle: CMTMAX ciliary muscle thickness at the point of maximum thickness, SSMAX distance between scleral spur and the thickest point of the ciliary muscle, CMT2 distance between ciliary muscle to a perpendicular point on the ciliary muscle and scleral border that is 2 mm posterior to the scleral spur. Scale bar: 1000 µm.
Age-related ciliary muscle changes during accommodation
Focused on the ciliary muscle, CMTMAX is an endpoint for anterior ciliary muscle contraction, SSMAX is an endpoint for ciliary muscle anterior displacement, and CMT2 is an endpoint for posterior ciliary muscle contraction. Results from two-way repeated measures ANOVAs with factors of both ciliary muscle location and accommodative stimulus showed that both the nasal and temporal CMTMAX increased with increasing accommodation (Table 1; ap < 0.001). SSMAX decreased (or the muscle shifted anteriorly) with increasing accommodation (Table 1; ap < 0.001). Posterior ciliary muscle thickness also decreased with increasing accommodation (Table 1; ap < 0.001–0.002). The changes in ciliary muscle across accommodation were comparable for both sides (Table 1; bp = 0.53–0.98).
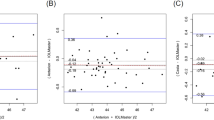
CMTMAX thickening, SSMAX decreasing, and CMT2 decreasing over accommodation were individually different across the three age groups (Table 2; bp < 0.001, bp < 0.001, bp = 0.04, respectively). There was no statistically significant change in any of the ciliary muscle parameters within the older-aged group (Table 2; ap = 0.07–0.35). For younger- and middle-aged groups, ciliary muscle changes were seen but with differences. CMTMAX thickness increased significantly with increasing accommodation (Table 2; both ap < 0.001), while SSMAX distance decreased significantly (Table 2; both ap < 0.001). In terms of CMTMAX thickening, post hoc pairwise comparisons showed statistically significant differences between each accommodative step in the younger-aged group (all p < 0.001) while the thickening in the middle-aged group reached a plateau at 3 D (p < 0.001–0.002), as the difference in CMTMAX at 3 and 5 D was not statistically significant (p = 1.0). In terms of SSMAX decreasing, post hoc analysis showed statistically significant differences between each accommodative step in the younger-aged group (all p < 0.001) while the decrease in the middle-aged group reached a plateau at 3 D (p = 0.001–0.005), and the difference in SSMAX at 3 and 5 D was not statistically significant (ap = 1.0). CMT2 thickness decreased significantly with increasing accommodation in the younger-aged group (Table 2; p < 0.001). Statistically significant differences were seen between each accommodative step in the younger-aged group (all p < 0.001). In contrast, no overall change and no unidirectional trend was seen for CMT2 in the middle-aged group (Table 2; ap = 0.08).
Age-related nonciliary muscle changes during accommodation
Other components of the anterior segment are known to change during accommodation so that AD, lens thickness, lens vault, and PD were simultaneously evaluated as well. Similar to the ciliary muscle, there was no statistically significant change in any of these parameters over accommodation in the older-aged group (Table 3; ap = 0.13–0.32). For younger- and middle-aged groups, accommodative effort led to a reduction in AD and PD with an increase in lens thickness and lens vault (Table 3), but subtle differences existed.
Lens thickness and lens vault increased significantly with increasing accommodation in both younger- and middle-aged groups (Table 3; both ap < 0.001–0.002). Statistically significant differences were seen between each accommodative step in the younger-aged group (all p < 0.001) while the lens thickness and vault increase in the middle-aged group reached a plateau at 3 D (p = 0.001–0.04), and the differences in lens thickness (p = 1.0) and vault (p = 0.6) at 3 and 5 D were not statistically significant.
AD and PD decreased significantly with increasing accommodation in both younger- and middle-aged groups (Table 3; both ap < 0.001–0.001). Statistically significant differences were seen between each accommodative step in the younger-aged group (p < 0.001–0.001) while the AD and PD decrease in the middle-aged group reached a plateau at 3 D (p = 0.001–0.02), and the differences in AD and PD between 3 and 5 D were not statistically significant (both p = 1.0).
Refraction-related ciliary muscle changes during accommodation in the middle-aged group
Further analyses were performed solely in the middle-aged group (given that this is when presbyopia occurs) across refractive status. There was no statistically significant change in any of the ciliary muscle parameters over accommodation for the hyperopic cohort (Table 4; ap = 0.20–0.83). Focused on the emmetropic and myopic groups, CMTMAX thickness increased (both ap < 0.001), and SSMAX distance decreased (Table 4; ap = 0.005 and <0.001, respectively) significantly with increasing accommodation. For CMTMAX, post hoc pairwise comparisons showed statistically significant differences between accommodative steps for both groups (emmetropia: [0–1 D] p < 0.001, [1–3 D] p = 0.03; and myopia: [0–1 D] p < 0.001, but not [1–3 D] p < 0.07). The differences in CMTMAX at 3 and 5 D were not statistically significant for either group (emmetropia: p = 0.15; and myopia: p = 1.0). For SSMAX, post hoc pairwise comparisons showed statistically significant differences between the 0 and 1 D accommodative step in both groups (emmetropia: p < 0.001; and myopia: p < 0.001). The differences between 1 and 3 D (emmetropia: p = 0.15; and myopia: p = 0.12) and between 3 and 5 D (both: p = 1.0) were not statistically significant. CMT2 thickness decreased significantly with increasing accommodation in the myopic but not the emmetropic group (Table 4; ap = 0.005 and 0.53, respectively).
Refraction-related nonciliary muscle changes during accommodation in the middle-aged group
For nonciliary muscle parameters, no statistically significant change was seen in the middle-aged hyperopic group (Table 4; ap = 0.07–0.16). However, statistically significant changes among all of these parameters were seen in the middle-aged myopic group (Table 4; ap < 0.001–0.04). For the middle-aged emmetropic group, some of the alterations were significantly different (Table 4; lens thickness: ap = 0.04 and PD: ap = 0.001) but others were borderline or not (Table 4; AD: ap = 0.05 and lens vault ap = 0.06).
Discussion
The results of this study supported Helmholtz’s theory of accommodation [2, 7] with additional findings. Swept-source OCT allowed simultaneous assessment of the entire anterior segment in individual B-scans of healthy human volunteers. The ciliary muscle (nasal and temporal) was noted to show an inward contraction and anterior shift (Clip 1 and Table 1). These alterations diminished with age (Clip 2 and Table 2). Simultaneously, decreased AD and decreased pupil constriction with increased lens thickness and increased lens vault were seen with increasing age (Table 3). Separately, posterior ciliary muscle contraction was lost earlier, compared to other parts of the ciliary muscle (Table 2). Loss of CMT2 contraction may thus be an early presbyopia biomarker. To confirm this, future studies will need to test a larger sample, longitudinally.
The issue of diminishing ciliary muscle function with age is also clinically important. Accommodative multifocal intraocular lenses presume a functioning ciliary muscle in old age to allow for forward shift of the pseudophakic lens during postoperative accommodative effort [33]. The literature describes maintained ciliary muscle contraction with age, and this is often used to argue for a lenticular cause of presbyopia (lens hardening) as opposed to a muscular cause (ciliary muscle weakening) [12, 13, 16]. In our results, no significant changes to ciliary muscle endpoints, AD, or lens parameters were noted in the older-aged cohort during attempted accommodation. At most, a trend toward initial CMTMAX thickening and SSMAX/CMT2 thinning from baseline to 1 D of attempted accommodation was seen, but this did not continue at higher levels of demand. Then, middle-aged eyes showed statistically significant changes in all of the parameters but mostly at lower accommodative effort, while younger eyes showed statistically significant changes for all parameters between all accommodative steps. It is important to note that “older subjects” in the OCT-based literature were mostly less than 60 years of age, and included at most 0–4 subjects per study [12, 13, 16]. Thus, our middle-aged cohort better matched “older subjects” in the literature, and our results agree that individuals less than 60 years of age maintain some accommodative ability. However, for even older individuals, our results suggest lesser benefit of accommodative multifocal IOLs such that evaluation of ciliary muscle function before surgery should be performed to identify patients who can benefit.
The result of diminished pupil response in the older-aged cohort is also interesting. The “near triad” is a combination of accommodation, convergence, and miosis [34]. Most theories for presbyopia focus solely on end organs (ciliary muscle and lens). However, the simultaneous lack of miosis and ciliary muscle contraction in older subjects in this report raises the hypothesis that age-related loss of CNS neurological output could also contribute to presbyopia. To study this, a longitudinal investigation over a timeframe where presbyopia is occurring will be required.
The result of maintained accommodative anterior-segment anatomical changes in the myopic middle-aged cohort is also interesting, although based on a small sample size. Comparing the emmetropic to myopic cohorts, while some of the same accommodative ciliary muscle alterations were seen, the emmetropic group lost CMT2 contraction, while the myopic group did not (Table 4). Further, the emmetropic group lost alterations to the lens which is ultimately what changes the direction of light during accommodation. First, this result continues to support a lenticular cause of presbyopia as lens change was lost despite continued muscular activity. Further, it puts forth the hypothesis that myopes are mechanistically less impacted by presbyopia. To speculate, previously described thicker anterior and posterior ciliary muscle in myopia [35,36,37] has been of unclear functional significance, and it is possible that it represents a more enduring muscle that can resist age-related lenticular changes.
Several limitations exist in this study. First, we relied upon subjects to accommodate upon request. Compliance with instructions could not be assessed. Future studies could use pharmacological stimulation [17, 19, 38, 39] to avoid subject cooperation. Also, nonsignificant results with p values suggestive of trends were seen in some cases (older individuals and in the refractive analyses) where increased sample could have increased power. However, the results demonstrated strong biological plausibility. For example, for all accommodative endpoints (Tables 2 and 3), changes were statistically significant between all accommodative steps in the young-aged cohort, only statistically significant in the early (0–3 D) but not in the later (3–5 D) steps in the middle-aged cohort, and overall nonsignificant in the older-aged cohort. For the older-aged cohort, lack of accommodative structural change is expected since presbyopia is defined by the loss of accommodation at old age [1]. Lastly, as the original intent of the research was to evaluate accommodation across a distribution of ages, we did not achieve simultaneous wide distribution of ages with an even distribution of refractive error. Thus, conclusions regarding refractive error were only available for the middle-aged cohort with smaller sample sizes. Fortunately, this is the age group where presbyopia becomes most noticeable.
In conclusion, swept-source AS-OCT with image tracking and image averaging capability allows for anterior-segment imaging that is particularly useful for studying accommodation. Future research should be directed at identifying those most prone to early presbyopia, identifying those who have a chance to benefit from accommodative IOLs, and helping to develop OCT-based anatomical endpoints for innovating presbyopia treatments.
Summary
What was known before
-
Nonsimultaneous imaging of different parts of the anterior segment has supported Helmholtz’s theory of accommodation.
-
However, this approach is limited because different methods are being used while imaging different parts of the eye at different times.
-
Simultaneous visualization of accommodation across the superficial and deep anterior chamber has not been performed.
What this study adds
-
Swept-source AS-OCT approaches allow for simultaneous assessment of superficial and deep aspects of accommodation. This has allowed for two new findings.
-
Loss of posterior ciliary muscle contraction may be an early biomarker of presbyopia.
-
Anterior-segment accommodation structural alterations are better maintained in myopic eyes.
References
Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–43.
Glasser A, Kaufman PL. The mechanism of accommodation in primates. Ophthalmology. 1999;106:863–72.
Tamm S, Tamm E, Rohen JW. Age-related changes of the human ciliary muscle. A quantitative morphometric study. Mech Ageing Dev. 1992;62:209–21.
Lütjen-Drecoll E, Tamm E, Kaufman PL. Age-related loss of morphologic responses to pilocarpine in rhesus monkey ciliary muscle. Arch Ophthalmol. 1988;106:1591–8.
Croft MA, Glasser A, Heatley G, McDonald J, Ebbert T, Dahl DB, et al. Accommodative ciliary body and lens function in rhesus monkeys, I: normal lens, zonule and ciliary process configuration in the iridectomized eye. Investig Ophthalmol Vis Sci. 2006;47:1076–86.
Crawford K, Terasawa E, Kaufman PL. Reproducible stimulation of ciliary muscle contraction in the cynomolgus monkey via a permanent indwelling midbrain electrode. Brain Res. 1989;503:265–72.
von Helmholtz H. Mechanism of accommodation. In: Southall J, editor. Helmholtz’s treatise on physiological optics. New York: Optical Society of America; 1924. p. 382–415.
Koretz JF, Cook CA, Kaufman PL. Accommodation and presbyopia in the human eye. Changes in the anterior segment and crystalline lens with focus. Investig Ophthalmol Vis Sci. 1997;38:569–78.
Strenk SA, Strenk LM, Guo S. Magnetic resonance imaging of the anteroposterior position and thickness of the aging, accommodating, phakic, and pseudophakic ciliary muscle. J Cataract Refract Surg. 2010;36:235–41.
Glasser A, Croft MA, Brumback L, Kaufman PL. Ultrasound biomicroscopy of the aging rhesus monkey ciliary region. Optom Vis Sci. 2001;78:417–24.
Esteve-Taboada JJ, Domínguez-Vicent A, Monsálvez-Romín D, Del Águila-Carrasco AJ, Montés-Micó R. Non-invasive measurements of the dynamic changes in the ciliary muscle, crystalline lens morphology, and anterior chamber during accommodation with a high-resolution OCT. Graefes Arch Clin Exp Ophthalmol. 2017;255:1385–94.
Domínguez-Vicent A, Monsálvez-Romín D, Esteve-Taboada JJ, Montés-Micó R, Ferrer-Blasco T. Effect of age in the ciliary muscle during accommodation: sectorial analysis. J Optom. 2019;12:14–21.
Richdale K, Sinnott LT, Bullimore MA, Wassenaar PA, Schmalbrock P, Kao CY, et al. Quantification of age-related and per diopter accommodative changes of the lens and ciliary muscle in the emmetropic human eye. Investig Ophthalmol Vis Sci. 2013;54:1095–105.
Bailey MD. How should we measure the ciliary muscle? Investig Ophthalmol Vis Sci. 2011;52:1817–8.
Sheppard AL, Davies LN. In vivo analysis of ciliary muscle morphologic changes with accommodation and axial ametropia. Investig Ophthalmol Vis Sci. 2010;51:6882–9.
Sheppard AL, Davies LN. The effect of ageing on in vivo human ciliary muscle morphology and contractility. Investig Ophthalmol Vis Sci. 2011;52:1809–16.
Mohamed Farouk M, Naito T, Shinomiya K, Mitamura Y. Observation of ciliary body changes during accommodation using anterior OCT. J Med Investig. 2018;65:60–3.
Lossing LA, Sinnott LT, Kao CY, Richdale K, Bailey MD. Measuring changes in ciliary muscle thickness with accommodation in young adults. Optom Vis Sci. 2012;89:719–26.
Kuchem MK, Sinnott LT, Kao CY, Bailey MD. Ciliary muscle thickness in anisometropia. Optom Vis Sci. 2013;90:1312–20.
Wagner S, Zrenner E, Strasser T. Emmetropes and myopes differ little in their accommodation dynamics but strongly in their ciliary muscle morphology. Vis Res. 2019;163:42–51.
Ruggeri M, de Freitas C, Williams S, Hernandez VM, Cabot F, Yesilirmak N, et al. Quantification of the ciliary muscle and crystalline lens interaction during accommodation with synchronous OCT imaging. Biomed Opt Express. 2016;7:1351–64.
Shao Y, Tao A, Jiang H, Mao X, Zhong J, Shen M, et al. Age-related changes in the anterior segment biometry during accommodation. Investig Ophthalmol Vis Sci. 2015;56:3522–30.
Huang AS, Belghith A, Dastiridou A, Chopra V, Zangwill LM, Weinreb RN. Automated circumferential construction of first-order aqueous humor outflow pathways using spectral-domain optical coherence tomography. J Biomed Opt. 2017;22:66010.
Hau SC, Papastefanou V, Shah S, Sagoo MS, Restori M, Cohen V. Evaluation of iris and iridociliary body lesions with anterior segment optical coherence tomography versus ultrasound B-scan. Br J Ophthalmol. 2015;99:81–6.
Ang M, Baskaran M, Werkmeister RM, Chua J, Schmidl D, Dos Santos VA, et al. Anterior segment optical coherence tomography. Prog Retin Eye Res. 2018;66:132–56.
Asrani S, Sarunic M, Santiago C, Izatt J. Detailed visualization of the anterior segment using fourier-domain optical coherence tomography. Arch Ophthalmol. 2008;126:765–71.
Xie X, Corradetti G, Song A, Pardeshi A, Sultan W, Lee JY, et al. Age- and refraction-related changes in anterior segment anatomical structures measured by swept-source anterior segment OCT. PLoS ONE. 2020;15:e0240110.
Pardeshi AA, Song AE, Lazkani N, Xie X, Huang A, Xu BY. Intradevice repeatability and interdevice agreement of ocular biometric measurements: a comparison of two swept-source anterior segment OCT devices. Transl Vis Sci Technol. 2020;9:14.
Pucker AD, Sinnott LT, Kao CY, Bailey MD. Region-specific relationships between refractive error and ciliary muscle thickness in children. Investig Ophthalmol Vis Sci. 2013;54:4710–6.
Wagner S, Zrenner E, Strasser T. Ciliary muscle thickness profiles derived from optical coherence tomography images. Biomed Opt Express. 2018;9:5100–14.
Buckhurst H, Gilmartin B, Cubbidge RP, Nagra M, Logan NS. Ocular biometric correlates of ciliary muscle thickness in human myopia. Ophthalmic Physiol Opt. 2013;33:294–304.
Lockhart TE, Shi W. Effects of age on dynamic accommodation. Ergonomics. 2010;53:892–903.
Alió JL, Alió Del Barrio JL, Vega-Estrada A. Accommodative intraocular lenses: where are we and where we are going. Eye Vis. 2017;4:16.
Digre KB. Assessment of accommodation, convergence and the near response. In: Miller NR, Newman NJ, editors. Walsh and Hoyt’s clinical neuro-ophthalmology. Philadelphia: Lippincott Williams and Wilkins; 2005. p. 726–8.
Muftuoglu O, Hosal BM, Zilelioglu G. Ciliary body thickness in unilateral high axial myopia. Eye. 2009;23:1176–81.
Bailey MD, Sinnott LT, Mutti DO. Ciliary body thickness and refractive error in children. Investig Ophthalmol Vis Sci. 2008;49:4353–60.
Oliveira C, Tello C, Liebmann JM, Ritch R. Ciliary body thickness increases with increasing axial myopia. Am J Ophthalmol. 2005;140:324–5.
Koeppl C, Findl O, Kriechbaum K, Drexler W. Comparison of pilocarpine-induced and stimulus-driven accommodation in phakic eyes. Exp Eye Res. 2005;80:795–800.
Tabernero J, Chirre E, Hervella L, Prieto P, Artal P. The accommodative ciliary muscle function is preserved in older humans. Sci Rep. 2016;6:25551.
Acknowledgements
This study was supported by China Scholarship Council Grant (#201808110001), Capital Characteristic Clinic Project of Beijing (Z18110000171808) [XX]. AGS MAPS Award (BYX); NIH NEI R01EY030501 [ASH] and K23EY029763 [BYX]; Research to Prevent Blindness Career Development Award 2016 [ASH]; and an unrestricted grant from Research to Prevent Blindness [UCLA and USC]. The sponsor or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
XX was responsible for experimental design, data acquisition, data analyses, creation of figures/tables, and preparation of the manuscript. WS was responsible for data analyses, creation of figures, and preparation of the manuscript. GC was responsible for experimental design, data acquisition, data analyses, and preparation of the manuscript. JYL was responsible for data analyses and preparation of the manuscript. AS and AP were responsible for data acquisition and preparation of the manuscript. FY was responsible for statistical analyses. VC was responsible for data analyses and preparation of the manuscript. SRS, BYX, and ASH were responsible for experimental design, data analyses, and preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
ASH and BYX were loaned the ANTERION from Heidelberg Engineering for the purpose of research. ASH, SRS, and BYX received research support from Heidelberg Engineering.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xie, X., Sultan, W., Corradetti, G. et al. Assessing accommodative presbyopic biometric changes of the entire anterior segment using single swept-source OCT image acquisitions. Eye 36, 119–128 (2022). https://doi.org/10.1038/s41433-020-01363-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01363-3