Abstract
The treatment of neovascular AMD (nAMD) has been revolutionized by the introduction of anti-vascular endothelial growth factor (VEGF) agents. Though, there is a tremendous gap between the outcomes in randomized clinical trials and real-world settings, where long-term outcomes are not as good as expected. This is due to undertreatment, i.e., fewer injection and low monitoring frequency. Treatment burden due to frequent injections remains a major limitation. Long-lasting treatments provide promising solutions for this unmet need by achieving better results with less mandatory injections. This review aims to cover the current state in this field and also discuss the mechanism of action, data from pivotal trials, and safety profile of long-acting treatments in present and future, going into details about the following agents: Brolucizumab, Faricimab, Abipicar, and Conbercept.
摘要
抗血管内皮生长因子 (VEGF) 药物的应用使新生血管性AMD (nAMD) 的治疗发生了革命性变化。但随机临床试验的结果与现实世界存在巨大差距, 临床实际的长期疗效远低于预期。这是由于治疗不足所致, 即注射次数较少以及随访频率低。其中频繁注射造成的治疗负担为主要的制约因素。而长效制剂通过减少注射次数以及获得的更好疗效, 为满足临床上述的需求提供了解决方案。本综述旨在阐述该领域的现状, 讨论长期治疗在目前和未来阶段的作用机制、重要临床试验数据和安全性, 并详细介绍以下药物: Brolucizumab、Faricimab、Abipicar和Conbercept。
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the leading cause of vision loss in people over 50 years of age in developed countries [1]. Severe visual loss due to AMD is caused by the advanced forms of the disease: geographic atrophy secondary to non-neovascular AMD and neovascular AMD (nAMD) [2]. It is estimated that 15 million (85–90% of all AMD patients) currently have non-neovascular AMD and 1.7 million (10–15% of all AMD patients) have nAMD. An estimated 200,000 new cases of wet AMD develop each year in the US [3]. Choroidal neovascularization in AMD is driven mainly by vascular endothelial growth factor (VEGF), a diffusible cytokine that promotes angiogenesis and vascular permeability and also promotes disease progression leading to macular oedema and vision loss. Based on this concept, anti-VEGF therapy has become the primary treatment option for nAMD. Intravitreal anti-VEGF injections of ranibizumab, bevacizumab, and aflibercept are the current treatment for nAMD. These agents have been shown to be safe and efficacious, leading to improvement in retinal anatomy and preservation of vision [4, 5]. However, a high proportion of patients lose sight in the longer term (>4 years) and are unable to read and drive, mainly due to development of macular fibrosis and atrophy [6,7,8,9,10]. Post hoc analysis of the CATT study has shown that follow-up clinic visit adherence plays an important role in visual outcomes [11]. Moreover, undertreatment and noncompliance in real-world settings lead to visual outcomes that fall far short of randomized clinical trials (RCTs) [12]. Patients in real life settings do not comply with mandatory follow-up visits and might miss appointments and injections [13]. Loss to follow-up, i.e., receipt of one or more injections with no subsequent follow-up visit within 12 months, was reported in 22% of patients in real-world studies [14, 15]. There are a myriad of limitations in the current treatment of nAMD. The first is related with the drugs themselves, i.e., high costs to health systems and patient affordability, lack of accessibility, insufficient response, high treatment burden due to short duration of action of existing drugs, and need for monthly loading. The second is related with the current treatment regimens [fixed, treat and extend, and pro re nata]. While we may be overtreating part of the patients, others might be undertreated—both situations might lead to visual loss. To date, there is not enough information available to guide customized treatment with anti-VEGF. The last limitation is related to the patient: low adherence to frequent injections and missed injections due to comorbidities, patient perception, anxiety and discomfort, financial burden, lack of transportation etc. As has been pointed out in Goodman and Gilman’s Pharmacological Basis of Therapeutics [16], the best drug to treat any disease, such as nAMD, is an agent which might be administered once without any side effects and cure the disorder in the first treatment. We do not have such a drug yet, but science is on track by performing clinical trials to find long-acting treatments for nAMD. New agents for nAMD might offer the potential to improve treatment outcomes and reduce treatment burden associated with current therapy. This review aims to introduce the new promising drugs for treatment of nAMD, explain their mechanism of action, summarize pivotal trials results, discuss potential limitations and safety profile for brolucizumab, abipicar, faricimab, and conbercept.
Brolucizumab
The drug
Brolucizumab, also known as RTH258 (Beovu®; Novartis), is a humanized single-chain antibody fragment approved in October 2019 by the US Food and Drug Administration (FDA) for the treatment of nAMD [17]. It is considered the smallest subunit of an antibody for treatment in medicine tested for human use, with a molecular weight of ~26 kD. The primary molecular interaction of this substance consists of inhibiting VEGF-A binding to VEGF receptors VEGFR1 and VEGFR2 [18]. Its small molecular size and the absence of the crystallizable fragment provide amplified bioavailability and reduction of immunogenicity with better tissue penetration, more sustained effect, and less systemic exposure with the potential consequent decrease in adverse effects compared to full-size antibodies [19]. The molecule can be concentrated in a smaller amount of net liquid volume, allowing to supply 6 mg of brolucizumab in as little as 50 μl for intravitreal injection, which means eleven times higher than aflibercept [20].
Preclinical data has shown higher penetration of the drug through the retina, and the retinal pigment epithelium compared to ranibizumab, hinting that brolucizumab might provide better control over all retinal layers and decrease fluid in all retinal compartments [19]. The phase 2 OSPREY study showed that brolucizumab was as efficacious as aflibercept at 8 and later at 12 weeks intervals providing the base for phase 3 clinical trials [21].
Pivotal trials
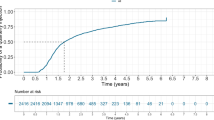
The HAWK and HARRIER clinical trials were two similarly designed phase 3 trials comparing brolucizumab with aflibercept in the treatment of nAMD. Both were double-masked, multicenter, active-controlled, randomized trials. After three initial monthly injections, the frame interval was modified to every 8 and weeks in the HAWK and every 12 weeks in the HARRIER trial. HAWK utilized brolucizumab at 3 mg and 6 mg dosing, and HARRIER only at 6 mg dosing. Patients on the aflibercept group received a fixed 2 mg dose at 8 weeks interval. Both studies showed good results in the brolucizumab groups with reduction in intraretinal fluid and subretinal fluid compared to aflibercept at time points of 16, 48, and 96 weeks. Regarding best-corrected visual acuity (BCVA), brolucizumab showed noninferiority vs. aflibercept. More than 50% of the patients in both trials were able to maintain a 12-week scheduling interval with brolucizumab [22, 23].
Safety profile
Intraocular inflammation (IOI) was seen in 5.3% and 2.7% in HAWK and HARRIER, respectively. In the aflibercept group, only <1% presented evidence of IOI. A total of 6/730 patients (0.82%) presented retinal arterial occlusions in the brolucizumab 6 mg group. Post marketing, eleven more cases of occlusive retinal vasculitis were reported [23]. By March 2020, twenty-seven cases were reported by the American Society of Retina Specialists Research and Safety in Therapeutics committee in conjunction with brolucizumab-induced inflammation reports by The American Academy of Ophthalmology [24, 25] Recent publications have raised concerns about these serious adverse events and reveal more detailed information [26]. Careful evaluation for inflammation and continued vigilance in monitoring brolucizumab treatment outcomes are advised [26].
Abicipar
The drug
Designed ankyrin repeated molecules (DARP) are considered one of the new potential substances to overcome antibody-based therapeutics. They are small and stable, with high specificity and affinity [27] and therefore considered a potential tool for VEGF inhibition [28].
Abicipar pegol (Abicipar, Allergan) is a DARP molecule of 14 kDa coupled to a 20 kDa polyethylene glycol (PEG) moiety to yield a 34 kDa molecule, directed to inhibit all isoforms of VEGF-A, with a prolonged intraocular effect to up to 13 days [29, 30].
Pivotal trials
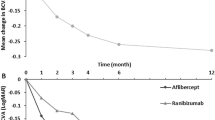
The REACH study, a phase 2, multicenter, RCT, compared the efficacy of abicipar 1 mg, abicipar 2 mg, and ranibizumab in patients with naïve nAMD which included 64 participants. At the first endpoint (16 weeks), mean change in BCVA was similar between the groups (+6.2, +8.3, and +5.6 for abicipar 1 mg, 2 mg, and ranibizumab, respectively). At 20 weeks, there was a continued improvement in the abicipar groups with a mean change in BCVA of +8.2, +10.00 letters in the 1 mg, and 2 mg, each, with an associated reduction in central macular thickness (CMT) compared to baseline, while BCVA in the ranibizumab group changed by +5.3 letters.
After the third abicipar injection, anatomical and functional changes were maintained for 3 months [31]. These encouraging results promoted phase 3 trials: The SEQUOIA and CEDAR studies were two multicenter, randomized, double-masked, clinical trials, comparing the efficacy of abicipar in two different dosing regimens vs. ranibizumab for patients with nAMD. The patients were randomized in the following manner (1:1:1):
-
1.
Abicipar 2 mg every 8 weeks after a loading dose of 3 monthly injections.
-
2.
Abicipar 2 mg, every 12 weeks after a loading dose of 3 monthly injections.
-
3.
Ranibizumab 0.5 mg monthly.
Patients in all treatment groups remained stable vision in >91% of cases. Compared to monthly ranibizumab, abicipar was non-inferior with Q8 and Q12 weeks intervals in terms of anatomical and visual outcomes, with less injections given in the abicipar groups (8 and 6 vs. 13, respectively) [32].
Safety profile
At 96 weeks, the rate of IOI was reported to be 15% in the abicipar group compared to 0.3% in the ranibizumab group. Initially, the average onset of IOI events was 22.3 days, being present in 68.7% of the patients after one of the first three monthly injections. However, after subsequent administration, these inflammatory responses were seen more rapidly, within 1 week after the drug was administered. The majority of participants in the abicipar group had mild to moderate IOI events (77.6%) with uveitis and vitritis being the most common clinical finding, whereas severe events were reported in 3.4% (43 patients), including retinal vasculitis in 1.8% [23, 30, 32].
Due to the high incidence of IOI, the manufacturer tried to improve this by modifying the manufacturing process. The safety results of this modification were shown in the MAPLE trial which was a 28-week open-label study which enrolled 123 participants. The incidence of IOI events was reduced to 8.9%, and severe IOI was reported in 2 cases (1.6%) with iritis and uveitis. No case of retinal vasculitis was seen in this study [33].
Despite the results shown in the MAPLE study, the FDA argued that the rate of IOI still results in an unfavorable benefit-risk ratio in the treatment of nAMD. The manufacturer is answering concerns raised by the FDA to approve the drug [34].
Faricimab
The drug
Faricimab, also known as RG7716, is a bispecific antibody and the first of its kind designed for intraocular use. Besides, it is a single molecule with a dual mechanism of action blocking angiopoietin-2 (ang-2) and VEGF-A simultaneously [35]. Ang-2 blocking promotes pericyte stabilization, decreased leakage, and inflammation.
Pivotal trials
The AVENUE trial was a 36-week, multiple-dose-regimen (1.5 and 6 mg faricimab), double-masked, phase 2 randomized clinical study comparing to ranibizumab. Although the primary endpoint of superiority of faricimab over ranibizumab in BCVA was not met, overall visual and anatomical gains supported pursuing phase 3 trials.
The STAIRWAY trial is a 52-week, multicenter, randomized, phase 2 study, aiming to assess the durability of faricimab for the treatment of nAMD vs. ranibizumab. Seventy-six nAMD patients were enrolled and randomized 2:2:1, to faricimab 6.0 mg Q12, 6.0 mg Q16 weeks (both with 4 monthly initial injections), and monthly ranibizumab 0.5 mg. Both faricimab arms were non-inferior to monthly ranibizumab injections in terms of functional and anatomical results [36].
TENAYA and LUCERNE are ongoing phase 3 trials with the primary outcome to compare 6.0 mg faricimab Q16 weeks interval to aflibercept 2.0 mg Q8 weeks. These studies are expected to be completed in 2022 [37, 38].
Safety profile
The STAIRWAY and AVENUE trials showed similar results: Faricimab was well tolerated, and there were no new or unexpected safety events. Results from the phase 3 trials need to be awaited for further safety results.
Conbercept
The drug
Conbercept is a recombinant fusion protein with a mixture of domains related to VEGF receptors 1 and 2, fused with the constant region (Fc) of human IgG1. Like aflibercept, conbercept binds to all isoforms of VEGF-A, VEGF-B, and PlGF [39]. In 2013, this fusion protein was approved in China for nAMD and has been used widely since then.
Pivotal trials
Clinical trials conducted in China have proven that conbercept is safe and effective with patients experiencing an improvement in BCVA and decrease in CMT [40, 41].
The PANDA 1 and 2 trials are ongoing multicenter, double-masked phase 3 RCT’s evaluating conbercept in the treatment of nAMD with two different doses and regimens compared to aflibercept. Their primary objective is to evaluate safety, durability, and efficacy of 0.5 mg conbercept Q8 weeks and 1.0 mg conbercept Q12 weeks, compared to aflibercept 2.0 mg Q8 weeks, after 3 mandatory initial loading dose injections in all arms.
In PANDA-2, at week 40, all three groups will perform a disease activity evaluation with VA and OCT driven assessment and continue on a PRN regimen until week 92 in case of stability [42, 43].
Safety profile
Data from phase 2 trials has shown that conbercept is well tolerated, and there were no new or unexpected safety events. Further safety results from the phase 3 trials are needed.
Discussion and conclusion
Anti-VEGF drugs have impacted positively in the management of retinal disease. However, health providers and patients are having to cope with the high burden of injections (including costs, as well as the frequent time consuming monitoring visits, and therapies in the current treatment). Minimizing the monitoring and injection burden is an important unmet need in the management of patients with nAMD. In real life settings, most of the patients do not receive the number of treatments and retreatments necessary to achieve anatomical and functional result shown in clinical randomized trials [4, 5, 44, 45]. This situation has led to frequent undertreatment [12].
A new era of therapies is characterized by more durable intravitreal effect, lasting up to 16 weeks. Although these new drugs have not shown superiority to the current standard of care in terms of vision gain, they do have the potential to improve real-world results by receiving less procedures per year i.e., improving patient’s compliance.
Despite the promise of these new therapies, other potential therapies have failed to reach clinic used in the past. Besides, we have been reading and experiencing sudden inflammation and extreme devastating side effects from long-lasting effect drugs. As such we must stay alert and report any side effects properly to the Health Authorities.
However, this new generation of therapies that has made it to phase 3 trials appears to be the strongest group yet to display the potential effectiveness and durability needed for approval.
In conclusion, the long-lasting drugs discussed in this manuscript open the door for a better nAMD treatments. Others are expected to follow in the future.
These long-lasting effect treatments should demonstrate better efficacy with longer effect and less frequent injections, in order to ameliorate the current algorithm of treatment in nAMD. In consequence, these treatments might lead to achieve less frequent checkups and fewer side effects. While these aims have not been achieved yet, ongoing trials might offer us answers in the near future.
References
Bourne RRA, Jonas JB, Bron AM, Cicinelli MV, Das A, Flaxman SR, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe in 2015: magnitude, temporal trends and projections. Br J Ophthalmol. 2018;102:575–85. https://www.ncbi.nlm.nih.gov/pubmed/29545417.
Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY. Age-related macular degeneration. Lancet. 2012;379:1728–38. https://www.ncbi.nlm.nih.gov/pubmed/22559899.
Cantor LB, Rapuano C, Cioffi G. Retina and vitreous. San Francisco: American Academy of Ophthalmology; 2014.
The CATT Research Group. The CRG. Ranibizumab and bevacizumab for neovascular. N Engl J Med. 2011;364:1897–908. http://blogs.nejm.org/now/index.php/ranibizumab-and-bevacizumab-for-neovascular-age-related-macular-degeneration/2011/05/18/trackback/.
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48.
Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON a multicenter cohort study (SEVEN-UP). Ophthalmology. 2013;120:2292–9.
Singer MA, Awh CC, Sadda S, Freeman WR, Antoszyk AN, Wong P, et al. HORIZON: an open-label extension trial of ranibizumab for choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology. 2012;119:1175–83. https://www.ncbi.nlm.nih.gov/pubmed/22306121.
Bhisitkul RB, Mendes TS, Rofagha S, Enanoria W, Boyer DS, Sadda SVR, et al. Macular atrophy progression and 7-year vision outcomes in subjects from the ANCHOR, MARINA, and HORIZON studies: the SEVEN-UP study. Am J Ophthalmol. 2015;159:915. https://doi.org/10.1016/j.ajo.2015.01.032.
Grunwald JE, Pistilli M, Daniel E, Ying G-S, Pan W, Jaffe GJ, et al. Incidence and growth of geographic atrophy during 5 years of comparison of age-related macular degeneration treatments trials. Ophthalmology. 2017;124:97–104.
Holz FG, Tadayoni R, Beatty S, Berger A, Cereda MG, Cortez R, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99:220–6. https://www.ncbi.nlm.nih.gov/pubmed/25193672.
Ramakrishnan MS, Yu Y, VanderBeek BL. Association of visit adherence and visual acuity in patients with neovascular age-related macular degeneration: secondary analysis of the comparison of age-related macular degeneration treatment trial. JAMA Ophthalmol. 2020;138:237–42. https://doi.org/10.1001/jamaophthalmol.2019.4577.
Holz FG, Tadayoni R, Beatty S, Berger A, Cereda MG, Hykin P, et al. Key drivers of visual acuity gains in neovascular age-related macular degeneration in real life: findings from the AURA study. Br J Ophthalmol. 2016;100:1623–8.
Karampelas M, Pefkianaki M, Rees A, Gill N, Kotecha A, Hamilton R, et al. Missed hospital appointments of patients receiving ranibizumab therapy for neovascular age-related macular degeneration. Ophthalmol Ther. 2015;4:43–9.
Obeid A, Gao X, Ali FS, Aderman CM, Shahlaee A, Adam MK, et al. Loss to follow-up among patients with neovascular age-related macular degeneration who received intravitreal anti–vascular endothelial growth factor injections. JAMA Ophthalmol. 2018;136:1251–9. https://doi.org/10.1001/jamaophthalmol.2018.3578.
Droege KM, Muether PS, Hermann MM, Caramoy A, Viebahn U, Kirchhof B, et al. Adherence to ranibizumab treatment for neovascular age-related macular degeneration in real life. Graefes Arch Clin Exp Ophthalmol. 2013;251:1281–4.
Brunton LL, Hilal-Dandan R, Knollmann BC Editors. In: Goodman & Gilman’s, editor. The pharmacological basis of therapeutics, 13th ed. New York, NY: McGraw-Hill Education; 2017. http://accessmedicine.mhmedical.com/content.aspx?aid=1154973599.
Sharma A, Kumar N, Parachuri N, Sharma R, Bandello F, Kuppermann BD, et al. Brolucizumab and immunogenicity. Eye. 2020;34:1726–28.
Agency EM. Assessment report; Beovu. Assess. Rep. EMA/23630/2020 Comm. Med. Prod. Hum. Use. 2019;1–6.
Nguyen QD, Das A, Do DV, Dugel PU, Gomes A, Holz FG, et al. Brolucizumab: evolution through preclinical and clinical studies and the implications for the management of neovascular age-related macular degeneration. Ophthalmology. 2020;127:963–76.
Holz FG, Dugel PU, Weissgerber G, Hamilton R, Silva R, Bandello F, et al. Single-chain antibody fragment VEGF inhibitor RTH258 for neovascular age-related macular degeneration. Ophthalmology. 2016;123:1080–9.
Yannuzzi NA, Freund KB. Brolucizumab: evidence to date in the treatment of neovascular age-related macular degeneration. Clin Ophthalmol. 2019;ume 13:1323–9.
Dugel PU, Koh A, Ogura Y, Jaffe GJ, Schmidt-Erfurth U, Brown DM, et al. HAWK and HARRIER: phase 3, multicenter, randomized, double-masked trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2020;127:72–84.
Michael Singer MD, Effie Z, Rahman M. Update on longer-acting anti-VEGF therapies/an expansive horizon is coming into focus. Retinal Phys. 2020;17:38–41.
ASRS. American Society of Retina Specialists Research and Safety in Therapeutics Committee. 2020; p. 1. https://www.asrs.org/clinical/clinical-updates/2976/New-nbsp-ReST-Committee-Report-Summarizes-Analysis-of-Reported-Cases-of-Inflamma.
Rajan K. Update: Brolucizumab’s safety under review. Compr. Ophthalmol. Retin. https://www.aao.org/headline/brolucizumab-s-safety-under-review.
Rosenfeld PJ, Browning DJ. Is this a 737 max moment for brolucizumab? Am J Ophthalmol. 2020;216:A7–8.
Stumpp MT, Binz HK, Amstutz P. DARPins: a new generation of protein therapeutics. Drug Discov Today. 2008;13:695–701.
Stahl A, Stumpp MT, Schlegel A, Ekawardhani S, Lehrling C, Martin G, et al. Highly potent VEGF-A-antagonistic DARPins as anti-angiogenic agents for topical and intravitreal applications. Angiogenesis. 2013;16:101–11.
Rodrigues GA, Mason M, Christie L-A, Hansen C, Hernandez LM, Burke J, et al. Functional characterization of abicipar-pegol, an anti-VEGF DARPin therapeutic that potently inhibits angiogenesis and vascular permeability. Investig Opthalmology Vis Sci. 2018;59:5836.
Moisseiev E, Loewenstein A. Abicipar pegol—a novel anti-VEGF therapy with a long duration of action. Eye. 2020;34:605–6.
Callanan D, Kunimoto D, Maturi RK, Patel SS, Staurenghi G, Wolf S, et al. Double-masked, randomized, phase 2 evaluation of abicipar pegol (an anti-VEGF DARPin therapeutic) in neovascular age-related macular degeneration. J Ocul Pharmacol Ther. 2018;34:700–9.
Kunimoto D, Yoon YH, Wykoff CC, Chang A, Khurana RN, Maturi RK, et al. Efficacy and safety of abicipar in neovascular age-related macular degeneration: 52-Week Results of Phase 3 Randomized Controlled Study. Ophthalmology. 2020;127:1331–44.
Molecular Partners AG. The MAPLE study used a modified manufacturing process and demonstrated decreased intraocular inflammation. Press RELEASE. https://www.molecularpartners.com/allergan-and-molecular-partners-announce-topline-safety-results-from-maple-study-of-abicipar-pegol/.
Jerry Helzner. DARPin fails to get approval due to inflammation issue. Retin. Physician. https://www.retinalphysician.com/issues/2020/june-2020/darpin-fails-to-get-approval-due-to-inflammation.
Sharma A, Kumar N, Kuppermann BD, Bandello F, Loewenstein A. Faricimab: expanding horizon beyond VEGF. Eye. 2020;34:802–4.
Danzig CarlJ, Lin Hugh, Guibord Pascal, Silverman David, Ruiz CarlosQuezada, Ivo Stoilov ZH. Clinical Effects of Blocking Ang-2 and VEGF with Faricimab in the Phase 2 STAIRWAY Trial. Investig Ophthalmol Vis Sci. 2020;61:1160.
ClinicalTrials.gov. A study to evaluate the efficacy and safety of faricimab in participants with neovascular age-related macular degeneration (LUCERNE). https://clinicaltrials.gov/ct2/show/NCT03823300.
ClinicalTrials.gov. A study to evaluate the efficacy and safety of faricimab in participants with neovascular age-related macular degeneration (TENAYA). https://clinicaltrials.gov/ct2/show/NCT03823287.
Sun X, Lu X. Profile of conbercept in the treatment of neovascular age-related macular degeneration. Drug Des Dev Ther. 2015;9:2311–20.
Li X, Xu G, Wang Y, Xu X, Liu X, Tang S, et al. Safety and efficacy of conbercept in neovascular age-related macular degeneration. Ophthalmology. 2014;121:1740–7.
Liu K, Song Y, Xu G, Ye J, Wu Z, Liu X, et al. Conbercept for treatment of neovascular age-related macular degeneration: results of the randomized phase 3 PHOENIX study. Am J Ophthalmol. 2019;197:156–67.
ClinicalTrials.gov. Efficacy and safety trial of conbercept intravitreal injection for neovascular age-related macular degeneration (PANDA-1). https://clinicaltrials.gov/ct2/show/NCT03577899.
ClinicalTrials.gov. Efficacy and safety trial of conbercept intravitreal injection for neovascular age-related macular degeneration (PANDA-2). https://clinicaltrials.gov/ct2/show/NCT03630952.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1432–44.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iglicki, M., González, D.P., Loewenstein, A. et al. Longer-acting treatments for neovascular age-related macular degeneration—present and future. Eye 35, 1111–1116 (2021). https://doi.org/10.1038/s41433-020-01309-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01309-9
This article is cited by
-
Accuracy of biomicroscopy, ultrasonography and spectral-domain OCT in detection of complete posterior vitreous detachment
BMC Ophthalmology (2023)
-
Potential for Treatment Interval Extension in Eyes with nAMD Disease Activity Post Loading Phase in HAWK and HARRIER
Ophthalmology and Therapy (2023)
-
Influence of lesion location on lesion reactivation after initial treatment in neovascular age-related macular degeneration
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Intraprocedural OCT monitoring of the immediate treatment response during indocyanine green angiography-guided laser therapy of teleangiectatic capillaries in diabetic macular edema
Scientific Reports (2022)
-
Comparison of agents using higher dose anti-VEGF therapy for treatment-resistant neovascular age-related macular degeneration
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)