Abstract
Purpose
To compare the macular microvasculature differences in cases with idiopathic macular hole (MH) after vitrectomy when using internal limiting membrane (ILM) removal or temporal inverted ILM flap technique (IFT).
Method
A total of 34 patients were included, of whom 20 were treated vitrectomy with ILM removal (group 1), and 14 were treated with IFT (group 2). The OCTA (RTVue; Optovue, Fremont, CA) parameters, including foveal avascular zone (FAZ), vessel density (VD) ratios in superficial capillary plexus (SCP), and deep capillary plexus (DCP) were evaluated at baseline and 6 months follow-up. The VD measurements in DCP and inner retinal thickness (IRT) in temporal and nasal sectors were compared in subanalyses.
Results
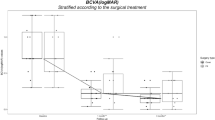
There was no significant difference in means of post-operative BCVA and FAZ between the two groups (p = 0.943, p = 0.760). The mean VDs of the DCP was significantly decreased at 6 months postoperatively in both groups (p < 0.001, p < 0.001). The mean post-operative temporal VDs of DCP were similar in the two groups, but the mean post-operative nasal VDs of the DCP was lower in group 1 than in group 2 (p = 0.005 and p = 0.03 for parafovea and perifovea, respectively). The mean temporal IRTs were similar in the two groups, but paranasal and perinasal IRTs were significantly thinner in group 1 than in group 2 (p < 0.001, p < 0.001). The mean post-operative VDs of parafoveal and perifoveal temporal and nasal quadrants in DCP significantly and positively correlated with the IRTs.
Conclusion
Single-layered temporal IFT causes fewer VD changes when compared to complete ILM removal, especially in the DCP.
Similar content being viewed by others
Introduction
The surgical treatment for full-thickness macular holes (MH) frequently consists of a pars plana vitrectomy (PPV) with an internal limiting membrane (ILM) peeling and use of gas tamponade with a high anatomical success rate [1,2,3,4]. A long-term follow-up study has found that the ILM peeling improved the rate of hole closure. However, the functional outcomes of large, recurrent or myopic MHs were not so promising [5,6,7,8].
The classical inverted flap technique (IFT), first described by Michalewska et al., is a potentially helpful surgical technique for treating large idiopathic MHs [9]. In previous studies, IFT has been demonstrated to improve the rate of hole closure, especially for large MHs [9,10,11,12,13]. The removal of ILM, which is formed by the footplates of Müller cells, is complicated by the potential iatrogenic damage in the nerve fibre layer (NFL). An alternative ILM peeling technique was developed to improve anatomical and functional results. This novel technique involves the single-layered temporal inverted flap by preserving the nasal part of ILM and is as efficient as the conventional technique [14].
Developments in optical coherence tomography angiography (OCTA) have enabled more detailed analyses to evaluate signs of anatomic recovery of retinal microstructure after MH surgery. OCTA has demonstrated that deep capillary plexus (DCP) is particularly affected, and the foveal avascular zone (FAZ) area is decreased after MH surgery [15, 16].
Previous studies have reported the features of OCTA images in eyes with MH. However, the microvascular changes between surgery techniques have not been widely studied. In this study, we evaluated the features of the retinal microvasculature in eyes with closed MH after surgery using OCTA. The aim of this study was to compare the macular microvasculature differences in patients with idiopathic MH after vitrectomy with conventional ILM removal and temporal inverted IFT.
Methods
Cases consisting of 34 patients who were referred to the Mugla Sitki Kocman University Ophthalmology Department from January 2017 to May 2019 were retrospectively reviewed. The study included those cases with large MHs who underwent PPV with either conventional ILM peeling removal (Group 1) or single-layered temporal IFT (Group 2). All patients were informed of the study, and written informed consent was obtained. This study adhered to the principles of the Declaration of Helsinki. Approval from the institutional review board/ethics committee was obtained.
Cases with idiopathic MH, least baseline hole diameter >400 μm, and a minimum follow-up of 6 months were included in the study. Exclusion criteria consisted of history or symptoms of chorioretinal diseases (such as diabetic retinopathy, retinal vascular occlusion, and retinal and choroidal inflammatory disease), optic nerve disease, previous intraocular surgeries, high intraocular pressure, high refractive error, axial length (AXL) > 26 mm in either eye. Patients with secondary MHs, for example, MH after blunt ocular trauma and MH associated with a retinal detachment, were also excluded.
Demographic information and follow-up data were obtained from all the individuals’ records. A detailed ophthalmic examination that included measurement of best-corrected visual acuity (BCVA), slit-lamp examination, dilated fundus examination, axial length measurement with no-contact partial coherence laser interferometry, optical coherence tomography (OCT), and OCTA was performed in all patients. The BCVA was measured with a Snellen chart, and the decimal values were converted to the logarithm of minimal angle of resolution units for statistical analyses. These examinations were performed at baseline and 6 months postoperatively.
The OCTA (RTVue; Optovue, Fremont, CA) database was reviewed in all patients at baseline and 6th month postoperatively. An experienced ophthalmic technician performed the OCTA examinations and OCTA data were analysed by two of the authors (SS, SK) who were masked to the postoperative findings. The VD was automatically calculated by the software embedded in the OCTA scanner. The SCP was located between 3 mm below the ILM to 15 mm below the inner plexiform layer and the DCP extended from 15 mm to 70 mm below the inner plexiform layer. The parafoveal regions of the ETDRS grid (3 mm diameter) were used for the regional analysis of the VD for both the SCP and DCP. The scan area of 6 mm × 6 mm (about 10° angle of a view), centred on the macula, was performed in this study. “Auto All” function of the device, OCTA signal position and signal quality were determined and the scan quality below 7/10 was considered an exclusion criterion from the study. Retinal microvasculature was analysed using the automated retinal layer segmentation algorithm that is available on the device. In cases in which we obtained insufficiency of automatic layer segmentation, the correction was performed manually. The OCTA features were compared between the groups over the follow-up time. The VD ratios in the DCP and inner retinal thickness (IRT) in temporal and nasal sectors were evaluated in subanalyses. The postoperative OCTA values were compared with fellow eyes.
The 25-G 3-port was used to PPV and the ILM was stained with Membrane Blue (Dual, Dorc, Zuiland, the Netherland) for 10 s and took out by gripping with forceps peeling about 3 disc diameters centred on the fovea in group 1. In group 2 ILM was peeled from the temporal area of the macula and created flap was folded over the MH and nasal region. After the fluid-air exchange, 20% SF6 gas endo tamponade was injected in all cases, and face-down positioning was ordered. Phacoemulsification with intraocular lens implantation was performed simultaneously for avoiding the decrement of visual acuity due to cataract.
The SPSS 22.0 (SPSS, Inc, Chicago, IL) software program was used for statistical analyses. Continuous variables are given as mean ± SD, and qualitative variables are shown as frequencies (absolutes) and percentages (%). Quantitative variables were checked by the Shapiro–Wilk test for the normality hypothesis. The Student’s t test was used for comparisons between continuous variables (with normal distribution). Comparisons between categorical variables were evaluated using contingency tables and the Chi-square test or Fisher’s test, when necessary. Also, according to the change in the FAZ and VD ratios, the general linear modelling technique for repeated measurements was used to examine the significance of the change in time for the groups. For significant interaction terms, simple effects analysis was performed with Bonferroni correction as a post-hoc procedure. The model included time (pre- and post-operative values), group (group 1 vs. group 2) main effect terms, and time × group interaction effect term. Pearson’s correlation analyses were used to examine the relationships between inner IRT and post-operative VD. Analysis of variance (ANOVA) and post-hoc Tukey’s honestly significant differences were calculated to compare differences between group 1, group 2, and fellow eyes. A p value o5f lower than 0.05 was considered as statistically significant.
Results
A total of 34 eyes of 34 patients with surgically closed idiopathic MH were included in this study. Twenty patients were treated with PPV with conventional ILM removal (Group 1) and 14 patients were treated with PPV single-layered temporal IFT (Group 2). The hole was completely closed in all cases after the first operation, which was confirmed in OCT examination. Patient demographics, pre and postoperative anatomical and visual outcomes in the two groups are resumed in Table 1. All MHs were idiopathic and were larger than 400 µ. The mean preoperative BCVA of eyes improved significantly in two groups at postoperative 6 months (p < 0.001, p < 0.001). There was no significant difference in the two groups in terms of postoperative BCVA (p = 0.943). No complications, such as retinal detachment or endophthalmitis, were noted. The mean temporal IRTs were similar in two groups The paranasal and perinasal IRTs were significantly thinner in group 1 than in group 2 (p < 0.001, p < 0.001) (Table 1).
En face photographs of the macula revealed the preoperative cystic areas encircling the hole in all MH eyes with the resolution of the MH and neighbouring cystic areas in all cases. Nerve fibre layer (NFL) defects were observed in the peeled region (temporal and nasal side) in group 1 (Fig. 1a). In group 2, NFL defects were observed only on the temporal region of the retina (Fig. 1b).
a En face image of the central retina and Bscan image at 6 months after vitrectomy and ILM removal in a patient. (White arrows show the edge of peeled ILM flap and yellow arrows show nerve fibre layer defects.) b En face image of the central retina and Bscan image postoperatively in a patient who had temporal inverted ILM flap surgery. (White arrows show nerve fibre layer defects only on the temporal (peeled) side of retina. Yellow arrow shows the edge of ILM flap defects).
The pre and postoperative mean FAZ, VD ratios in SCP and DCP are shown in Table 2. The mean FAZ areas were significantly decreased over follow-up time (6 months) in two groups (p < 0.001). There was no significant difference between the two groups in terms of FAZ change over time. (p = 0.07) The mean parafoveal and perifoveal VD ratios in SCP were similar in the groups and there was no change over time after the surgery. However, the mean parafoveal and perifoveal VDs of the DCP ratios were significantly decreased at 6 months postoperatively in two groups. (p < 0.001 and p < 0.001, respectively).
The mean temporal and nasal VD ratios of the DCP were compared between two groups over time after surgery in subanalyses. The mean VD ratios decreased over time in all cases. This decreasing in the parafoveal and perifoveal temporal quadrants were similar between groups. However, nasal VD in group 1 were decreased more evident than in group 2. (P group = 0.038). The mean postoperative nasal VD ratios of the DCP were lower in group 1 than in group 2. (For parafovea; 53.4% in group 1, 55.7% in group 2, p = 0.005. For perifovea; 55.4% in group 1, 57.9% in group2, p = 0.03) (Table 3).
The mean postoperative VDs of parafoveal temporal and nasal quadrants in DCP significantly and positively correlated with the IRTs (r = 0.533, p = 0.001; r = 0.620, p < 0.001, respectively). The mean postoperative VDs of perifoveal temporal and nasal quadrants in DCP significantly and positively correlated with the IRT (r = 0.862, p < 0.001; r = 0.824, p < 0.001, respectively).
The mean postoperative FAZ, parafoveal and perifoveal VD ratios of the DCP were significantly lower than the fellow eyes in two groups (Table 4).
Discussion
The most desirable surgical technique is still unknown for large and myopic MHs. The Large MHs have a potential of unclosed holes after a successful surgery [10]. Previous studies have shown that the peeling of ILM caused a significant improvement in postoperative anatomical outcomes in large MH surgery [17, 18]. However, this was not always viable for functional results [19].
The different method of temporal IFT, which involved the peeling of the ILM at the temporal side of the fovea, up to the margins of the MH and transposition of the flap nasally to cover the MH was recently described by Michalewska et al. [14]. The theory regarding this technique is to not remove the peeled ILM but to leave a half piece of it at the covering of the hole to function as a connection. The results of this novel technique were studied and reported as a functionally and anatomically successful method like the conventional IFT by previous studies in the literature [11, 14, 20, 21].
Previously, ILM peeling has been held responsible for some structural and microvascular changes in retina. One of the structural changes in retina is defects on NFL (DONFL) appearance after ILM peeling. ILM is thought to be a structural support for nerve fibres and peeling of ILM may cause nerve fibres into a dissociated structure [22]. Our findings were consistent with previous studies that DONFL were detected in the ILM peeled area [14, 20, 22]. We observed that DONFL was present at the temporal (peeled) side of the retina in the IFT group.
Iwasaki et al. reported higher percentages of complete repair of ELM and a higher increase in BCVA in the ILM peeling group compared with IFT in 24 cases with large MH. But in the IFT group, two different types of IFT were conducted, including ‘cover’ and ‘fill’ procedures [23]. Avcı et al. reported that single-layered temporal IFT methods have better functional, anatomical and morphological outcomes for the treatment of large MHs compared with classical ILM peeling [21]. They recommend that a single-layered, even ILM flap forms the optimal scaffold for retinal gliosis rather than a multilayered ILM flap or filling the MH with ILM in an irregular pattern [21]. Earlier OCT reports have similarly described the dynamic healing process that happens after the surgical repair of MHs. These authors performed a detailed analysis of the flap closure methods. They described that recovery initiated at the outer layer of the retina (firstly the ELM and secondly the ellipsoid zone) [15, 24]. In our study we have not observed any differences between the surgery groups in means of postoperative BCVA and OCT features (disruption ellipsoid zone and ELM). Although Iwasaki et al.’s study has included the same patients as ours, BCVA results were obviously different. We think this difference may be related to the technique that they used.
The ILM is acting as a base membrane for Muller cells. Therefore, mechanical disruption of Muller cells may contribute to damage of inner retinal layers. We thought that the single-layered temporal IFT can decrease this undesirable injury and limits it to temporal side where ILM is peeled. Visual and anatomical outcomes may be favourable.
Retinal vasculature is found at two levels: the SCP is localised at the level of the ganglion cell layer and the DCP is at the level of the inner nuclear layer. Therefore, we suggested that ILM peeling might change the retinal vasculature in addition to its structural effects on retina, both of which have close relationship with each other.
The effects of ILM peeling on retinal microvascular structure was previously reported by several authors. Baba et al. have found an increase VDs at both SCP and DCP after surgery and higher VDs at nasal quadrant than temporal quadrant. They also have found higher IRTs at nasal quadrant. They have concluded that these outcomes are associated with retinal slippage towards nasal side [22]. Kim et al. have found lower VD particularly at DCP after MH surgery [16]. Furthermore, Michalewska et al. showed lower VDs at temporal side where she performed ILM peeling and concluded that ILM peeling might alter the blood flow particularly at deep retinal layers [20]. There is no study comparing the structural and microvacular effects of two different ILM peeling techniques. We found a decrease of FAZ areas in both groups, which is related to centripedal contraction of retina during healing process and consistent with previous reports. However, unlike Baba et al., DCP VDs significantly decreased at both parafovea and perifovea in both surgical groups. In addition, DCP VD decrease was significantly higher at complete ILM removal at both parafovea and perifovea. Furthermore, DCP VD decrease was similar at temporal side (where ILM was peeled) in both groups but higher in group 1 compared to group 2 [22].
Why ILM peeling effected DCP rather than SCP? Cystic changes around MH occur at inner nuclear and outer plexiform layer where DCP exists and were postulated as the result of DCP breakdown. This vascular breakdown may not be restored after MH closure and the loss of supportive effect of Müller cell glial processes inner retinal layers after ILM peeling may have an additional effect on VD decrease particularly at DCP. This is likely because of a loss of ILM supportive effect on the inner retina, retinal microvasculature may be more prone to late recovery. We did not evaluate foveal displacement and its effect on macular microvascular structure as mentioned by Baba et al. However, we thought that ILM peeling, with the loss of support on inner retinal layers, appears to affect deep microvascular structure more than foveal displacement. Because, unlike Baba et al., nasal VDs decreased and this decrease was higher at complete ILM removal group. We found that the nasal IRT was thicker in the temporal IFT group at 6 months after the surgery. There were significant positive correlations between the VD of DCP and the IRT at 6 months similar to their study [22].
It is reported in the literature that the VD ratios in DCP were decreased after vitrectomy and ILM peeling [9, 25]. Also, previous studies showed that the mean VD in the DCP was significantly lower in the surgical eyes than in the control group [20, 26, 27]. Recently Michalewska et al. reported the decrement of the VD in DCP at the temporal side when compared with the nasal side after surgery. They hypothesised a further superiority of the temporal inverted ILM flap technique (IFT) over techniques relying on complete ILM peeling [20]. In our study, we compared the FAZ and the VD ratios after vitrectomy with ILM removal and single-layered temporal IFT. The mean FAZ and VD ratios in DCP significantly decreased in both groups over time. Similar to Michalewska et al.’s study, we found lower VD in DCP at the temporal side when compared with the nasal side after surgery in the IFT group.
Vessels abnormalities are observed in the exact area where ILM peeling is performed might result in prolonged regeneration. The restorative process after MH surgery may be involved in both anatomic and hemodynamic modifications of the inner retina. The lower VD ratios might mean that a reduction of functional vascular density after MH surgery may limit the dynamic healing process and lead to undesirable BCVA, despite the anatomical success of the surgery. We suggest that the temporal IFT reduced the unnecessary injury to the microvasculature of inner retina layers.
This study was limited in retrospective nature and lower sample sizes. To the best of our knowledge, a strength of the study is that FAZ and VD ratios were compared quantitatively via OCTA between the ILM removal and temporal IFT in anatomically closed large MHs for the first time. We reported early results of MH surgery in this study, and further studies on more patients with long-term follow up are needed.
In summary, single-layered temporal IFT causes less VD changes when compared to complete ILM removal especially in the DCP. OCTA might be a beneficial instrument for the evaluation of vascular changes in MHs pre and postoperatively. Consequently, the restoration of the retinal microvasculature after MH surgery may influence the postoperative visual acuity by altering the photoreceptor structure and inner retinal layers and explain the poor postoperative BCVA.
Summary
What was known before
-
The most desirable surgical technique is still unknown for large and myopic MHs.
-
The Large MHs have a potential of unclosed holes or delayed visual acuity after a successful surgery.
What this study adds
-
The paranasal and perinasal vessel density of DCP and IRT of nasal parafovea and perifovea are higher in single-layered temporal flap technique than complete ILM removal.
-
The temporal IFT reduced the unnecessary injury to the microvasculature of inner retina layers.
References
Rahimy E, McCannel CA. Impact of internal limiting membrane peeling on macular hole reopening: a Systematic Review and Meta-Analysis. Retina. 2016;36:679–87.
Lai MM, Williams GA. Anatomical and visual outcomes of idiopathic macular hole surgery with internal limiting membrane removal using low-concentration indocyanine green. Retina. 2007;27:477–82.
Kannan NB, Kohli P, Parida H, Adenuga OO, Ramasamy K. Comparative study of inverted internal limiting membrane (ILM) flap and ILM peeling technique in large macular holes: a randomized-control trial. BMC Ophthalmol. 2018;18:177.
Mester V, Kuhn F. Internal limiting membrane removal in the management of full-thickness macular holes. Am J Ophthalmol. 2000;129:769–77.
Brooks HL Jr. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000;107:1939–48. discussion 1948–1939
Rizzo S, Belting C, Genovesi-Ebert F, Cresti F, Vento A, Martini R. Successful treatment of persistent macular holes using “heavy silicone oil” as intraocular tamponade. Retina. 2006;26:905–8.
Hillenkamp J, Kraus J, Framme C, Jackson TL, Roider J, Gabel VP, et al. Retreatment of full-thickness macular hole: predictive value of optical coherence tomography. Br J Ophthalmol. 2007;91:1445–9.
D’Souza MJ, Chaudhary V, Devenyi R, Kertes PJ, Lam WC. Re-operation of idiopathic full-thickness macular holes after initial surgery with internal limiting membrane peel. Br J Ophthalmol. 2011;95:1564–7.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25.
Mahalingam P, Sambhav K. Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol. 2013;61:601–3.
Khodani M, Bansal P, Narayanan R, Chhablani J. Inverted internal limiting membrane flap technique for very large macular hole. Int J Ophthalmol. 2016;9:1230–2.
Kuriyama S, Hayashi H, Jingami Y, Kuramoto N, Akita J, Matsumoto M. Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol. 2013;156:125–31.e121.
Gekka T, Watanabe A, Ohkuma Y, Arai K, Watanabe T, Tsuzuki A, et al. Pedicle Internal Limiting Membrane Transposition Flap Technique for Refractory Macular Hole. Ophthalmic Surg Lasers Imaging. Retina. 2015;46:1045–6.
Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Adelman RA, Nawrocki J. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: a comparative study. Retina. 2015;35:1844–50.
Wilczynski T, Heinke A, Niedzielska-Krycia A, Jorg D, Michalska-Malecka K. Optical coherence tomography angiography features in patients with idiopathic full-thickness macular hole, before and after surgical treatment. Clin Inter Aging. 2019;14:505–14.
Kim YJ, Jo J, Lee JY, Yoon YH, Kim JG. Macular capillary plexuses after macular hole surgery: an optical coherence tomography angiography study. Br J Ophthalmol. 2018;102:966–70.
Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R, et al. Internal limiting membrane removal during macular hole surgery: results of a multicenter retrospective study. Ophthalmology. 2006;113:1401–10.
Rizzo S, Tartaro R, Barca F, Caporossi T, Bacherini D, Giansanti F. Internal Limiting Membrane Peeling Versus Inverted Flap Technique for Treatment of Full-Thickness Macular Holes: a Comparative Study in a Large Series of Patients. Retina. 2018;38:S73–S78.
Uemoto R, Yamamoto S, Aoki T, Tsukahara I, Yamamoto T, Takeuchi S. Macular configuration determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol. 2002;86:1240–2.
Michalewska Z, Nawrocki J. Swept-Source Optical Coherence Tomography Angiography Reveals Internal Limiting Membrane Peeling Alters Deep Retinal Vasculature. Retina. 2018;38:S154–60.
Avci R, Mavi Yildiz A, Yilmaz S. Conventional internal limiting membrane peeling versus temporal inverted internal limiting membrane flap for large macular holes. Eur J Ophthalmol. 2019: 1120672119892427.
Baba T, Kakisu M, Nizawa T, Oshitari T, Yamamoto S. Regional Densities of Retinal Capillaries and Retinal Sensitivities after Macular Hole Surgery with Internal Limiting Membrane Peeling. Retina. 2020;40:1585–91.
Iwasaki M, Kinoshita T, Miyamoto H, Imaizumi H. Influence of Inverted Internal Limiting Membrane Flap Technique on the Outer Retinal Layer Structures after a Large Macular Hole Surgery. Retina. 2019;39:1470–7.
Grewal DS, Reddy V, Mahmoud TH. Assessment of Foveal Microstructure and Foveal Lucencies Using Optical Coherence Tomography Radial Scans Following Macular Hole Surgery. Am J Ophthalmol. 2015;160:990–9.e991.
Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Nawrocki J. Inverted internal limiting membrane flap technique for surgical repair of myopic macular holes. Retina. 2014;34:664–9.
Demirel S, Degirmenci MFK, Bilici S, Yanik O, Batioglu F, Ozmert E, et al. The Recovery of Microvascular Status Evaluated by Optical Coherence Tomography Angiography in Patients after Successful Macular Hole Surgery. Ophthalmic Res. 2018;59:53–57.
Cho JH, Yi HC, Bae SH, Kim H. Foveal microvasculature features of surgically closed macular hole using optical coherence tomography angiography. BMC Ophthalmol. 2017;17:217.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karalezli, A., Kaderli, S.T. & Sul, S. Macular microvasculature differences in patients with macular hole after vitrectomy with internal limiting membrane removal or single-layered temporal inverted flap technique. Eye 35, 2746–2753 (2021). https://doi.org/10.1038/s41433-020-01301-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01301-3
This article is cited by
-
Update on surgical management of complex macular holes: a review
International Journal of Retina and Vitreous (2021)