Abstract
Purpose
To characterise the posterior and total corneal astigmatism using colour point-source light-emitting diodes (LED) topography.
Methods
In a prospective case series 400 eyes from 400 patients were evaluated by colour-LED topography. Only eyes with normal topographies were considered. The following parameters were studied: magnitude and distribution of SimK and posterior corneal astigmatism, correlation between SimK and posterior corneal astigmatism, and differences in magnitude and axis between total and anterior corneal astigmatism.
Results
The mean SimK corneal astigmatism was 1.21 ± 0.94 D. The mean posterior corneal astigmatism was 0.37 ± 0.24 D. Posterior astigmatism was vertically oriented in 68% of eyes. Twenty-two percent of eyes showed a posterior corneal astigmatism ≥ 0.50 D. The correlation coefficients between SimK and posterior corneal astigmatism were: r2 = 0.066; p = 0.371 in WTR eyes, r2 = 0.112; p = 0.173 in ATR eyes and r2 = −0.019; p = 0.879 in oblique eyes. A difference between SimK and total corneal astigmatism ≥ 0.50 D was found in 7% of eyes. A difference in axis between SimK and total corneal astigmatism ≥ 10° was found in 24% of eyes.
Conclusions
The percentage of eyes with posterior corneal astigmatism ≥ 0.50 D and the differences between anterior and total corneal astigmatism were higher than those previously reported in the literature. Therefore, this study supports the consideration of total corneal astigmatism magnitude and axis is mandatory for a precise surgical correction of astigmatism.
Similar content being viewed by others
Introduction
Cataract surgery is the most frequent surgical procedure in developed countries. In recent years, while having increasingly high success and patient satisfaction rates, a steady fusion of cataract and refractive surgery occurred. Nevertheless, one of the factors limiting visual acuity and spectacle independence after cataract surgery is astigmatism.
In general, it is estimated that up to 40% of patients undergoing cataract surgery have a corneal astigmatism of 1.00 D or more [1, 2], and it has been suggested that correction of astigmatism below 0.50 D has a limited visual benefit, whereas correction of astigmatism of more than 0.50 D can improve visual outcomes [3]. Therefore, without surgical correction of this astigmatic component, it is unlikely that spectacle independence will be achieved after surgery [3]. This, in turn, compromises the visual quality, leading to personal, social and economic burdens [4].
The most important source of error when calculating a toric intraocular lens (IOL) is not considering the astigmatism of the posterior corneal surface [5]. Ignoring its power in toric IOL calculation results in overcorrection in eyes with with-the-rule (WTR) astigmatism and undercorrection in eyes with against-the-rule (ATR) astigmatism [5,6,7]. The currently available nomograms to consider the posterior corneal surface in toric IOL calculation are based on data from Scheimpflug cameras [6, 8, 9]. Colour point-source light-emitting diodes (LED) topography provides consistent measures of posterior corneal curvature and astigmatism in healthy eyes [10]. In a recent study [11], direct measurement of the posterior corneal surface with colour-LED topography showed better performance than a Scheimpflug camera in toric IOL calculation.
Accounting for the limited precision of current technologies and lack of a gold standard for evaluating corneal astigmatism and particularly the posterior corneal surface, knowledge of normative ocular biometric parameters is essential in IOL power calculation. The purpose of this study is to characterise the posterior and total corneal astigmatism (TCA) in normal eyes using colour-LED topography.
Methods
In a prospective case series 400 eyes from 400 patients were evaluated by colour-LED topography. Only eyes with normal topographies were considered. The following parameters were studied: magnitude and distribution of SimK and posterior corneal astigmatism, correlation between SimK and posterior corneal astigmatism, and differences in magnitude and axis between anterior and TCA.
Population sample
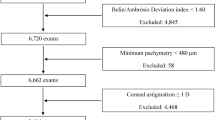
This study prospectively reviewed colour-LED topography images taken in the Department of Ophthalmology, Hospital da Luz Lisboa, from December 2016 to April 2018. 400 eyes from 400 patients were included.
Each scan met the manufacturer’s specifications. Patients with anterior astigmatism magnitude of 6.00 D more were excluded from this study. Also excluded were patients with dry eye or Meibomian gland disease, patients with contact lens use in the 2 weeks prior to the examination and patients with corneal disease (pterygium, ectasia, keratoconus or evidence of corneal dystrophy). The exam with the highest posterior quality factor obtained of each patient was selected for inclusion in the study. One eye of each patient was randomly selected for analysis. The randomisation was performed using Excel RAND function.
The study was approved by Hospital da Luz Lisboa Ethics Committee and carried out in accordance with the ethical principles for medical research with human beings approved by the Helsinki declaration. Written informed consent was obtained from each subject before inclusion in the study.
Device and measurements
All eyes were measured using a Colour-LED topographer (Cassini I-Optics, Den Haag, The Netherlands, software v2.4.1). The Cassini has approximately 700 red, yellow, and green LEDs arranged in a specific pattern to ensure a 1-to-1 correspondence between the source and image points. Using forward ray tracing, the anterior corneal surface is reconstructed. This information, combined with the second Purkinje reflex of seven additional infra-red LEDs to study the posterior surface of the cornea (again, using forward ray tracing), allows the Cassini to measure TCA [12].
The following parameters were evaluated with the Cassini:
-
(1)
SimK corneal astigmatism (1.3375):
Corneal astigmatism from simulated keratometry (K) over the 0.0–3.0 mm zone. The magnitude of corneal astigmatism (CA) SimK is the difference between steep simulated K and flat simulated K, and the meridian is the steep simulated K meridian. This value is calculated based on the anterior corneal measurement only, using the effective corneal refractive index of 1.3375.
-
(2)
Anterior corneal astigmatism (1.376):
CA from the anterior corneal surface, which is uniquely measured instantaneously over the 0.0–3.0 mm zone. The magnitude of CA anterior is calculated from the measured radius of curvature (r) by (1.376–1.0)/Roc, in which the refractive index of air is 1.0, the refractive index of the cornea is 1.376 and the r is expressed in metres. The CA anterior power is calculated for both the steep and flat meridian. The difference represents CA of the anterior corneal surface.
-
(3)
Posterior corneal astigmatism (1.336):
CA from the posterior corneal surface, measured at a ring with a diameter of ~3.8 mm using an instantaneous recording of the second Purkinje images. A ray-tracing model is used to convert the measurement points into the posterior corneal r for the steep and flat meridian. Posterior corneal power for both meridians is calculated through (1.336–1.376)/Roc, in which the refractive index of the cornea is 1.376, the refractive index of the aqueous humour is 1.336 and the r is expressed in metres.
-
(4)
Total corneal astigmatism:
CA from TCA displayed on the device. The TCA is measured by parallel ray tracing through the anterior and posterior corneal surfaces using the Snell law over the central 0.0–3.0 mm zone. This calculation of TCA combines the contributions of the anterior and posterior corneal surfaces independently of the effect of corneal thickness.
The internal quality verification tests included in the device were utilised to validate the quality of the obtained measurement for acceptance in the study. The selected measurements of the Cassini device were those in which all quality indicators (quality factor centration (lateral), quality factor focus (axial), quality factor corneal coverage, quality factor stability value and quality factor posterior value) were 85% or more (represented by green colour on the display).
Statistical analysis
The sample size was calculated for an alpha of 0.05 and a power of 0.80. A standard deviation (SD) in visual acuity of 0.84 D in astigmatism magnitude was presumed, based on previous data analyses in a previous study from our group [1]. According to this calculation, 328 eyes should be included.
Database design and statistical analysis was performed using Microsoft Office Excel (Microsoft Corp.) and SPSS software (version 24.0, SPSS, Inc.). The results of the quantitative variables were expressed by their minimum and maximum values, means, and SDs. For comparing variables between subgroups, an ANOVA test with Bonferroni correction was used. Correlations between variables were investigated with linear regression models with SimK astigmatism as the independent variable. A p value ≤ 0.05 was considered statistically significant.
Data analysis
Eyes were divided in subgroups according to steep meridian location, as follows:
Eyes with anterior astigmatism steep meridian between 60 degrees (°) and 120° were classified as WTR (with-the-rule astigmatism), between 30° and 60° and between 120° and 150° as oblique astigmatism (OBL), and between 0° and 30° and between 150° and 180° as ATR (against-the-rule astigmatism).
The following parameters were investigated:
-
(1)
Magnitude and distribution of anterior, SimK, and posterior corneal astigmatism.
-
(2)
Correlations between SimK, posterior and TCA.
-
(3)
Differences in magnitude and axis between total and SimK corneal astigmatism.
-
(4)
According to the magnitude of SimK corneal astigmatism, percentage of cases with a mean difference in magnitude between total and SimK astigmatism of 0.50 D or more and in axis of 10° or more.
Results
Magnitude and distribution of corneal astigmatism
This study included 400 eyes of 400 patients.
Minimum SimK was 42.85 ± 2.02 D (range 34.62–51.73) and maximum SimK was 44.06 ± 2.08 D (35.80–53.80). Minimum anterior keratometry was 47.74 ± 2.25 D (38.56–57.63) and maximum anterior keratometry was 49.09 ± 2.32 D (39.89–59.93). Minimum posterior keratometry was −6.00 ± 0.31 D (−6.82 to −5.01) and maximum posterior keratometry was −6.37 ± 0.32 D (−7.59 to −5.28).
The magnitude of astigmatism is shown in Table 1. The mean magnitude of SimK corneal astigmatism was 1.21 ± 0.94 D (range, 0.02–5.73). SimK corneal astigmatism was significantly higher in eyes with ATR and WTR astigmatism than in eyes with OBL (p < 0.001) The mean magnitude of posterior corneal astigmatism was 0.37 ± 0.24 D (range, 0.02–1.44 D). Posterior corneal astigmatism magnitude was higher in eyes with WTR than in eyes with ATR and OBL SimK astigmatism (p < 0.001).
The distribution of the steep meridian location in the anterior and posterior surface is shown in Fig. 1. Concerning the anterior corneal surface, the most frequent location of the steep meridian, in 186 eyes (47%), was WTR; 149 eyes (37%) showed ATR astigmatism, and 65 eyes (16%) OBL (Fig. 1). In the posterior corneal surface, 270 eyes (68%) had a WTR orientation of the steep meridian; 53 eyes (13%) ATR, and 77 eyes (19%) oblique. Globally, the distribution of the TCA steep meridian location was WTR in 156 eyes (39%); ATR in 167 eyes (42%) and oblique in 77 eyes (19%).
Vertical orientation was the most common for posterior corneal astigmatism, in 68% of cases. This WTR orientation was the most common, irrespective of anterior meridian location. The location of the posterior steep meridian according to the location of the anterior steep meridian is shown in Fig. 2.
In 82% of eyes, TCA magnitude was 0.50 D or more. Posterior corneal astigmatism magnitude was 0.50 D or more and in 22% of eyes. The distribution of posterior and TCA is shown in Fig. 3.
Correlation between SimK and posterior corneal astigmatism
Correlations between SimK and TCA are shown in Fig. 4. A weak positive correlation was found between SimK and posterior corneal astigmatism in WTR eyes (r2 = 0.066; p = 0.371). This correlation was also weak in ATR eyes (r2 = 0.112; p = 0.173) and non-significant in oblique eyes (r2 = −0.019; p = 0.879). A very strong positive correlation was observed between SimK and TCA (r2 = 0.904; p < 0.001). This correlation is shown in Fig. 5.
Top: Correlation between SimK and total corneal astigmatism in WTR eyes. Middle: Correlation between SimK and total corneal astigmatism in ATR eyes. Bottom: Correlation between SimK and total corneal astigmatism in OBL eyes. (WTR with-the-rule, ATR against-the-rule, OBL oblique; PCA posterior corneal astigmatism).
Differences between total and SimK corneal astigmatism
The differences between total and SimK corneal astigmatism are shown in Table 2.
The mean difference in magnitude between SimK and TCA was 0.22 ± 0.17 D, in the WTR eyes the mean difference was 0.19 ± 0.14 D (p < 0.001 for ATR and p > 0.999 for oblique), in the ATR eyes the mean difference was 0.27 ± 0.19 D (p < 0.001 for ATR and p = 0.017 for oblique), and in the oblique eyes the mean difference was 0.20 ± 0.18 D.
A difference between SimK and TCA of more than 0.25 D was found in 39% of eyes and of more than 0.50 D was found in 7% of eyes.
The mean difference in axis difference between SimK and TCA was 14.81 ± 34.27°. In the WTR eyes the mean difference was 9.53 ± 14.90° (p = 0.006 for ATR and p = 0.657 for oblique); in the ATR eyes the mean difference was 21.07 ± 50.44° (p = 0.006 for WTR and p = 0.825 for oblique), and in the oblique eyes the mean difference was 15.55 ± 24.99°.
A difference between SimK and TCA of 10° or more was found in 24% of eyes.
A difference of 0.50 D or more in the magnitude of SimK and TCA and a difference of 10° or more in the location of the steep meridian was observed in 29% of cases.
Table 3 shows the differences in magnitude and axis of eyes with <1.00 D and ≥1.00 D of SimK astigmatism.
Considering eyes with SimK astigmatism ≥ 1.0 D, 10% of the evaluated eyes had a difference in magnitude ≥ 0.50 D. In addition to this, 7% of the evaluated eyes had a difference in axis ≥ 10°. In eyes with SimK astigmatism < 1.0 D, the differences in magnitude ≥ 0.50 D were less (4%), while the differences in axis ≥ 10° were more frequent (40%).
Discussion
This study evaluated posterior and TCA with colour-LED topography. Most published studies evaluated TCA with Scheimpflug tomography. This is, to our knowledge, the first study to do this evaluation using colour-LED topography.
Traditionally, the corneal curvature and astigmatism are studied with autokeratometers. These have several limitations. They measure only a small central area of the cornea, not providing peripheral information and presuming the cornea is symmetrical. Moreover, they only evaluate the anterior corneal surface, assuming a fixed ratio between the curvature of both corneal surfaces. In most cases, a standard keratometric index of 1.3375 is used for converting anterior surface measurements in total corneal power and astigmatism. This index overestimates the total corneal power in about 0.56 D, and this overestimation is increasingly important with steeper corneas [13, 14].
In recent years, the importance of considering the posterior corneal surface in astigmatic correction has been recognised. Not considering it is the most important source of error in toric IOL power calculation [5]. Most of our knowledge about the posterior corneal surface is based on data derived from Scheimpflug imaging-based devices [15,16,17,18]. Scheimpflug-based devices may underestimate vertical posterior astigmatism and overestimate it in the horizontal meridian [19, 20], and their repeatability in posterior corneal curvature evaluation has been shown to be lower than in anterior corneal curvature [21]. These limitations may explain why, in toric IOL power calculation directly measuring the posterior corneal surface is not superior to predicting its power with mathematical models [22, 23].
Because of the limited precision in evaluating corneal astigmatism, a new technology was introduced in 2014—colour-LED topography. We previously showed that measurements of the anterior corneal surface and TCA by colour-LED topography are more precise than those of automated keratometry or slit-scanning tomography. Furthermore, they are highly repeatable [10, 24, 25].
In our study, mean SimK corneal astigmatism was 1.21 ± 0.94 D. In a recent study using an automated keratometer, we found this value to be similar (1.08 ± 0.84 D), despite the different evaluation methods [1].
The mean magnitude of posterior corneal astigmatism was 0.37 ± 0.24 D. This value is in accordance with several published studies using Scheimpflug imaging, notwithstanding the reported lower agreement levels between Scheimpflug and colour-LED topography for posterior than for anterior keratometry [26]. Table 4 shows the mean magnitude of posterior corneal astigmatism using Scheimpflug imaging in published studies [20, 27,28,29,30,31,32,33]. Also, we found that posterior corneal astigmatism magnitude is higher in eyes with WTR (0.38 D) than in eyes with ATR SimK astigmatism (0.35 D; p < 0.001). Although the mean magnitude in ATR eyes is similar to that previously reported, in WTR eyes, the mean magnitude in our study was slightly smaller than previously reported [6, 20].
Irrespective of anterior meridian orientation, vertical orientation was the most common for posterior corneal astigmatism. In the whole sample, posterior corneal astigmatism was vertically oriented in 68% of eyes. This value is lower than those previously reported with Scheimpflug-imaging evaluation [6, 15, 20, 34]. However, a recent study by LaHood and Goggin using the IOLMaster 700 (Carl Zeiss Meditec, Jena, Germany), found a similar value for the proportion of eyes with vertical orientation of the posterior steep meridian (73%), with a low ATR prevalence (10%) [35]. WTR was the most frequent orientation of the posterior steep meridian, irrespective of the location of the steep meridian in the anterior surface. This result is in accordance with previous studies, although in eyes with WTR and OBL, the percentage of eyes with vertical orientation of the posterior steep meridian was lower in our study than in a previous study with a Scheimpflug tomographer [36]. Meanwhile, oblique eyes showed higher variability in the orientation of posterior astigmatism and less eyes with the same orientation of posterior astigmatism, which may influence the use of nomograms and the use of vectorial calculation.
In the investigated eyes, 22% showed a posterior corneal astigmatism magnitude of 0.50 D or more. The maximum magnitude was 1.44 D. This percentage is superior to those published in Scheimpflug imaging-based studies and gives further importance to the consideration of the posterior corneal surface when surgically correcting astigmatism [6, 20, 37].
A non-significant positive correlation was found between SimK and posterior corneal astigmatism in WTR eyes (r2 = 0.066; p = 0.371). This correlation was very weak in ATR eyes (r2 = 0.112; p = 0.173) and non-significant in oblique eyes (r2 = −0.019; p = 0.879). These results are in accordance with those previously reported by Koch et al. [6, 20]. In contrast, Tonn et al. found a positive correlation for all subgroups of eyes, although weaker for ATR and oblique than for eyes with WTR astigmatism [36].
The mean difference between SimK and TCA was 0.22 ± 0.17 D. This difference was significantly higher in ATR eyes (0.27 D) than in WTR (0.19 D) and oblique (0.20 D) eyes (p = 0.001). Tonn et al. showed a similar difference for eyes with ATR astigmatism but a lower difference (0.11 D) for eyes with WTR astigmatism. Nevertheless, a difference over 1.00 D was only found in WTR (maximum difference 1.19 D) and oblique eyes (maximum difference 1.04 D). A difference between SimK and TCA ≥ 0.50 D was found in 7% of eyes. This percentage is similar to that previously reported by Tonn et al. [36]. In toric IOL power calculation, if we consider the average pseudophakic human eye, with a ratio between the cylinder at the corneal plane and IOL plane of 1.46, this means we would change the cylindrical power of the implanted IOL (considering 0.75 D steps) in about 7% of the eyes when considering total and not SimK corneal astigmatism.
The mean difference in axis difference between SimK and TCA was 14.81 ± 34.27°, with eyes with SimK ATR astigmatism showing the largest difference (mean 21.07°; p = 0.009). A difference ≥ 10° was found in 24% of eyes. These values are higher than those previously reported in the literature [33, 34]. Savini et al. studied eyes with high to moderate corneal astigmatism (≥1.00 D) with a Scheimpflug camera [34]. In our study, if we consider only this subgroup of eyes, 10% of eyes showed a difference between SimK and TCA ≥ 0.50 D (compared with 16.6% in the study by Savini et al.) and 7% showed a difference in axis ≥ 10°.(compared with 3.8% reported by Savini et al.). While in our study more eyes showed a difference in axis ≥ 10° than in the study by Savini et al. this difference was even more frequent in eyes with SimK astigmatism < 1.00 D, with 40% of eyes showing a difference ≥ 10°. It is important to remember, as toric IOLs are increasingly used, that accurate alignment of the lens inside the eye remains a concern. For each degree of toric IOL misalignment, about 3.3% of the efficacy in cylinder correction is lost [38]. If the lens is 30 degrees off axis, it will negate any correction of astigmatism. Hence, our data supports that considering TCA instead of SimK is mandatory for a precise surgical correction of astigmatism, with this being more evident in eyes with small corneal astigmatism.
In conclusion, our study confirms the previously reported magnitude of posterior corneal astigmatism. However, we found the percentage of eyes with posterior corneal astigmatism of 0.50 D or more to be higher than that previously reported in the literature. Moreover, differences in axis between SimK and TCA were higher than those reported in previous studies. Therefore, this study supports the consideration of TCA magnitude and axis is mandatory for a precise surgical correction of astigmatism.
Summary
What was known before
-
The consideration of TCA magnitude and axis is mandatory for a precise surgical correction of astigmatism.
What this study adds
-
The percentage of eyes with posterior corneal astigmatism superior to 0.5 D and the differences between anterior and TCA are higher than that previously reported in the literature.
References
Ferreira TB, Hoffer KJ, Ribeiro F, Ribeiro P, O’Neill JG. Ocular biometric measurements in cataract surgery candidates in Portugal. PLoS ONE. 2017;12:e0184837.
Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980;90:360–8.
Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014;40:13–9.
Laurendeau C, Lafuma A, Berdeaux G. Modelling lifetime cost consequences of toric compared with standard IOLs in cataract surgery of astigmatic patients in four European countries. J Med Econ. 2009;12:230–7.
Savini G, Næser K. An analysis of the factors influencing the residual refractive astigmatism after cataract surgery with toric intraocular lenses [published correction appears in Invest Ophthalmol Vis Sci. 2015 Apr;56(4):2303]. Investig Ophthalmol Vis Sci. 2015;56:827–35.
Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39:1803–9.
Ninomiya Y, Minami K, Miyata K, Eguchi S, Sato R, Okamoto F, et al. Toric intraocular lenses in eyes with with-the-rule, against-the-rule, and oblique astigmatism: One-year results. J Cataract Refract Surg. 2016;42:1431–40.
Savini G, Næser K, Schiano-Lomoriello D, Ducoli P. Optimized keratometry and total corneal astigmatism for toric intraocular lens calculation. J Cataract Refract Surg. 2017;43:1140–8.
Næser K, Savini G, Bregnhøj JF. Estimating total corneal astigmatism from anterior corneal data. Cornea. 2017;36:828–33.
Piñero DP, Camps VJ, de Fez D, García C, Caballero MT. Validation of posterior corneal curvature measurements with color light-emitting diode topography. Eur J Ophthalmol. 2019;1120672119870738 [Epub ahead of print].
Ribeiro FJ, Ferreira TB, Relha C, Esteves C, Gaspar S. Predictability of different calculators in the minimization of postoperative astigmatism after implantation of a toric intraocular lens. Clin Ophthalmol. 2019;13:1649–56.
Snellenburg JJ, Braaf B, Hermans EA, van der Heijde RG, Sicam VA. Forward ray tracing for image projection prediction and surface reconstruction in the evaluation of corneal topography systems. Opt Express. 2010;18:19324–38.
Holladay JT, Moran JR, Kezirian GM. Analysis of aggregate surgically induced refractive change, prediction error, and intraocular astigmatism. J Cataract Refract Surg. 2001;27:61–79.
Ribeiro F, Castanheira-Dinis A, Dias JM. Refractive error assessment: influence of different optical elements and current limits of biometric techniques. J Refract Surg. 2013;29:206–12.
Li C, Zhang J, Yin X, Li J, Cao Y, Lu P. Distribution and related factors of corneal regularity and posterior corneal astigmatism in cataract patients. Clin Ophthalmol. 2019;13:1341–52.
Pastoura E. Posterior corneal astigmatism and its importance in selection of toric intraocular lens. EC Ophthalmol. 2017;4.5:608–12.
Kohnen T. Posterior corneal astigmatism. J Cataract Refract Surg. 2013;39:1795.
Fityo S, Bühren J, Shajari M, Kohnen T. Keratometry versus total corneal refractive power: analysis of measurement repeatability with 5 different devices in normal eyes with low astigmatism. J Cataract Refract Surg. 2016;42:569–76.
Reitblat O, Levy A, Kleinmann G, Abulafia A, Assia EI. Effect of posterior corneal astigmatism on power calculation and alignment of toric intraocular lenses: comparison of methodologies. J Cataract Refract Surg. 2016;42:217–25.
Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080–7.
Aramberri J, Araiz L, Garcia A, Illarramendi I, Olmos J, Oyanarte I, et al. Dual versus single Scheimpflug camera for anterior segment analysis: precision and agreement. J Cataract Refract Surg. 2012;38:1934–49.
Ferreira TB, Ribeiro P, Ribeiro FJ, O’Neill JG. Comparison of astigmatic prediction errors associated with new calculation methods for toric intraocular lenses. J Cataract Refract Surg. 2017;43:340–7.
Ferreira TB, Ribeiro P, Ribeiro FJ, O’Neill JG. Comparison of methodologies using estimated or measured values of total corneal astigmatism for toric intraocular lens power calculation. J Refract Surg. 2017;33:794–800.
Ferreira TB, Ribeiro FJ. A novel color-LED corneal topographer to assess astigmatism in pseudophakic eyes. Clin Ophthalmol. 2016;10:1521–9.
Ferreira TB, Ribeiro FJ. Comparability and repeatability of different methods of corneal astigmatism assessment. Clin Ophthalmol. 2017;12:29–34.
Lee JH, Lee YW, Lee JS, Knorz MC, Auffarth GU, Choi CY. Comparison of color light-emitting diode corneal topographer and dual rotating scheimpflug-placido topographer. J Ophthalmol. 2018;2018:6764805.
Ueno Y, Hiraoka T, Miyazaki M, Ito M, Oshika T. Corneal thickness profile and posterior corneal astigmatism in normal corneas. Ophthalmology. 2015;122:1072–8.
Zhang L, Sy ME, Mai H, Yu F, Hamilton DR. Effect of posterior corneal astigmatism on refractive outcomes after toric intraocular lens implantation. J Cataract Refract Surg. 2015;41:84–9.
Nemeth G, Berta A, Lipecz A, Hassan Z, Szalai E, Modis L Jr. Evaluation of posterior astigmatism measured with Scheimpflug imaging. Cornea. 2014;33:1214–8.
Preussner PR, Hoffmann P, Wahl J. Impact of posterior corneal surface on toric intraocular lens (IOL) calculation. Curr Eye Res. 2015;40:809–14.
Eom Y, Kang SY, Kim HM, Song JS. The effect of posterior corneal flat meridian and astigmatism amount on the total corneal astigmatism estimated from anterior corneal measurements. Graefes Arch Clin Exp Ophthalmol. 2014;252:1769–77.
Montalbán R, Piñero DP, Javaloy J, Alio JL. Correlation of the corneal toricity between anterior and posterior corneal surfaces in the normal human eye. Cornea. 2013;32:791–8.
Ho JD, Tsai CY, Liou SW. Accuracy of corneal astigmatism estimation by neglecting the posterior corneal surface measurement. Am J Ophthalmol. 2009;147:788–95.e952.
Savini G, Versaci F, Vestri G, Ducoli P, Næser K. Influence of posterior corneal astigmatism on total corneal astigmatism in eyes with moderate to high astigmatism. J Cataract Refract Surg. 2014;40:1645–53.
LaHood BR, Goggin M. Measurement of posterior corneal astigmatism by the IOLMaster 700. J Refract Surg. 2018;34:331–6.
Tonn B, Klaproth OK, Kohnen T. Anterior surface-based keratometry compared with Scheimpflug tomography-based total corneal astigmatism. Investig Ophthalmol Vis Sci. 2014;56:291–8.
Németh J, Erdélyi B, Csákány B. Corneal topography changes after a 15 second pause in blinking. J Cataract Refract Surg. 2001;27:589–92.
Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: correcting astigmatism while controlling axis shift. J Cataract Refract Surg. 1994;20:523–6.
Acknowledgements
This paper was presented at the 24th ESCRS Winter Meeting a presentation with interim findings.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mendes, J., Ribeiro, F.J. & Ferreira, T.B. Evaluation of posterior and total corneal astigmatism with colour-LED topography. Eye 35, 2585–2593 (2021). https://doi.org/10.1038/s41433-020-01278-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01278-z