Abstract
Background
The present study aimed to explore the association between body composition indices, such as fat mass (FM) and lean body mass (LBM), and blepharoptosis.
Methods
The study evaluated 12,168 Korean adults aged 40 years or older using data from the Korea National Health and Nutrition Examination Survey (2008–2011). FM index (FMI, kg/m2) and LBM index (LBMI, kg/m2) were used to correct for the effects of body size. Multivariable logistic regression analysis was performed to investigate the association between blepharoptosis and body composition indices such as FMI, LBMI, and fat percentage of whole body or head. Stratified analyses were also performed by levator function.
Results
Higher FMI and head fat percentage were significantly associated with blepharoptosis (adjusted odds ratio [aOR] = 1.35, 95% confidence interval [CI] = 1.10–1.65; and aOR = 1.32, 95% CI = 1.03–1.69 in the highest tertile compared with the lowest, respectively). In the subgroup with good levator function (≥8 mm), higher FMI, head fat percentage, and head lean mass were significantly associated with blepharoptosis (aOR for the right eye [aORr] = 1.42 and aOR for the left eye [aORl] = 1.36; aORr = 1.41 and aORl = 1.37; and aORr = 1.50 and aORl = 1.49 in the highest tertile compared with the lowest, respectively; all p < 0.05).
Conclusions
Body compositions with high adiposity indices, such as high FMI and head fat percentage, were positively associated with blepharoptosis. Awareness of the potential correlation between obesity-associated fat deposition and blepharoptosis could improve management of the condition and contribute to understanding the pathogenesis of blepharoptosis.
Similar content being viewed by others
Introduction
Blepharoptosis is a common condition defined as an abnormally low-lying upper eyelid margin, with a prevalence of 13.5% in the Korean population over 40 years of age, which further advances with age, reaching a prevalence of up to 30% in those aged 70 years or older [1]. Blepharoptosis sometimes occurs in isolation but can also be a clinical manifestation of other health conditions, such as neurological, immunological, cerebral, and vascular disorders [2]. Blepharoptosis is classified as being either congenital or acquired based on its onset [3]. Acquired blepharoptosis is further categorised into myogenic, neurogenic, aponeurotic, mechanical, or traumatic type based on its aetiology. Among the types of acquired blepharoptosis, aponeurotic blepharoptosis, also known as involutional ptosis, is the most prevalent, and ordinarily presents in late adulthood [4].
The pathogenesis of aponeurotic blepharoptosis is most often due to involutional changes, such as gradual stretching or dehiscence, in the levator aponeurosis [2, 5]. Even in severe cases, the function of the levator muscle itself can be preserved [6]. A retrospective study in Taiwan reported that 77.1% of ptotic eyelids have good levator function [7]. Another study revealed that levator function of eyelids with aponeurotic blepharoptosis is as strong as that of normal eyelids, while levator function of eyelids with myogenic or neurogenic blepharoptosis is weaker than that of normal eyelids [8]. Histologically, significant fatty infiltration of the levator muscle/aponeurosis and Müller’s muscle was primarily observed in eyelids with aponeurotic blepharoptosis, which is associated with stretching or dehiscence of the levator aponeurosis [9].
Several epidemiological studies have suggested a potential association between blepharoptosis and general body condition, especially obesity [10,11,12,13]. These prior studies evaluated obesity using body mass index (BMI), waist circumference (WC), or body fat percentage, and demonstrated that obesity and blepharoptosis are positively associated [10]. Although BMI is widely used to identify the presence of obesity, this index is not able to differentiate between fat mass (FM) and lean body mass (LBM). To the best of our knowledge, no prior report has evaluated the potential association between blepharoptosis and body composition indices such as FM and LBM. Because FM and LBM could have different effects on health outcomes [14, 15], the present study aimed to investigate the potential association between blepharoptosis and various body composition indices using data from the Korea National Health and Nutrition Examination Survey (KNHANES).
Materials and methods
Study population
Data from 2008 to 2011 in the KNHANES were used. The KNHANES, conducted by the Korea Center for Disease Control and Prevention, is a nationwide, representative cross-sectional survey using a clustered, multistage, stratified, and probability-sampling design. The survey includes demographic, socioeconomic, medical, and dietary information [16]. Ophthalmologic interviews and examinations have been conducted as a part of the survey since 2008 [17].
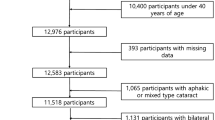
In the present study, we initially included 16,109 participants aged 40 years or older, taking into account the high prevalence of aponeurotic blepharoptosis in older adults. In addition, we excluded subjects with thyroid disease (n = 374) or facial palsy after stroke (n = 45) that could affect the position or motility of the upper eyelid. We also excluded 3522 subjects without adequate data regarding body composition or blepharoptosis. Finally, 12,168 participants that had undergone both ophthalmologic examination and dual-energy X-ray absorptiometry (DXA) to examine body composition were included. This survey was reviewed and approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C and 2011-02CON-06-C), and all participants provided written informed consent prior to beginning the survey. This work was carried out following the tenets of the Declaration of Helsinki.
Assessment of blepharoptosis
Ophthalmologic examinations were performed by ophthalmologists affiliated with the Korean Ophthalmologic Society. Marginal reflex distance 1 (MRD1) was measured as follows: After positioning the participant’s eye at the physician’s eye level, the participant was asked to look straight and relax while focusing on a distant target. When the physician shone a penlight into the participant’s eye, the distance from the corneal light reflex to the upper eyelid margin was measured in millimetres [17]. Blepharoptosis was defined as an MRD1 in primary position of <2 mm in either eye [16, 18].
Levator function was calculated by measuring the distance between the upper eyelid excursion from full downgaze to full upgaze without frontalis muscle contraction. Participants were divided into two groups for stratified analysis, with either good levator function (≥8 mm) or fair levator function (<8 mm) [4].
Anthropometric measurements and body composition analyses
Body weight, height, and WC were measured to the nearest 0.1 kg, 0.1 cm, and 0.1 cm, respectively, with subjects wearing light clothing and without shoes. BMI was calculated as weight (kg) divided by squared height (m2). Body components, including FM, LBM, and fat percentage, were measured using a DXA scanner (QDR 4500A, Hologic Inc., Waltham, MA, USA). FM and LBM were respectively converted to FM index (FMI: FM [kg] divided by height [m2]) and LBM index (LBMI: LBM [kg] divided by height [m2]) to correct for the effect of body size [19], as FM and LBM are largely determined by height [20]. FMI and LBMI were initially proposed as body composition indices normalised to height for nutritional assessment [21]. In the present study, FMI, LBMI, and fat percentage were divided into sex-specific tertiles with tertile 1 as the lowest, and tertile 3 as the highest. The first tertile was set as the reference. For head lean mass, we excluded contribution of bone mass by subtracting head bone mass from head lean mass, such that head lean mass could be used as a proxy for head muscle mass.
Covariates
Smoking status was categorised as non-smoker or current smoker based on a self-reported questionnaire. Regular physical activity was defined as performing strenuous exercise for more than 20 min at least 3 days per week. Hypertension was defined as mean systolic blood pressure ≥140 mm Hg, mean diastolic blood pressure ≥90 mm Hg, or an affirmative survey response to taking antihypertensive medicine. Diabetes was defined as fasting blood glucose ≥126 mg/dL, or an affirmative survey response to taking hypoglycaemic agents or having a history of physician-diagnosed diabetes. The presence of strabismus was assessed using the cover-uncover test, prism and alternate cover test, and/or Krimsky test. Strabismus was defined as a manifest or latent ocular deviation at distance or near fixation, including esodeviation ≥10 prism dioptres, exodeviation ≥15 prism dioptres, or any vertical deviation.
Statistical analysis
All statistical analyses were conducted using Stata version ver. 14.1 (Stata Corp, College Station, TX). To reflect nationally representative prevalence estimates, weights were assigned to each subject to allow an equal probability for sampling. A two-sided P value < 0.05 was considered to be statistically significant. Baseline characteristics of participants according to the presence or absence of blepharoptosis are presented as mean ± standard error (SE) for continuous variables, or as proportions (%) for categorical variables. Student’s t tests and Chi-square tests were conducted to compare differences in participant characteristics between participants with and without blepharoptosis. Multivariable logistic regression analyses were performed to explore the strength of the association between body composition and blepharoptosis. Model 1 was adjusted for age and sex, model 2 was adjusted for smoking status and physical activity levels in addition to age and sex, and model 3 was furthermore adjusted for hypertension, diabetes, and strabismus. Model 4 was mutually adjusted for LBMI and FMI to investigate the independent associations of each variable. For example, LBMI was examined in relation to blepharoptosis with an additional adjustment for FMI, and vice versa. Body fat percentage and head fat percentage were additionally adjusted for BMI and head weight, respectively, in model 4. In a stratified analysis by levator function, we fully adjusted for all variables included in model 4.
Results
Baseline characteristics
All baseline characteristics and their association with blepharoptosis are shown in Table 1. The mean age of the study population was 55.3 years (SE, 0.2), and females comprised 51.4% of the participants. In total, 14.1% of the participants had blepharoptosis. Participants with blepharoptosis were more likely to have higher BMI, WC, and body fat percentage (all p values < 0.001). LBMI was not associated with blepharoptosis (p = 0.917), but FMI was higher in participants with blepharoptosis than in participants without blepharoptosis (7.0 vs 6.7 kg/m2, p < 0.001). Higher head fat percentage and lower head lean mass were associated with the presence of blepharoptosis (all p values < 0.001).
Association between body composition and blepharoptosis
The association between whole body composition and blepharoptosis was analysed using multivariable logistic regression, as shown in Table 2. Increased BMI (adjusted odds ratio [aOR] = 1.05, 95% confidence interval [CI] = 1.03–1.07, p < 0.001) and WC (aOR = 1.02, 95% CI = 1.01–1.03, p < 0.001) were associated with blepharoptosis in model 3. Body fat percentage was not significantly associated with blepharoptosis after additional adjustment for BMI in model 4 (aOR = 1.14, 95% CI = 0.89–1.46 in the highest tertile compared with the lowest, p = 0.333). Higher LBMI was significantly associated with blepharoptosis in model 3 (aOR = 1.25, 95% CI = 1.06–1.48 in the highest tertile compared with the lowest, p = 0.009), but the association in model 4 became insignificant after mutual adjustment for FMI (aOR = 1.13, 95% CI = 0.93–1.38, p = 0.207). By contrast, higher FMI was significantly associated with blepharoptosis in model 4, even after mutual adjustment for LBMI (aOR = 1.35, 95% CI = 1.10–1.65 in the highest tertile compared with the lowest, p = 0.005).
The associations between head composition and blepharoptosis was analysed using multivariable logistic regression analysis, and is shown in Table 3. Higher head fat percentage was significantly associated with blepharoptosis in model 4 independent of total head weight (aOR = 1.32, 95% CI = 1.03–1.69 in the highest tertile compared with the lowest, p = 0.027). In model 4, the associations between head LM and head FM and blepharoptosis were insignificant (all p values > 0.05).
Stratification by levator function
In Table 4, we conducted stratified analyses by levator function categories for each eye with mutual adjustment. In the subgroup with good levator function (≥8 mm), higher FMI was significantly associated with blepharoptosis (aOR = 1.42, 95% CI = 1.14–1.77 in the highest tertile for the right eye, p = 0.002; and aOR = 1.36, 95% CI = 1.09–1.71 in the highest tertile for the left eye, p = 0.007). However, LBMI and body fat percentage were not significantly associated with blepharoptosis in the subgroup with good levator function.
In the subgroup with good levator function (≥8 mm), higher head lean mass and head fat percentage were significantly associated with blepharoptosis, but head FM was not significantly associated with blepharoptosis: (1) head lean mass (aOR = 1.50, 95% CI = 1.04–2.15 in the highest tertile for the right eye, p = 0.029; and aOR = 1.49, 95% CI = 1.04–2.14 in the highest tertile for the left eye, p = 0.032); and (2) head fat percentage (aOR = 1.41, 95% CI = 1.08–1.85 in the highest tertile for the right eye, p = 0.013; and aOR = 1.37, 95% CI = 1.06–1.78 in the highest tertile for the left eye, p = 0.018). In the subgroup with fair levator function (<8 mm), none of the body composition indices were significantly associated with blepharoptosis.
Discussion
In the present study, we identified that obesity and body composition were significantly associated with blepharoptosis. Among general obesity indices, blepharoptosis was significantly associated with higher BMI and WC. Among whole body or head composition indices, blepharoptosis was significantly associated with higher head fat percentage and higher FMI, independent of LBMI. In a stratified analysis only for presumed aponeurotic blepharoptosis with good levator function (≥8 mm) [4], blepharoptosis was significantly associated with higher FMI, head fat percentage, and head lean mass.
Only a few prior studies have evaluated the association between blepharoptosis and general obesity or body composition [10, 11]. Paik et al. investigated the association between blepharoptosis and obesity indices including BMI, WC, and body fat percentage in 10,285 adults aged 40 years or older [10]. Paik et al. demonstrated that each index was significantly associated with blepharoptosis prevalence and severity. Koh et al. evaluated the association between blepharoptosis and metabolic syndrome determined by WC, hypertension, and blood chemistry, and also found that blepharoptosis was associated with WC and other obesity indices [11]. Consistent with prior studies, the present study demonstrated that higher BMI and WC were associated with blepharoptosis, suggesting that general obesity could be a potential risk factor for blepharoptosis. However, unlike the study by Paik et al. [10], the present study found that body fat percentage was not significantly associated with blepharoptosis after adjusting BMI in model 4. Additional adjustment for BMI to reflect body size [22] in the present study could account for this inconsistency between studies.
The present study was designed to investigate body composition indices as potential risk factors for blepharoptosis in addition to traditional obesity indices. In this study, higher FMI and head fat percentage were associated with blepharoptosis in adults aged 40 years or older. Although the underlying mechanism is unclear, these two indices reflect obesity, especially adiposity. Peltz et al. suggested that FMI, as a selective measure of adiposity, is in some cases a more accurate index for obesity than BMI, based on the observation of a large discrepancy (9.2–32.8%) between BMI and body fat percentage for defining obesity [23]. Obesity, represented by high FMI, may induce insulin resistance and chronic inflammation driven by both obesity itself and obesity-related comorbidities [24]. Shirado reported that dyslipidemia is associated with blepharoptosis (odds ratio = 4.01) in a study of 251 subjects aged 60 years or older [25]. This study suggested that obesity-related dyslipidemia can impair microvascular blood flow to the eyelids, subsequently inflicting hypoxic damage on the upper eyelid retractor, which could cause degenerative changes and fatty infiltration of the upper eyelid retractors [25].
Head fat percentage, another potential risk factor, is more likely to reflect the fat distribution around the orbit compared with other body fat indices such as whole-body fat percentage or head FM. In obese subjects, hypertrophy of the preaponeurotic fat or retro-orbicularis oculi fat (ROOF) could develop, and heavy loads on the levator can adversely affect the margin level and retractor efficacy of the upper eyelid. Paik et al. also speculated that increased fat volume could increase downward mechanical pressure on the upper eyelid [10]. Intense stretching of the levator aponeurosis due to increased fat burden, combined with tissue damage resulting from microvascular impairment, could cause detachment or dehiscence of the aponeurosis, which could contribute to aponeurotic blepharoptosis.
Paik et al. described that a limitation of their study regarding the association between obesity and involutional blepharoptosis was that levator function was not considered, and therefore that various types of blepharoptosis other than aponeurotic blepharoptosis were also included in the analysis [10]. Because aponeurotic ptosis is known to present with good levator function of 8 mm or larger, we conducted separate analyses for subgroups with good (≥8 mm) and fair (<8 mm) levator function in each eye. Interestingly, FMI (aOR = 1.42 for the right and 1.36 for the left) and head fat percentage (aOR = 1.41 for the right and 1.37 for the left) were significant risk factors for blepharoptosis in the good levator function group, but were insignificant in the fair levator function group. These findings suggest that adiposity is associated only with aponeurotic blepharoptosis, but not with other types of blepharoptosis.
Most prior studies evaluating the relationships between obesity and blepharoptosis have focused on the harmful effects of obesity and body fat, while neglecting the effect of LBM, a counterpart of FM [10,11,12,13]. In the present study, the positive association between LBMI and blepharoptosis was statistically insignificant after mutual adjustment for FMI, suggesting that the positive association of LBMI with blepharoptosis could be due to the confounding effect of FMI, as obese subjects tend to have high muscle mass as well as high FM [26]. Unlike LBM/LBMI, higher head lean mass was associated with blepharoptosis, independent of head FM, in stratified analysis for the subgroup with good levator function. Although lean mass is generally thought to have favourable effects on health outcomes for conditions such as insulin resistance [27], some studies suggested that LBM had unfavourable effects on some conditions such as osteoarthritis and hypertension [28, 29]. A prior study suggested that increased mechanical loading on the joints by skeletal muscle mass could be related to its negative impact on osteoarthritis [28]. Similarly, higher head lean mass could impair the levator aponeurosis by increasing mechanical loading. However, further studies are needed to verify that head lean mass has an unfavourable impact on blepharoptosis.
The present study has several limitations that should be acknowledged to avoid its overinterpretation. First, we cannot clarify causality due to the inherent nature of the cross-sectional study design. However, it is unlikely that blepharoptosis causes high FMI or head fat percentage, rather than the reverse. Second, we could not classify blepharoptosis subtype, and lacked information regarding whether the subjects had a prior history of surgical interventions for blepharoptosis. However, the present study used large-scale data from a representative Korean population, and excluded subjects with possible neurologic or mechanical aetiologies of blepharoptosis. Furthermore, we performed stratified analyses by category according to levator function to address aponeurotic blepharoptosis. Third, our findings might not be generalisable, as we included only Korean subjects, and eyelid structure varies between ethnicities. Further replicative studies in Western countries are needed.
In conclusion, high adiposity traits, such as high FMI and high head fat percentage, were positively associated with the presence of blepharoptosis in adults, and these findings suggested that obesity-associated fat deposition is a possible risk factor for blepharoptosis in older adults. In addition, we uncovered a potentially unfavourable role for head lean mass in blepharoptosis, which should be explored in future studies. Further studies are needed to evaluate whether obesity control could prevent blepharoptosis.
Summary
What was known before
-
Obesity has been suggested as the pathogenesis of blepharoptosis.
-
However, studies on the relationship between body composition and blepharoptosis are insufficient.
What this study adds
-
In this cross-sectional study, the higher FM index and head fat percentage were significantly associated with blepharoptosis.
-
Awareness of the potential correlation between obesity-associated fat deposition and blepharoptosis could improve understanding of the pathogenesis of blepharoptosis.
References
Kim MH, Cho J, Zhao D, Woo KI, Kim YD, Kim S, et al. Prevalence and associated factors of blepharoptosis in Korean adult population: the Korea National Health and Nutrition Examination Survey 2008-2011. Eye (Lond, Engl). 2017;31:940–6.
Pimentel de Figueiredo AR. Blepharoptosis. Semin Ophthalmol. 2010;25:39–51.
Sakol PJ, Mannor G, Massaro BM. Congenital and acquired blepharoptosis. Curr Opin Ophthalmol. 1999;10:335–9.
Lee YG, Son BJ, Lee KH, Lee SY, Kim CY. Clinical and Demographic Characteristics of Blepharoptosis in Korea: a 24-year Experience including 2,328 Patients. Korean J Ophthalmol. 2018;32:249–56.
Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003;27:193–204.
Pauly M, Sruthi R. Ptosis: evaluation and management. Kerala J Ophthalmol. 2019;31:11–6.
Lai HT, Weng SF, Chang CH, Huang SH, Lee SS, Chang KP, et al. Analysis of Levator Function and Ptosis Severity in Involutional Blepharoptosis. Ann Plast Surg. 2017;78:S58–s60.
Frueh BR, Musch DC. Evaluation of Levator Muscle Integrity in Ptosis with Levator Force Measurement. Ophthalmology. 1996;103:244–50.
Shore JW, McCord CD. Anatomic Changes in Involutional Blepharoptosis. Am J Ophthalmol. 1984;98:21–27.
Paik JS, Jung SK, Han KD, Kim SD, Park YM, Yang SW. Obesity as a Potential Risk Factor for Blepharoptosis: the Korea National Health and Nutrition Examination Survey 2008-2010. PloS ONE. 2015;10:e0131427.
Koh C, Kim G, Han K, Park J. Association between metabolic syndrome and blepharoptosis in the Korean adults: the Korea National Health and Nutrition Examination Survey 2010–2012. J Cosmet Med. 2018;2:85–90.
Satariano N, Brown MS, Zwiebel S, Guyuron B. Environmental factors that contribute to upper eyelid ptosis: a study of identical twins. Aesthetic Surg J. 2015;35:235–41.
Cho B-J, Choi YJ, Shin MC, Yang S-W, Lee MJ. Prevalence and risk factors of childhood blepharoptosis in Koreans: the Korea National Health and Nutrition Examination Survey. Eye. 2019;2020;34:1585–91.
Han SS, Kim KW, Kim KI, Na KY, Chae DW, Kim S, et al. Lean mass index: a better predictor of mortality than body mass index in elderly Asians. J Am Geriatrics Soc. 2010;58:312–7.
Medina‐Inojosa JR, Somers VK, Thomas RJ, Jean N, Jenkins SM, Gomez‐Ibarra MA et al. Association between adiposity and lean mass with long‐term cardiovascular events in patients with coronary artery disease: no paradox. J Am Heart Assoc. 2018;7:e007505.
Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014;43:69–77.
Yoon KC, Mun GH, Kim SD, Kim SH, Kim CY, Park KH, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011;25:421–33.
Small RG, Sabates NR, Burrows D. The measurement and definition of ptosis. Ophthalmic Plast reconstructive Surg. 1989;5:171–5.
Weber DR, Leonard MB, Shults J, Zemel BS. A comparison of fat and lean body mass index to BMI for the identification of metabolic syndrome in children and adolescents. J Clin Endocrinol Metab. 2014;99:3208–16.
Lee DH, Keum N, Hu FB, Orav EJ, Rimm EB, Willett WC, et al. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: prospective US cohort study. BMJ. 2018;362:k2575–k2575.
VanItallie TB, Yang MU, Heymsfield SB, Funk RC, Boileau RA. Height-normalized indices of the body’s fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr. 1990;52:953–9.
Bradbury KE, Guo W, Cairns BJ, Armstrong MEG, Key TJ. Association between physical activity and body fat percentage, with adjustment for BMI: a large cross-sectional analysis of UK Biobank. BMJ Open. 2017;7:e011843–e011843.
Peltz G, Aguirre MT, Sanderson M, Fadden MK. The role of fat mass index in determining obesity. Am J Hum Biol: Off J Hum Biol Counc. 2010;22:639–47.
Vekic J, Zeljkovic A, Stefanovic A, Jelic-Ivanovic Z, Spasojevic-Kalimanovska V. Obesity and dyslipidemia. Metabolism. 2019;92:71–81.
Shirado M. Dyslipidaemia and age-related involutional blepharoptosis. J Plast, Reconstructive Aesthetic Surg. 2012;65:e146–150.
Ye S, Zhu C, Wei C, Yang M, Zheng W, Gan D, et al. Associations of Body Composition with Blood Pressure and Hypertension. Obes (Silver Spring, Md). 2018;26:1644–50.
Srikanthan P, Karlamangla AS. Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third National Health and Nutrition Examination Survey. J Clin Endocrinol Metab. 2011;96:2898–903.
Visser AW, de Mutsert R, Loef M, le Cessie S, den Heijer M, Bloem JL, et al. The role of fat mass and skeletal muscle mass in knee osteoarthritis is different for men and women: the NEO study. Osteoarthr Cartil. 2014;22:197–202.
Julius S, Majahalme S, Nesbitt S, Grant E, Kaciroti N, Ombao H, et al. A “gender blind” relationship of lean body mass and blood pressure in the Tecumseh study*. Am J Hypertension. 2002;15:258–63.
Author information
Authors and Affiliations
Contributions
Conception and design: CL, SMJ, HSS. Data acquisition: SMJ. Data analysis and interpretation: CL, SMJ, HSS. Writing, review, and/or revision of the paper: CL, SMJ, HSS. Study supervision: SMJ, HSS.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, C., Jeong, SM. & Sa, HS. Correlation between body composition and blepharoptosis in adults. Eye 35, 1999–2007 (2021). https://doi.org/10.1038/s41433-020-01214-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01214-1
This article is cited by
-
Sarcopenia as a potential risk factor for senile blepharoptosis: Nationwide Surveys (KNHANES 2008–2011)
Scientific Reports (2023)