Abstract
Background
The association between retinal microvascular structure and glaucoma has been revealed in multiple studies using optical tomography angiography (OCTA), but limited information on the macular vessel density (mVD) in patients with glaucoma is available. In this study, we tried to identity the factors that affected macular VD (mVD) in glaucomatous eyes.
Methods
This retrospective cross-sectional study evaluated OCT and OCTA images from 92 eyes from 58 healthy subjects and 179 eyes from 103 glaucoma patients using the SD-OCT database from July 2017 to July 2018. Glaucomatous eyes were further divided into two groups according to history of disc haemorrhage (DH). Association between mVD and demographic characteristics, ganglion cell-inner plexiform layer (GCIPL) thickness, visual field mean deviation (MD) and systemic blood pressure was analysed in each group.
Results
In both healthy and glaucomatous eyes, mVD was inversely associated with age (β = −0.035, P = 0.025; β = −0.039, P = 0.018). In the glaucomatous eyes, mVD was significantly decreased, as the MD value was worse (β = 0.109, P = 0.002). In glaucomatous eyes with DH, mVD decreased as blood pressure increased (β = -0.111, P = 0.003)
Conclusions
Reduced mVD is more common in older individuals in both healthy and glaucomatous eyes, and correlates with functional deterioration than structural damage in glaucomatous eyes. In glaucomatous eyes with DH, high systemic BP is associated with a reduction in mVD. This may indicate that glaucoma patients with DH are more susceptible to vascular damage secondary to hypertension
Similar content being viewed by others
Introduction
Optical coherence tomography angiography (OCTA) has recently been spotlighted as a technology capable of noninvasively evaluating microvascularity across various retinal layers with good reproducibility [1,2,3]. Since the first report of decreased optic nerve head (ONH) perfusion in glaucoma using OCTA [4], multiple studies have demonstrated reduced peripapillary or ONH [1, 2, 5,6,7,8] and macular [9,10,11,12,13,14] perfusion in glaucoma patients via OCTA. Early OCTA studies focused on primary insult sites in glaucoma (e.g., ONH and peripapillary region). Recent macular vascular structure studies have also reported various findings. The reasons why these studies have focused on the macular vessel density (mVD) in glaucoma and impressive findings about mVD are as follows. First, glaucomatous optic neuropathy results in retinal ganglion cell (RGC) loss. The macula is among the most metabolically active eye tissues [15, 16] and includes half of all RGCs [17, 18], which depend on regional retinal capillary networks to meet their high metabolic requirements. Therefore, mVD can be an important factor affecting the viability of damaged RGCs in glaucoma. Second, there is an increasing body of evidence that mVD is a good reflection of functional loss and structural macular thinning [12, 13]. Third, serial OCTA measurements reveal glaucomatous change with mVD in eyes without evidence of altered ganglion cell complex thickness [11]. This suggests the possibility that changes of mVD may occur prior to structural changes in ganglion cell layer in glaucoma. Therefore, macular vascular indexing using OCTA may play a pivotal role in understanding and evaluating the glaucoma progression.
The purpose of the current study was to investigate factors, especially systemic blood pressure (BP), which may affect mVD in healthy and glaucomatous eyes. We also performed subgroup analyses of mVD categorized based on their history of disc haemorrhage (DH).
Materials and methods
Study design and subjects
This study adhered to the tenets of the Declaration of Helsinki, and Institutional Review Board approval was obtained at the Severance Hospital (4-2019-0371). Patients identified in the spectral domain optical coherence tomography (SD-OCT) database who had been treated from July 2017 to July 2018 in the glaucoma unit of Severance Hospital of Yonsei University were examined. This retrospective observational cross-sectional study included 92 eyes from 58 healthy subjects and 179 eyes from 103 patients with a definitive diagnosis of open-angle glaucoma (primary open-angle glaucoma, pigment dispersion glaucoma, pseudoexfoliative glaucoma, or preperimetric glaucoma).
Glaucoma was diagnosed based on a clinical examination demonstrating a defective optic nerve rim (notching or localized thinning), which is characteristic of glaucoma. Retinal nerve fibre layer (RNFL) thickness and OCT deviation maps (CirrusTM HD-OCT 5000; Zeiss, Dublin, CA) were reviewed in all patients. All glaucoma cases demonstrated focal RNFL thinning consistent with funduscopic disc findings. For perimetric glaucoma, Humphrey Swedish Interactive Threshold Algorithm 24-2 visual fields had at least one of the following three characteristics: (1) a glaucoma hemifield test outside normal limits, (2) pattern standard deviation outside normal limits (P < 0.05), or (3) a cluster of three or more adjacent points in locations characteristic of glaucoma, all of which were reduced on the pattern deviation plot at a P value of < 5%. Preperimetric glaucoma eyes had an optic nerve rim defect, consistent OCT findings, and no qualifying VF findings. If all of the above conditions were met and pseudoexfoliation and pigment dispersion were suspected on both slit-lamp and gonioscopic examinations, the appropriate diagnosis was made.
As a healthy subject, we included those who were diagnosed as not having glaucoma among those who wanted to be screened for glaucoma. Healthy subjects in the present study had normal clinical examination results, including non-glaucomatous optic discs and an intraocular pressure (IOP) of 21 mmHg or less. Inclusion criteria for both the glaucoma and healthy groups was an age of 18 years and older. Exclusion criteria included known spherical refractive error greater than +6.00 dioptres or less than −9.00 dioptres, macular or other retinal or optic nerve disease, history of ocular trauma or ocular surgery other than uncomplicated cataract and glaucoma surgery, and OCT signal strength of 6 or less (out of 10).
Demographic information collected from the patient medical records included age, sex, IOP, systolic and diastolic BP, diagnosis of diabetes or hypertension, history of DH, VF mean deviation (MD), and visual field index score. Within 4 h on the same day when OCT and OCTA were performed, all subjects underwent slit-lamp biomicroscopy, IOP measurement using Goldman applanation tonometry, and systemic BP measurement using an automated BP metre. Patients’ BP was taken while seated after waiting 20 min in a waiting room. The same automated BP monitor was used in the clinic to reduce variability owing to instrument differences or cuff size. The mean arterial pressure (MAP) was calculated as MAP = 1/3 systolic BP + 2/3 diastolic BP.
To confirm the presence of DH, only glaucoma patients who were managed for 3 years or more were included. If DH was confirmed in the corresponding eye within the previous 3 years of medical records, the subject was classified as being DH positive. Most of patients had VF test (Humphrey Field Analyzer II 24-2; Zeiss) on the same day as the OCTA test. If the test dates were different, the VF test performed on the date closest to the OCTA test was used for analyses.
OCT image acquisition
All subjects underwent OCT imaging of the ganglion cell-inner plexiform layer (GCIPL) thickness (CirrusTM HD-OCT 5000; Zeiss) and OCT angiography imaging (Zeiss AngioPlex® OCT Angiography powered by CirrusTM HD-OCT 5000). Macular Cube 6 × 6 mm scan protocol for GCIPL evaluation was acquired. Rather than 3 × 3 mm (about ±4.95° from the foveal centre) volumetric scans, 6 × 6 mm (about ± 9.9° from the foveal centre) ones were used [19] as the thickest portion of the RGC layer lies within ± 8° of the foveal centre [20, 21]. Mean GCIPL thickness is based on ganglion cell analysis of an area outlined by two ellipsoids. The outer ellipsoid has a vertical diameter of 4 mm and a horizontal diameter of 4.8 mm and the inner blacked out ellipsoid has a vertical diameter of 1 mm and a horizontal diameter of 1.2 mm around the fovea. The AngioPlex® OCTA technology used the optical microangiography-complex algorithm to analyse changes in the complex signal (both intensity and phase changes within sequential B-scans performed at the same position) [22, 23] and then generate en face microvascular images in a 6 × 6 mm region. Vascular images of the superficial and deep layers of the retina are displayed separately. Boundaries of the superficial and deep retinal layer slab were automatically determined. The inner surface of the superficial retinal layer (SRL) was defined by the internal limiting membrane (ILM). The outer surface of the SRL was an approximation of the inner plexiform layer (IPL), where the IPL was estimated to be 70% of the thickness between the ILM and retinal pigmented epithelium. The segmentation software automatically detected retinal layer boundaries from structural OCT cross-sectional images by measuring the OCT signal gradients and creating SRL en face images of the macular regions. The AngioPlex® OCTA technology includes software that automatically analyses mVD percentage data in the SRL and divides mVD scans into three areas: (1) a central circle mVD (≤1 mm), (2) an inner circle mVD (1–3 mm), and (3) an outer circle mVD (3–6 mm). Total mVD values for the whole scan area were used in subsequent analyses. The AngioPlex® incorporates FastTrac retinal-tracking technology to reduce motion artefacts. All scans were individually reviewed by one glaucoma specialist to assess image quality (i.e., signal strength, segmentation error, loss of fixation, motion artefact, and media opacity). Substandard scans were excluded.
Statistical analyses
Data were imported into SPSS 23.0 (SPSS Inc., Chicago, IL, USA) for further statistical analyses. Normal distribution of the data was checked using the Kolmogorov–Smirnov test and Q-Q plot. Data were expressed as mean ± standard deviation (SD) for Gaussian distributed values. Independent t tests were used to compare differences in continuous variables between the two groups. F test was performed prior to independent t test and indicated that the data had the equality of variance across the group. Exact chi-square tests were used to test differences between categorical variables. Correlations between mVD percentage data and demographic factors, systemic BP, and eye-specific parameters were evaluated using multiple linear regression analyses. Multivariate linear regression modelling was performed, adjusting significant variables with reference to the univariate linear regression results. P values < 0.05 were considered statistically significant.
Results
Of 557 eyes from 286 patients who underwent OCT and OCTA macula imaging, 179 eyes from 103 glaucoma patients and 92 healthy eyes from 58 control subjects met our inclusion and exclusion criteria after exclusion owing to poor image quality, as per the conditions described above. Table 1 summarizes the baseline characteristics of the study subjects. There were significant differences in the ages and prevalence of hypertension between the healthy and glaucomatous eyes.
Simple linear regression analysis was performed for the effect of each factor on mVD and multiple linear regression analysis of mVD was obtained based on age, MAP, MD and GCIPL thickness. This multivariate model was chosen on the basis of results of simple linear regression analysis in each controls, glaucoma group and subgroup of glaucoma. Any factors that appeared significance in simple linear regression were included for multivariate analysis.
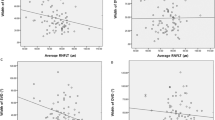
In the healthy eyes, univariate analyses revealed that age, MD, and GCIPL thickness were significantly associated with mVD. (Table 2). The multivariate analyses revealed that age was the only factor that was significantly and inversely associated with mVD in healthy eyes (β = −0.033, P = 0.045).
In glaucomatous eyes, age, MD, and GCIPL thickness were associated with mVD, similar to that observed in healthy eyes (Table 3). In the multivariate analyses, age retained an inverse association with mVD (β = −0.040, P = 0.018). In addition, MD was significantly associated with mVD (β = 0.107, P = 0.002). This association was stronger than that with age.
We performed subgroup analyses depending on the history of DH in the corresponding eyes. There was no significant difference between the two subgroups except for IOP (Table 4). The average IOP was slightly lower in the glaucomatous eyes with DH than in those without DH (mean ± SD; 13.4 ± 4.12 vs. 15.1 ± 3.93, P = 0.010). In glaucomatous eyes without DH, linear regression analyses revealed generally similar results to those in glaucomatous eyes. In glaucomatous eyes without DH, mVD was significantly associated with age, MD, and GCIPL thickness in the univariate analyses and with MD in the multivariate analyses (β = 0.121, P = 0.004; Table 5).
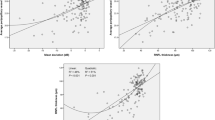
In glaucomatous eyes with DH, MAP was significantly associated with mVD in the univariate and multivariate analysis (β = −0.105, P = 0.003; β = −0.111, P = 0.003, respectively; Table 5). After adjusting for age, MD, and GCIPL thickness, the association between MAP and mVD was maintained in the multivariate analysis. Simple linear regression between MAP and mVD in glaucomatous eyes without and with DH is represented in Fig. 1. Figure 2 is a scatterplot between MAP and predicted mVD obtained from multivariate analysis adjusting compounding factors like age, MD and GCIPL thickness, so it can show the independent relationship between MAP and mVD. When compounding factors were adjusted, the inverse relationship between mVD and MAP became stronger in glaucoma group with DH.
Discussion
In the present study, we investigated the relationship between multiple clinical parameters and superficial mVD, detected using OCTA, in healthy eyes and glaucomatous eyes. The factors associated with mVD in healthy and glaucomatous eyes were mostly consistent with those reported in prior OCTA-based studies specified below. Here, age was associated with mVD in both healthy and glaucomatous eyes. In particular, age appeared to be an important factor associated with macular blood flow in the multivariate linear regression. In healthy eyes, most studies have shown that mVD decreases with increasing age [11, 13, 14, 24,25,26,27]. Only Gadde et al. [28] reported that age did not affect superficial capillary VD. A relatively small sample size (n = 18) may partially explain differences in these results. In glaucomatous eyes, Wu et al. [13] and Lommatzsch et al. [14] found a significant negative association between age and VD. Furthermore, Shoji et al. [11] reported that the rate of mVD decline accelerated with an increasing age.
We also found that in glaucomatous eyes, mVD was strongly associated with VF MD in the multivariate analysis. OCT structural parameters such as GCIPL and functional parameters such as VF MD values have also been found to correlate with mVD [12,13,14]. In all three studies, mVD had a slightly stronger association with the ganglion cell complex than VF parameters. These studies used AngioVue™ OCTA (RTVue-XR; Optovue, Inc., Fremont, CA, USA) and a different analysis method than that used here. These factors may have led to differences with the current study. Furthermore, decreased VD is significantly associated with functional loss severity, independent of structural loss [29, 30]. A recent study using AngioPlex™ OCTA further demonstrated that mVD was more robustly associated with functional measures of glaucoma than structural ones [31]. Therefore, future studies on the relationship between VD and OCT-structural and functional parameters are needed.
Subgroup analyses revealed that glaucomatous eyes without DH were similar to all eyes with glaucoma. In contrast, MAP was the only factor that was significantly associated with mVD in glaucomatous eyes with DH. After adjusting for age, GCIPL thickness, and VF MD, MAP retained a negative correlation with mVD.
Retinal circulation is autoregulated, meaning that within a certain range, flow is independent of perfusion pressure [32,33,34,35]. Furthermore, the autoregulation of blood supply to the ONH may be less efficient than that to the retina but more efficient than that to the choroid [36,37,38,39]. In glaucoma patients, this retinal and ONH vascular autoregulation may be disturbed, inhibiting the modulation of vascular parameters in response to fluctuations in ocular perfusion pressure [40,41,42,43,44]. Therefore, the idea that BP affects ocular perfusion is reasonable. Although mVD derived from OCTA is not a global indicator of retinal blood flow, it logically follows that changes in retinal blood flow may also lead to changes in mVD. Previous studies using OCTA found no significant correlation between BP and ONH VD in glaucoma patients [7, 45]. Shoji et al. [11] found that diastolic BP and mean ocular perfusion pressure were weakly and positively correlated with mVD (β = 0.02, P = 0.019; β = 0.08, P = 0.050), although this was not reproduced in the multivariate analyses. These previous results are similar to those reported here, in which MAP and mVD in all eyes with glaucoma were not correlated. Interestingly, in glaucomatous eyes with DH, there was an inverse correlation between MAP and mVD.
The underlying pathophysiological mechanisms of DH in glaucoma remain poorly understood. Currently, the two leading theories are a mechanical influence and a vascular mechanism [46]. Many previous studies have suggested a structural changes in lamina cribrosa as a cause of DH [47,48,49,50]. The common location of DH and the association between DH and glaucomatous structure damage support this mechanical mechanism. However, explaining DH is limited when there is no spatial correlation. It has long been suggested that microvascular ischaemia and autoregulatory dysfunction drive DH development. This theory proposes that vascular vulnerabilities lead to the damage of small vessels around the ONH, micro-occlusion of small retinal vessels, or shear stress-induced damage to vessel walls [46]. Several possible causative factors, including systemic vascular diseases, platelet dysfunction, primary vascular dysregulation, vasospasm, and dysfunctional autoregulation of optic nerve blood flow, have been suggested [51,52,53,54]. In addition, microinfarction and ischaemic changes may render capillaries more vulnerable to mechanical vessel rupture [55].
The theory that vascular mechanisms underlie DH development is inconclusive, but it is reasonable to assume that these may play an adjunctive role. Therefore, patients with DH might also exhibit reduced VD because hypertension is known to cause microvasculature damage. A reduced number of arterioles and capillaries has been known as microvascular rarefaction. An inverse correlation between capillary densities and BP has been identified in animal studies [56, 57]. In addition, human dermal and muscle tissue showed microvascular rarefaction in patients with primary hypertension [58,59,60,61].
Bosch et al. [62] reported that patients with untreated hypertension exhibited more retinal capillary rarefaction than healthy subjects. One noteworthy finding in the present study was that the absolute BP magnitude was related to mVD rather than simply to a hypertension diagnosis. This indicates that the degree of BP control is more important than a diagnosis of hypertension and that well-controlled hypertension may delay the progression of retinal microvasculature damage in glaucoma group with DH.
One limitation of the present study is the use of a single systemic BP measurement as BP is known to fluctuate over time [56]. Measurements at different times of the day [57] or year [58], in different arms [59], or with different cuff sizes [60] can affect the measured values, thereby introducing variability. In addition, as BP was measured at the hospital for this study, the possibility of white coat hypertension cannot be ignored. BPs of all patient were measured using the same automated BP monitor located in the ophthalmology department so that it could minimize this variability. In addition, to ensure accurate BP readings at OCTA scanning, we evaluated the time between OCTA and BP measurements and it did not exceed the maximum of 4 h. This was possible because routine glaucoma screening or follow-up included BP measurement of every patient. Patients were guided to measure BP after 20 min of inactivity during the waiting time.
Another limitation of the present study was that some glaucoma participants used topical antiglaucoma drugs. There is some evidence that topical antiglaucoma drugs can change blood flow in the ONH [61, 63]. Takusagawa et al. [12] found an association between topical β-blocker use and decreased macular VD in glaucomatous eyes measured using OCTA. We did not have participants discontinue antiglaucoma medication use before study commencement for ethical and medical reasons, excluding cases in which the IOP was well controlled after glaucoma surgery or where short-term follow-up observation was performed. In addition, given that systemic antihypertensive drug use and antihypertensive treatment duration had not been evaluated, any potentially confounding effect of these drugs on mVD could not be totally excluded here. In addition, poor evaluation of maximal untreated IOP might have an impact on the selection bias of subgroup analysis.
In conclusion, the present study demonstrates that age affects mVD, as measured using OCTA, in both healthy and glaucomatous eyes. Furthermore, mVD and functional and structural changes are correlated in glaucomatous eyes. However, in glaucomatous eyes with DH, high systemic BP was associated with reduced mVD. This indicates that retinal vessels may be more susceptible to damage induced by high BP in glaucomatous eyes with DH. The present study, which uses OCTA, highlights novel non-IOP mechanisms for determining the health of glaucomatous eyes with DH.
Summary
What was known before
-
Using optical coherence tomography angiography (OCTA), reduced microvascularity of retinal layer has been revealed in glaucoma patients.
-
Macular vessel density(mVD) can be a important index for glaucomatous change because of its anatomical and pathological meaning.
What this study adds
-
Older age is associated with reduced macular vessel density (mVD) in both healthy and glaucomatous eyes
-
Reduced mVD also correlates with functional deterioration than structure damage in glaucomatous eyes.
-
In glaucomatous eyes with disc haemorrhage, high systemic BP is associated with a reduction in mVD.
References
Manalastas PIC, Zangwill LM, Saunders LJ, Mansouri K, Belghith A, Suh MH, et al. Reproducibility of optical coherence tomography angiography macular and optic nerve head vascular density in glaucoma and healthy eyes. J Glaucoma. 2017;26:851–9.
Chen CL, Bojikian KD, Xin C, Wen JC, Gupta D, Zhang Q, et al. Repeatability and reproducibility of optic nerve head perfusion measurements using optical coherence tomography angiography. J Biomed Opt. 2016;21:65002.
Kashani AH, Chen CL, Gahm JK, Zheng F, Richter GM, Rosenfeld PJ, et al. Optical coherence tomography angiography: a comprehensive review of current methods and clinical applications. Prog Retin Eye Res. 2017;60:66–100.
Jia Y, Morrison JC, Tokayer J, Tan O, Lombardi L, Baumann B, et al. Quantitative OCT angiography of optic nerve head blood flow. Biomed Opt Express. 2012;3:3127–37.
Yarmohammadi A, Zangwill LM, Diniz-Filho A, Suh MH, Manalastas PI, Fatehee N, et al. Optical coherence tomography angiography vessel density in healthy, glaucoma suspect, and glaucoma eyes. Invest Ophthalmol Vis Sci. 2016;57:OCT451–9.
Akagi T, Iida Y, Nakanishi H, Terada N, Morooka S, Yamada H, et al. Microvascular density in glaucomatous eyes with hemifield visual field defects: an optical coherence tomography angiography study. Am J Ophthalmol. 2016;168:237–49.
Liu L, Jia Y, Takusagawa HL, Pechauer AD, Edmunds B, Lombardi L, et al. Optical coherence tomography angiography of the peripapillary retina in glaucoma. JAMA Ophthalmol. 2015;133:1045–52.
Wang X, Jiang C, Ko T, Kong X, Yu X, Min W, et al. Correlation between optic disc perfusion and glaucomatous severity in patients with open-angle glaucoma: an optical coherence tomography angiography study. Graefes Arch Clin Exp Ophthalmol. 2015;253:1557–64.
Chen HS, Liu CH, Wu WC, Tseng HJ, Lee YS. Optical Coherence Tomography Angiography of the Superficial Microvasculature in the Macular and Peripapillary Areas in Glaucomatous and Healthy Eyes. Invest Ophthalmol Vis Sci. 2017;58:3637–45.
Akil H, Chopra V, Al-Sheikh M, Ghasemi Falavarjani K, Huang AS, Sadda SR, et al. Swept-source OCT angiography imaging of the macular capillary network in glaucoma. Br J Ophthalmol. 2017; https://doi.org/10.1136/bjophthalmol-2016-309816.
Shoji T, Zangwill LM, Akagi T, Saunders LJ, Yarmohammadi A, Manalastas PIC, et al. Progressive macula vessel density loss in primary open-angle glaucoma: a longitudinal study. Am J Ophthalmol. 2017;182:107–17.
Takusagawa HL, Liu L, Ma KN, Jia Y, Gao SS, Zhang M, et al. Projection-resolved optical coherence tomography angiography of macular retinal circulation in glaucoma. Ophthalmology. 2017;124:1589–99.
Wu J, Sebastian RT, Chu CJ, McGregor F, Dick AD, Liu L. Reduced macular vessel density and capillary perfusion in glaucoma detected using OCT angiography. Curr Eye Res. 2018; 10.1080/02713683.2018.1563195.
Lommatzsch C, Rothaus K, Koch JM, Heinz C, Grisanti S. OCTA vessel density changes in the macular zone in glaucomatous eyes. Graefes Arch Clin Exp Ophthalmol. 2018;256:1499–508.
Yu DY, Cringle SJ, Balaratnasingam C, Morgan WH, Yu PK, Su EN. Retinal ganglion cells: energetics, compartmentation, axonal transport, cytoskeletons and vulnerability. Prog Retin Eye Res. 2013;36:217–46.
Yu DY, Yu PK, Cringle SJ, Kang MH, Su EN. Functional and morphological characteristics of the retinal and choroidal vasculature. Prog Retin Eye Res. 2014;40:53–93.
Garway-Heath DF, Caprioli J, Fitzke FW, Hitchings RA. Scaling the hill of vision: the physiological relationship between light sensitivity and ganglion cell numbers. Invest Ophthalmol Vis Sci. 2000;41:1774–82.
Curcio CA, Allen KA. Topography of ganglion cells in human retina. J Comp Neurol. 1990;300:5–25.
Nolan JM, Stringham JM, Beatty S, Snodderly DM. Spatial profile of macular pigment and its relationship to foveal architecture. Invest Ophthalmol Vis Sci. 2008;49:2134–42.
Hood DC, Raza AS, de Moraes CG, Liebmann JM, Ritch R. Glaucomatous damage of the macula. Prog Retin Eye Res. 2013;32:1–21.
Lee SY, Bae HW, Seong GJ, Kim CY. Diagnostic ability of swept-source and spectral-domain optical coherence tomography for glaucoma. Yonsei Med J. 2018;59:887–96.
An L, Johnstone M, Wang RK. Optical microangiography provides correlation between microstructure and microvasculature of optic nerve head in human subjects. J Biomed Opt. 2012;17:116018.
Zhang A, Zhang Q, Chen CL, Wang RK. Methods and algorithms for optical coherence tomography-based angiography: a review and comparison. J Biomed Opt. 2015;20:100901.
Shahlaee A, Samara WA, Hsu J, Say EA, Khan MA, Sridhar J, et al. In vivo assessment of macular vascular density in healthy human eyes using optical coherence tomography angiography. Am J Ophthalmol. 2016;165:39–46.
Yu J, Jiang C, Wang X, Zhu L, Gu R, Xu H, et al. Macular perfusion in healthy Chinese: an optical coherence tomography angiogram study. Invest Ophthalmol Vis Sci. 2015;56:3212–7.
Iafe NA, Phasukkijwatana N, Chen X, Sarraf D. Retinal capillary density and foveal avascular zone area are age-dependent: quantitative analysis using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57:5780–7.
Coscas F, Sellam A, Glacet-Bernard A, Jung C, Goudot M, Miere A, et al. Normative data for vascular density in superficial and deep capillary plexuses of healthy adults assessed by optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57:OCT211–23.
Gadde SG, Anegondi N, Bhanushali D, Chidambara L, Yadav NK, Khurana A, et al. Quantification of vessel density in retinal optical coherence tomography angiography images using local fractal dimension. Invest Ophthalmol Vis Sci. 2016;57:246–52.
Yarmohammadi A, Zangwill LM, Diniz-Filho A, Suh MH, Yousefi S, Saunders LJ, et al. Relationship between optical coherence tomography angiography vessel density and severity of visual field loss in glaucoma. Ophthalmology. 2016;123:2498–508.
Hwang JC, Konduru R, Zhang X, Tan O, Francis BA, Varma R, et al. Relationship among visual field, blood flow, and neural structure measurements in glaucoma. Invest Ophthalmol Vis Sci. 2012;53:3020–6.
Richter GM, Madi I, Chu Z, Burkemper B, Chang R, Zaman A, et al. Structural and functional associations of macular microcirculation in the ganglion cell-inner plexiform layer in glaucoma using optical coherence tomography angiography. J Glaucoma. 2018;27:281–90.
Grunwald JE, Sinclair SH, Riva CE. Autoregulation of the retinal circulation in response to decrease of intraocular pressure below normal. Invest Ophthalmol Vis Sci. 1982;23:124–7.
Riva CE, Sinclair SH, Grunwald JE. Autoregulation of retinal circulation in response to decrease of perfusion pressure. Invest Ophthalmol Vis Sci. 1981;21:34–8.
Dumskyj MJ, Eriksen JE, Dore CJ, Kohner EM. Autoregulation in the human retinal circulation: assessment using isometric exercise, laser Doppler velocimetry, and computer-assisted image analysis. Microvasc Res. 1996;51:378–92.
Rassam SM, Patel V, Chen HC, Kohner EM. Regional retinal blood flow and vascular autoregulation. Eye. 1996;10:331–7.
Pournaras CJ, Riva CE. [Studies of the hemodynamics of the optic head nerve using laser Doppler flowmetry]. J Fr Ophtalmol. 2001;24:199–205.
Movaffaghy A, Chamot SR, Petrig BL, Riva CE. Blood flow in the human optic nerve head during isometric exercise. Exp Eye Res. 1998;67:561–8.
Riva CE, Hero M, Titze P, Petrig B. Autoregulation of human optic nerve head blood flow in response to acute changes in ocular perfusion pressure. Graefes Arch Clin Exp Ophthalmol. 1997;235:618–26.
Flammer J, Orgul S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Caprioli J, Zeyen T. A critical discussion of the rates of progression and causes of optic nerve damage in glaucoma: International Glaucoma Think Tank II: July 25-26, 2008, Florence, Italy. J Glaucoma. 2009;18:S1–21.
Wagenfeld L, Weiss S, Klemm M, Richard G, Zeitz O. Vascular dysfunction in ocular blood flow regulation: impact of reactive oxygen species in an experimental setup. Invest Ophthalmol Vis Sci. 2014;55:5531–6.
Chin YC, Perera SA, Tun TA, Teh GH, Cheung CY, Aung T, et al. Structural differences in the optic nerve head of glaucoma patients with and without disc hemorrhages. J Glaucoma. 2016;25:e76–81.
Grieshaber MC, Mozaffarieh M, Flammer J. What is the link between vascular dysregulation and glaucoma?. Surv Ophthalmol. 2007;52 Suppl 2:S144–54.
Fuchsjager-Mayrl G, Wally B, Georgopoulos M, Rainer G, Kircher K, Buehl W, et al. Ocular blood flow and systemic blood pressure in patients with primary open-angle glaucoma and ocular hypertension. Invest Ophthalmol Vis Sci. 2004;45:834–9.
Jia Y, Wei E, Wang X, Zhang X, Morrison JC, Parikh M, et al. Optical coherence tomography angiography of optic disc perfusion in glaucoma. Ophthalmology. 2014;121:1322–32.
Kim KE, Park KH. Optic disc hemorrhage in glaucoma: pathophysiology and prognostic significance. Curr Opin Ophthalmol. 2017;28:105–12.
Takayama K, Hangai M, Kimura Y, Morooka S, Nukada M, Akagi T, et al. Three-dimensional imaging of lamina cribrosa defects in glaucoma using swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54:4798–807.
Lee EJ, Kim TW, Kim M, Girard MJ, Mari JM, Weinreb RN. Recent structural alteration of the peripheral lamina cribrosa near the location of disc hemorrhage in glaucoma. Invest Ophthalmol Vis Sci. 2014;55:2805–15.
Kim YK, Park KH. Lamina cribrosa defects in eyes with glaucomatous disc haemorrhage. Acta Ophthalmol. 2016;94:e468–73.
Sharpe GP, Danthurebandara VM, Vianna JR, Alotaibi N, Hutchison DM, Belliveau AC, et al. Optic disc hemorrhages and laminar disinsertions in glaucoma. Ophthalmology. 2016;123:1949–56.
Patel HY, Buys YM, Trope GE. Nailfold capillaroscopy assessment in patients with glaucoma with a current optic disc hemorrhage. Can J Ophthalmol. 2015;50:155–8.
Shim SH, Kim JM, Woo HY, Shin KU, Koh JW, Park KH. Association between platelet function and disc hemorrhage in patients with normal-tension glaucoma: a prospective cross-sectional study. Am J Ophthalmol. 2015;160:1191–9 e1.
Park HY, Park SH, Oh YS, Park CK. Nail bed hemorrhage: a clinical marker of optic disc hemorrhage in patients with glaucoma. Arch Ophthalmol. 2011;129:1299–304.
Kurvinen L, Harju M, Saari J, Vesti E. Altered temporal peripapillary retinal flow in patients with disc hemorrhages. Graefes Arch Clin Exp Ophthalmol. 2010;248:1771–5.
Kim YD, Han SB, Park KH, Kim SH, Kim SJ, Seong M, et al. Risk factors associated with optic disc haemorrhage in patients with normal tension glaucoma. Eye. 2010;24:567–72.
Grassi G, Bombelli M, Brambilla G, Trevano FQ, Dell’oro R, Mancia G. Total cardiovascular risk, blood pressure variability and adrenergic overdrive in hypertension: evidence, mechanisms and clinical implications. Curr Hypertens Rep. 2012;14:333–8.
Pickering TG, Harshfield GA, Kleinert HD, Blank S, Laragh JH. Blood pressure during normal daily activities, sleep, and exercise. Comparison of values in normal and hypertensive subjects. JAMA. 1982;247:992–6.
Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci G, Lumachi C, et al. Weather-related changes in 24-hour blood pressure profile: effects of age and implications for hypertension management. Hypertension. 2006;47:155–61.
Lane D, Beevers M, Barnes N, Bourne J, John A, Malins S, et al. Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens. 2002;20:1089–95.
Linfors EW, Feussner JR, Blessing CL, Starmer CF, Neelon FA, McKee PA. Spurious hypertension in the obese patient. Effect of sphygmomanometer cuff size on prevalence of hypertension. Arch Intern Med. 1984;144:1482–5.
Pillunat LE, Bohm AG, Koller AU, Schmidt KG, Klemm M, Richard G. Effect of topical dorzolamide on optic nerve head blood flow. Graefes Arch Clin Exp Ophthalmol. 1999;237:495–500.
Bosch AJ, Harazny JM, Kistner I, Friedrich S, Wojtkiewicz J, Schmieder RE. Retinal capillary rarefaction in patients with untreated mild-moderate hypertension. BMC Cardiovasc Disord. 2017;17:300.
Arend O, Harris A, Arend S, Remky A, Martin BJ. The acute effect of topical beta-adrenoreceptor blocking agents on retinal and optic nerve head circulation. Acta Ophthalmol Scand. 1998;76:43–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, C.K., Lee, K., Kim, E.W. et al. Effect of systemic blood pressure on optical coherence tomography angiography in glaucoma patients. Eye 35, 1967–1976 (2021). https://doi.org/10.1038/s41433-020-01199-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01199-x