Abstract
Aim
To determine predictors of rescue treatment among infants treated for retinopathy of prematurity and to evaluate their ocular outcomes at 18–24 months of corrected age.
Methods
This is a single centre retrospective study of infants who received treatment for type 1 ROP, using laser photocoagulation or anti VEGF agents. Multivariable logistic regression was used to generate a prediction model for rescue treatment of ROP. The primary outcome was an abnormal refractive outcome by 24 months of corrected age, among infants primarily treated with laser therapy.
Results
Two hundred and eight infants (including 416 eyes) who received single (n = 151) or rescue (multiple) treatments (n = 57) were included. Ninety three percent of the infants were primarily treated with laser photocoagulation. Lower gestational age, small for gestational age, early packed red blood cell transfusion (within 2 weeks of postnatal age), and presence of Zone 1 retinopathy predicted the need for rescue treatment in treated infants [area under the receiver operating characteristic curve: 0.81 (0.73–0.89)]. The incidence of abnormal refractive outcome, assessed in a total of 174 infants, was found to be significantly higher in the rescue treatment group (67% versus 21%, adjusted odds ratio: 7.56 (3.3–17.2), P < 0.001). Myopia, very high myopia and use of spectacles was significantly higher in the rescue treatment group (P < 0.001 for each).
Conclusions
Rescue treatment for ROP was associated with an increased incidence of refractive errors and requirement of spectacles by 2 years of age. Larger prospective multicentre studies are required to confirm the findings from our study.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) has been identified as a leading cause of preventable blindness in high income countries and as an emerging cause of severe visual impairment in middle income countries [1]. The incidence of severe ROP and treatment requiring ROP is increasing worldwide [2]. Severe ROP has been associated with delayed maturation of white matter and optic radiations as well as reduced brain volumes, with potentially serious implications for neural and visual development [3].
Laser photocoagulation is the first-line therapy for type 1 ROP [4]. Evidence of benefit in Zone 1 disease has led to increasing use of intravitreal anti VEGF (vascular endothelial growth factor) as the primary treatment for ROP [5]. A large proportion of infants are successfully managed with a single treatment, with either laser therapy or anti VEGF agents. However, many infants require rescue therapies as part of ongoing care and staged treatment. The two largest clinical trials conducted to date on ROP treatment strategies have acknowledged the need for rescue treatments in 25–30% of infants with treated ROP [5, 6].
Among extreme preterm birth survivors, treated ROP has been implicated as a major risk factor for abnormal visual outcomes in children [7]. Improved survival of extremely premature neonates and intensified screening and detection of zone 1 retinopathy, have likely further accentuated the morbidity associated with treated ROP [4]. In recent cohorts, nearly 40–50% of infants treated for ROP were reported to experience unfavourable visual outcomes at 18–24 months [8, 9]. Follow-up studies have reported a high incidence of myopia with laser ablation as compared to primary anti-VEGF therapy [10, 11]. However, there is very limited data on the visual and refractive outcomes of infants that receive rescue therapies for ROP.
Clinical prediction models have identified risk factors that could predispose infants to develop severe ROP and require treatment for ROP [12]. However, there is limited understanding regarding factors that could predispose treated infants to require rescue treatment. Assessment of risk factors and visual morbidities in those infants could aid in prognostication while counselling families in the neonatal intensive care unit. Knowledge of modifiable risk factors could also drive quality improvement initiatives to reduce the burden of treated ROP in a variety of neonatal care settings worldwide.
Therefore, we aimed to study the predictors of rescue treatment among infants treated for ROP and measure the refractive outcomes of those infants at 18–24 months corrected age.
Patients and methods
This is a retrospective study of neonates admitted in a single centre over a period of 4.5 years (February 2014–December 2018). The hospital is one of the largest tertiary referral centres for neonates in Western India. The centre is part of the Indian National Neonatal Collaborative (INNC) network and accounts for 35% of the extremely premature infants annually enroled in the database. Data for the study were extracted from the INNC database and from patient medical records. The study was approved for a waiver of informed consent by the institutional ethics committee (Surya Children’s Medicare Private Limited, EC-24/08/2019), given the retrospective and observational nature of the investigation.
Screening procedures
Preterm infants <34 weeks and <1750 g were screened per the National Neonatology Forum guidelines for ROP in Indian infants [13]. Staging of ROP was in accordance with the International Committee for the classification of ROP [14]. Binocular indirect ophthalmoscopy was used for screening. Weekly examinations were continued until complete vascularisation of the retina or until ROP regression was documented in two successive retinal examinations.
All infants diagnosed with Type 1 retinopathy per Early treatment for ROP (ETROP) study guidelines were considered for treatment [15]. Three trained paediatric ophthalmologists (with more than 12 years experience each) were involved in screening and treatment of ROP in our unit. Serial screening of an individual patient was assigned to a single ophthalmologist, and when treatment was deemed indicated, it was initiated only after the ophthalmoscopy findings were secondarily reviewed by a senior ophthalmologist. Any discordance between the lead and the senior ophthalmologist with regard to the ROP staging and treatment decision was discussed with the neonatologists and resolved by a consensus based approach. Infants were treated within 48 h of qualifying for treatment.
Treatment groups
Treated ROP was divided into two categories. The single treatment group comprised infants that were treated once with either laser therapy or anti VEGF. The rescue treatment group was defined to include infants that required any of the following: (a) laser therapy twice or more for progressive neovascularization, (b) laser therapy followed by adjuvant therapy with anti VEGF, (c) anti VEGF followed by laser therapy for recurrence of ROP. “Fill in” laser therapy to treat skipped areas from previous laser sessions, was not considered rescue therapy.
Treatment criteria and procedures
Laser ablation was the primary mode of treatment in the unit. Anti VEGF agent was considered the primary treatment modality in the following situations: (a) aggressive posterior zone ROP (b) stage 3 ROP noted in Zone 1, (c) an undilating pupil or poor visibility due to media opacities precluding laser therapy, (d) infant was too sick for laser therapy. Informed consent for treatment was obtained from the parents of all the patients.
Persistence of or new vessel formation on the iris, or persistence of plus disease and progression of retinal neovascularization despite complete photocoagulation were considered indications for rescue treatment. These infants were subjected to either a second round of laser therapy applied between the previous laser scars, or adjuvant therapy with anti VEGF. Infants primarily treated with anti VEGF were treated with laser if recurrence of retinal neovascularization was noted. Persistence of vascular tortuosity after anti VEGF injection was not considered an indication for additional treatment. Retreatment with anti VEGF was avoided in the first month following primary anti-VEGF therapy.
For laser therapy, an infrared diode laser (810 nm wavelength) via indirect ophthalmoscopy was used to ablate the avascular retina in a near confluent pattern, under topical anaesthesia with 0.5% Proparacaine. For anti-VEGF therapy, intravitreal bevacizumab at a dose of 0.625 mg (Avastin, Roche Products limited, India, 0.625 mg/0.025 ml) was administered under topical anaesthesia, using a 30 gauge needle inserted 1–1.5 mm inferotemporal to the sclerocorneal junction. When bevacizumab was unavailable, intravitreal ranibizumab at a dose of 0.2 mg (Lucentis, Novartis India Ltd, 0.2 mg/0.02 ml) was used as the anti VEGF agent.
Outcome assessment
The main outcomes of interest were (a) predictors of rescue treatment in treated ROP (b) refractive outcomes at 18–24 months among infants that received rescue treatments for ROP. Considering the higher incidence of myopia among infants treated with laser photocoagulation as compared to anti-VEGF monotherapy [10, 16], we restricted the analysis of refraction to infants that were primarily treated with laser therapy in both groups. Baseline maternal and neonatal demographic characteristics were recorded in a pre-designed case record form. We also collected data on risk factors for severe ROP, including mechanical ventilation, sepsis, early postnatal weight gain (weight gain in the first four postnatal weeks), and packed red blood cell (RBC) transfusions.
Infants who required treatment for ROP were followed up every 3–6 months in the first 2 years of age. Abnormal refractive outcome at 18–24 months was a composite outcome defined by the presence of myopia (≥0.25 dioptres) [17], hyperopia (≥4.00 dioptres) or astigmatism (>2.00 dioptres) [18]. The other outcomes assessed were need for spectacles, very high myopia (≥5.00D), strabismus, cortical visual impairment, and blindness (visual acuity of 20/200) in at least one eye. Refractive status of the infant was assessed using wet retinoscopy after instillation of 1% cyclopentolate hydrochloride, 0.8% tropicamide and 5% phenylephrine drops. Refractive correction was prescribed according to the recommendations by the American Academy of ophthalmology for preferred practice patterns in paediatric eye evaluations [19].
Statistical analysis
Descriptive statistics were computed for variables in both groups and presented as means and standard deviations (for parametric continuous data), medians and inter-quartile ranges (for non-parametric continuous data) and proportions (for categorical data). Baseline characteristics and outcome measures between the single and rescue treatment groups were compared using the Chi square test, two sample t-test or Mann–Whitney U test as applicable. Logistic regression analysis was used to generate the prediction model for rescue treatment. Clinically important covariates that were statistically different between the two groups (P value of <0.2) on univariate analysis were included in a multivariate logistic regression model. The final model was constructed using a stepwise backward elimination method to exclude variables that were not significant in predicting the need for rescue treatments. Covariates were examined for multicollinearity (variance inflation factor >2.5) prior to inclusion in the model. Bootstrap resampling method was used to internally validate our model and the corrected area under the receiver operating characteristic (ROC) was estimated to determine the discriminatory power of the model. The goodness of fit of the final model was tested by comparing the area under the ROC with that of the primary multivariate model. For the primary outcome, the adjusted odds ratios with 95% confidence intervals were reported, controlling for gestational age and the presence of zone 1 ROP a priori. All P values were two sided and a P value of <0.05 was considered statistically significant. Stata - version 13.1 (Statacorp, 4905 Lakeway Drive College Station, Texas, USA) was used for statistical analysis.
Results
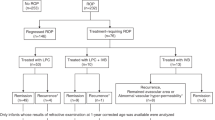
A total of 208 infants required treatment for ROP during the 4.5 year time period. Single treatment was administered in 151 patients while 57 infants received multiple treatments. The details of patient enrolment for the study have been displayed in Fig. 1.
Laser ablation was the primary treatment modality in 193 patients. Ten infants required “fill in” lasers within a period of 3 weeks of the primary laser session. Thirteen infants required rescue laser therapy following the primary laser treatment for progressive neovascularisation. Median time to rescue laser therapy was 5.5 weeks in this group.
Fifteen infants (seven in the single treatment group and eight in the rescue treatment group) were primarily treated with anti VEGF agents. Bevacizumab was the anti VEGF agent used in all of these instances except one who received intravitreal ranibizumab. One infant needed treatment with two courses of bevacizumab.
All patients in our study had bilateral eye disease requiring treatment in both eyes; 90% (n = 188) of infants were treated for type 1 ROP.
Among the cohort, 62% of the neonates were outborn and 71% were delivered by caesarean section. At least one dose of antenatal steroids was received by 84% of mothers (Table 1). Infants in the rescue treatment group were of lower birth weight and had higher rates of mechanical ventilation, infection, and RBC transfusions as compared to the single treatment group. The presence of Zone 1 ROP and use of anti VEGF was significantly higher in the rescue treatment group (Table 1). We included the following variables in the primary regression model—gestational age, being small for gestational age (SGA), male gender, outborn status, SNAPPE score, postnatal weight gain, patent ductus arteriosus, late onset sepsis, receipt of postnatal steroids, need for early packed RBC transfusion, presence of Zone 1 ROP, and days on mechanical ventilation. Following sequential elimination of covariates (significance level of P > 0.2), lower gestational age, SGA, need for RBC transfusion within the first 2 weeks of life, and the presence of Zone 1 ROP were identified as predictors for rescue treatment of ROP. The odds ratios and the 95% confidence intervals of the predictors are shown in Table 2. The area under the ROC curve for our final model was 0.81 (95% CI: 0.73–0.89) (Fig. 2). The apparent performance of our model was tested in 200 bootstrap samples that were randomly drawn with replacement from our original sample. The optimism corrected area under the ROC was calculated to be 0.804 (95% CI: 0.734–0.895) suggesting high discriminatory power of our model in predicting the need for rescue treatment. Test for equality of the ROC areas between the nested models suggested good model fit (0.81 versus 0.83, P = 0.35).
Out of the 208 infants included in the study, data on refractive outcomes at 18–24 months of corrected age were available for 189 infants. The refractive outcomes of 174 infants primarily treated with laser photocoagulation (129 in the single treatment group versus 45 in the rescue treatment group) were compared. Refractive abnormalities were significantly higher in the rescue treatment group [67% versus 21%, adjusted OR: 7.56 (95% CI: 3.3–17.2), P < 0.001]. The incidence of myopia, very high myopia and the need for spectacles was also significantly higher in the rescue treatment group (Table 3).
Two infants developed retinal detachment in the right eye despite rescue treatments and underwent lens sparing vitrectomy at 3 months of corrected age. The first infant was born at a gestational age of 26 weeks and developed aggressive posterior ROP at 34 weeks postmenstrual age, requiring treatment with intravitreal anti VEGF. Four weeks later, the infant received secondary treatment with laser for plus disease; however developed fibroretinal traction on follow up leading to partial retinal detachment. The second infant was born at 24 weeks and 5 days of gestation and developed stage 3 plus disease in zone II requiring laser photocoagulation at 33 weeks postmenstual age. At term gestational age, the infant was treated with anti VEGF agents for neovascularisation in the macular area, but progressed to develop extensive fibrotic changes in the retina and macular traction. Both the infants subsequently developed retinal detachment in left eye at 5 months of corrected age and underwent vitrectomy. On follow up, both the infants had bilateral blindness with no functional vision. Two infants in the single treatment group required surgical correction of strabismus at 21 and 24 months of corrected age.
Discussion
Our study demonstrates that lower gestational age, SGA, need for early packed RBC transfusion (within the first 2 weeks of life) and the presence of Zone 1 ROP predict the need for rescue treatment among preterm infants with treated ROP. We also found that infants who received rescue therapy had increased odds of an abnormal refractive outcome and an increased requirement for spectacles at 2 years of age.
Progression and reactivation of ROP despite primary treatment is increasingly being recognised in high risk neonatal populations, expanding the premise for rescue therapies [20, 21]. The incidence of rescue treatment in our study is in line with contemporary evidence from prospective studies. While the BEAT ROP investigators reported that 22% of infants with Zone 1 ROP required rescue therapy following primary laser photocoagulation [5], another RCT reported 26% recurrence rate of Zone 2 ROP following single dose anti VEGF treatment [22]. A recent multinational clinical trial comparing the efficacy of two doses of ranibizumab against laser therapy for ROP in zone 1 and 2 also reported 25–30% retreatment rate in all the treatment arms [6].
Our prediction model is concordant with prior evidence describing risk factors of severe and progressive retinopathy in neonates. Extreme prematurity and aggressive posterior ROP have been shown to be important risk factors for rescue treatment in other studies [23]. A recent meta-analysis of observational studies involving 190,146 infants showed a higher risk of ROP treatment in preterm SGA infants when compared to preterm non SGA infants [24]. Lust et al. showed that infants receiving packed RBC transfusions within the first 10 days following birth had four times higher odds of developing severe ROP independent of gestational age and oxygen requirements [25].
Various observational studies have reported on the visual and refractive outcomes of infants treated for ROP. While the Canadian Neonatal network and the NICHD report excluded infants that required multiple treatments [8, 9], a retrospective observational study of 61 infants (n = 45 for single treatment, n = 16 for rescue treatment) reported the visual outcomes to be similar in the groups despite a five times higher odds of severe psychomotor disabilities in the rescue treatment group [26]. Another retrospective study of 34 infants suggested a higher prevalence of myopia (82% versus 42%) and high myopia (29% versus 10%) at 2 years of age, with rescue treatment in 9 patients as compared to anti-VEGF monotherapy in 20 patients [27].
Our study infants differed from the aforementioned cohorts in various characteristics. First, the infants in our study were of slightly higher birth weight and a large proportion of them were outborn. Secondly, only 7% of study infants received anti VEGF as the primary treatment modality. This likely reflects the influence on local practice of growing concerns over the potential long term neurological and cognitive deficits associated with off label use of anti VEGF agents in vulnerable patient populations.
We found a significant increase in refractive abnormalities at 18–24 months following rescue treatment. It is possible that this association could be confounded by the predictors that we demonstrate in our model, particularly prematurity [28] and zone 1 disease. In a large national cohort of extremely preterm children, lower gestational age was predictive of refractive abnormalities, even after adjustment for treatment requiring ROP [7]. Zone 1 ROP was shown to be associated with high myopic refractive errors in eyes treated with either laser or anti VEGF [29]. Hence, we sought to adjust for the effect of these two confounders on the refractive outcomes in our study infants.
Although the sample size was dictated by the availability of data, our study had 90% power to detect a twofold change in the primary outcome with the available sample size and a 2:5 allocation ratio among groups. While this was a single centre study, the shared decision making approach employed locally ensured that choice of treatment was less likely to be influenced by clinician preferences. Variability in ROP stage ascertainment was also reduced. The follow up rate of over 95% is another strength of our study.
Our study has several limitations. We acknowledge that the retrospective study design could have introduced unmeasured biases. The generalisability of our study is limited by the single centre model. The treatment indications in our patients could slightly differ from cohorts in other geographic regions. Rapidly evolving treatment concepts and regional variations in management of ROP [30] could also have contributed to this difference. It is possible that the case- mix of infants requiring primary laser or anti VEGF treatment in each study group could have slightly influenced the risk of a subsequent treatment in the rescue treatment group. A small minority of our patients (9%) were treated for a disease milder than that recommended by ETROP guidelines, based on local ophthalmologist consensus. Nine infants with persistence of active ROP in Zone 2 or 3 beyond a postmenstrual age of 44 weeks (smouldering ROP) and 11 infants with Zone 2 posterior ROP without plus disease received treatment. However, such treatment patterns based on clinical judgement are reported to be similarly prevalent in recent study cohorts [31]. While refraction was routinely assessed at 18–24 months, visual acuity was not assessed in the majority of these patients. The dynamics of refraction are known to be variable until 2.5 years of age [32], yet, it remains highly likely that our observations at 18–24 months bear a significant relationship to future refractory outcome.
In summary, our study highlights the burden of refractive abnormalities in infants exposed to rescue treatments for ROP. There is a need for additional prospective studies of long term visual outcomes of rescue treatment in large and diverse neonatal cohorts.
Summary
What was known before
-
Laser photocoagulation and anti VEGF agents are the two most common modalities of primary treatment for ROP.
-
Recent multicentre studies have reported infants to have received additional rounds of treatment, despite being primarily treated for ROP.
What this study adds
-
Extreme prematurity, early packed RBC transfusion and zone 1 retinopathy predicted the need for additional rescue treatment in preterm infants with treated ROP.
-
Receipt of rescue treatment was associated with an increased incidence of abnormal refractive outcomes and the need for spectacles at 2 years of corrected age.
References
Gilbert C, Foster A. Childhood blindness in the context of VISION 2020-the right to sight. Bull World Health Organ. 2001;79:227–32.
Darlow BA, Gilbert C. Retinopathy of prematurity - a world update. Semin Perinatol. 2019;43:315–6.
Glass TJA, Chau V, Gardiner J, Foong J, Vinall J, Zwicker JG, et al. Severe retinopathy of prematurity predicts delayed white matter maturation and poorer neurodevelopment. Arch Dis Child Fetal Neonatal Ed. 2017;102:F532–7.
Adams GG, Bunce C, Xing W, Butler L, Long V, Reddy A, et al. Treatment trends for retinopathy of prematurity in the UK: active surveillance study of infants at risk. BMJ Open. 2017. https://doi.org/10.1136/bmjopen-2016-013366. e-pub ahead of print 21 March 2017.
Mintz-Hittner HA, Kennedy KA, Chuang AZ. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603–15.
Stahl A, Lepore D, Fielder A, Fleck B, Reynolds JD, Chiang MF, et al. Ranibizumab versus laser therapy for the treatment of very low birthweight infants with retinopathy of prematurity (RAINBOW): an open-label randomised controlled trial. Lancet. 2019;394:1551–9.
Hellgren KM, Tornqvist K, Jakobsson PG, Lundgren P, Carlsson B, Kallen K, et al. Ophthalmologic outcome of extremely preterm infants at 6.5 years of age: extremely preterm infants in Sweden Study (EXPRESS). JAMA Ophthalmol. 2016;134:555–62.
Morin J, Luu TM, Superstein R, Ospina LH, Lefebvre F, Simard MN, et al. Neurodevelopmental outcomes following bevacizumab injections for retinopathy of prematurity. Pediatrics. 2016. https://doi.org/10.1542/peds.2015-3218.
Natarajan G, Shankaran S, Nolen TL, Sridhar A, Kennedy KA, Hintz SR, et al. Neurodevelopmental outcomes of preterm infants with retinopathy of prematurity by treatment. Pediatrics. 2019. https://doi.org/10.1542/peds.2018-3537.
Geloneck MM, Chuang AZ, Clark WL, Hunt MG, Norman AA, Packwood EA, et al. Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. JAMA Ophthalmol. 2014;132:1327–33.
Abri Aghdam K, Khadamy J, Falavarjani KG, Tsui I. Refractive outcomes following the treatment of retinopathy of prematurity in the anti-VEGF era: a literature review. J AAPOS. 2016;20:539–40.e3.
Husain SM, Sinha AK, Bunce C, Arora P, Lopez W, Mun KS, et al. Relationships between maternal ethnicity, gestational age, birth weight, weight gain, and severe retinopathy of prematurity. J Pediatr. 2013;163:67–72.
Honavar SG. Do we need India-specific retinopathy of prematurity screening guidelines? Indian J Ophthalmol. 2019;67:711–6.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–94.
Sankar MJ, Sankar J, Chandra P. Anti-vascular endothelial growth factor (VEGF) drugs for treatment of retinopathy of prematurity. Cochrane Database Syst Rev. 2018;1:CD009734 https://doi.org/10.1002/14651858.CD009734.pub3.
Quinn GE, Dobson V, Davitt BV, Hardy RJ, Tung B, Pedroza C, et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: findings to 3 years of age. Ophthalmology. 2008;115:1058–64.e1.
Davitt BV, Dobson V, Quinn GE, Hardy RJ, Tung B, Good WV. Astigmatism in the Early Treatment for Retinopathy Of Prematurity Study: findings to 3 years of age. Ophthalmology. 2009;116:332–9.
Miller JM, Harvey EM. Spectacle prescribing recommendations of AAPOS members. J Pediatr Ophthalmol Strabismus. 1998;35:51–2.
Bourla DH, Gonzales CR, Valijan S, Yu F, Mango CW, Schwartz SD. Association of systemic risk factors with the progression of laser-treated retinopathy of prematurity to retinal detachment. Retina. 2008;28:S58–64.
Chen TA, Shields RA, Bodnar ZH, Callaway NF, Schachar IH, Moshfeghi DM. A spectrum of regression following intravitreal bevacizumab in retinopathy of prematurity. Am J Ophthalmol. 2019;198:63–9.
Zhang G, Yang M, Zeng J, Vakros G, Su K, Chen M, et al. Comparison of intravitreal injection of ranibizumab versus laser therapy for zone ii treatment-requiring retinopathy of prematurity. Retina. 2017;37:710–7.
Vinekar A, Trese MT, Capone A Jr. Evolution of retinal detachment in posterior retinopathy of prematurity: impact on treatment approach. Am J Ophthalmol. 2008;145:548–55.
Razak A, Faden M. Association of small for gestational age with retinopathy of prematurity: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2020;105:270–8.
Lust C, Vesoulis Z, Jackups R Jr., Liao S, Rao R, Mathur AM. Early red cell transfusion is associated with development of severe retinopathy of prematurity. J Perinatol. 2019;39:393–400.
Lien R, Yu MH, Hsu KH, Liao PJ, Chen YP, Lai CC, et al. Neurodevelopmental Outcomes in Infants with Retinopathy of Prematurity and Bevacizumab Treatment. PLoS ONE. 2016. https://doi.org/10.1371/journal.pone.0148019.
Chen YH, Chen SN, Lien RI, Shih CP, Chao AN, Chen KJ, et al. Refractive errors after the use of bevacizumab for the treatment of retinopathy of prematurity: 2-year outcomes. Eye (Lond). 2014;28:1080–6. quiz 1087.
Fielder AR, Quinn GE. Myopia of prematurity: nature, nurture, or disease? Br J Ophthalmol. 1997;81:2–3.
Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR. Outcomes after Intravitreal Bevacizumab versus Laser Photocoagulation for Retinopathy of Prematurity: a 5-Year Retrospective Analysis. Ophthalmology. 2015;122:1008–15.
Darlow BA, Lui K, Kusuda S, Reichman B, Hakansson S, Bassler D, et al. International variations and trends in the treatment for retinopathy of prematurity. Br J Ophthalmol. 2017;101:1399–404.
Gupta MP, Chan RVP, Anzures R, Ostmo S, Jonas K, Chiang MF. Practice patterns in retinopathy of prematurity treatment for disease milder than recommended by guidelines. Am J Ophthalmol. 2016;163:1–10.
Holmstrom G, Larsson E. Long-term follow-up of visual functions in prematurely born children-a prospective population-based study up to 10 years of age. J AAPOS. 2008;12:157–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balasubramanian, H., Sindhur, M., Doshi, A. et al. Predictors and ocular outcomes of rescue treatment in preterm infants with treated retinopathy of prematurity—a retrospective study. Eye 35, 1937–1945 (2021). https://doi.org/10.1038/s41433-020-01186-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01186-2