Abstract
Purpose
To assess the reliability and the diagnostic performance of a novel CE (European Conformity)-marked and FDA (Food and Drug Administration)-cleared dot patient self-monitoring test (Alleye, Oculocare medical Inc.) for the detection and characterization of metamorphopsia in age-related macular degeneration (AMD).
Methods
Three consecutive tests were performed in 63 wet AMD, 26 dry AMD, and 19 age-matched healthy eyes. In addition, the test was performed in 34 young healthy eyes. The mean Alleye score and standard deviations (SDs) were calculated for each eye and group. We compared and tested healthy with dry and wet AMD eyes and assessed the extent to which the test discriminated between healthy subjects and patients with dry and wet AMD using the area under the receiver operating characteristic curve (AUC).
Results
The mean (SD) Alleye score was 49.5 (16.1) in wet AMD eyes, 62.1 (22.5) in dry AMD eyes, 69.8 (10.2) in age-matched healthy eyes, and 85.3 (10.0) in young healthy subjects. Compared to age-matched healthy subjects, the AUC (95% confidence interval) to detect wet AMD was 0.845 (0.759–0.932), and 0.660 (0.520–0.799) to discriminate between dry and wet AMD. Compared to young healthy subjects, the AUC to detect dry AMD was 0.799 (0.675–0.923), and 0.969 (0.940–0.997) to detect wet AMD.
Conclusions
This is the first assessment of Alleye in clinical practice. The test is highly accurate to detect wet AMD and reasonably accurate to classify dry vs. wet AMD. Data from longitudinal monitoring and its role in the therapeutic management of AMD is warranted.
Similar content being viewed by others
Background
For accurate prognosis of visual outcome, self-monitoring of macular function has been shown to be indispensable in patients suffering from wet age-related macular degeneration (AMD) treated according to established anti-vascular endothelial growth factor (VEGF) regimens [1, 2]. The Amsler grid test, which was described more than 70 years ago [3], is the most frequently recommended self-monitoring tests for the qualitative assessment of macular function [2]. Macular function as measured by the Amsler grid test assesses hyperacuity, the ability of the human eye to detect even faint alterations in the shape of straight lines [4]. The decrease of hyperacuity is a proxy for a common symptom of retinal disease—the so-called metamorphopsia—a metamorphosis of sight caused by damage of the retina [5].
With the transformation of wet AMD patient management by the introduction of anti-VEGF agents, the requirements for a screening and self-monitoring test have changed. In order to be effective in the hand of patients, a test needs to be intuitive and able to reliably detect even slight fluctuations in macular function. However, a recent systematic review assessing the diagnostic accuracy of the Amsler grid and other hyperacuity tests revealed only limited diagnostic performance [6]. Various reasons for the limited performance of the Amsler grid test exist, but one possible explanation may be that the assessment of metamorphopsia by hyperacuity is a psychophysical measurement involving extra-foveolar retinal regions, asking patients to evaluate visual phenomena without fixating them. Using an Amsler grid patients often move their gaze from the central fixation dot to the area where they see metamorphopsia. This decreases the reproducibility and the ability to quantify this symptom or detect changes in metamorphopsia in eyes with pre-existing pathologies [7, 8]
Modern anti-VEGF treatment protocols for macular diseases such as a treat-and-extend regimen would ideally be supplemented by a self-monitoring tool as intuitive as the Amsler grid test, but with the ability to quantify even subtle changes of hyperacuity in corresponding retinal regions. In recent years, the preferential hyperacuity perimetry (PHP, Notal Vision Inc.) has gained popularity in patient self-testing for AMD. A clinical study showed a smaller decline in visual acuity compared to standard care when using the PHP test [9]. The test runs on a stand-alone device that connects via a wireless service to the company’s data monitoring center. Besides the need for additional hardware, a possible disadvantage to PHP is its high price [10]. In this paper, we describe a novel, intuitive, and freely available mobile app for self-monitoring (dot alignment test, Alleye) of metamorphopsia that can be performed everywhere and anytime by patients using their own smartphones or tablets. Alleye is a CE (European Conformity)-marked Class I medical device that received FDA (Food and Drug Administration) 510(k) clearance for monitoring eyesight in AMD in 2018.
Methods
The research presented in this paper adhered to the tenets of the Declaration of Helsinki and informed consent was obtained from the subjects after explanation of the nature and possible consequences of the study. The protocol was approved by the institutional review board of the Cantonal Hospital Lucerne, Switzerland.
The Alleye app
The Alleye is a mobile medical software application indicated for the detection and characterization of metamorphopsia, a visual distortion, in patients with AMD and as an aid in the monitoring of the progression of this condition with respect to metamorphopsia. It is intended to be used by patients who have the capability to regularly perform a simple self-test at home. Alleye consists of two different items: a mobile app for patients and a web interface for eye care professionals. Alleye implements an alignment hyperacuity task that helps patients with AMD to assess their visual function at home. This allows the timely detection of significant changes in vision function, enabling the regular monitoring of the disease progression and/or monitoring of visual function during ongoing treatments. The Alleye algorithm was developed using the performance found in healthy subjects completing the task. Using these values we defined the normal range. Subjects performing the Alleye task are compared against those norm values.
The self-monitoring task
Alleye’s monocular task is to align a mobile central dot along the two fixed flanking dots to an imaginary straight line. This task is repeated three times in differing positions with different distances between central and flanking dots in horizontal, vertical, and oblique axes (see: www.alleye.io). Essentially, this self-monitoring task applies a similar principle of hyperacuity testing as the well-known Amsler grid test. Different from the Amsler grid, this test assures that patients fixate on the mobile central dot while keeping the outer dots in their paracentral visual field by asking to move the central dot along an imaginary straight line between two flanking dots. By directing and hence fixating the mobile central dot, the task avoids saccades to the outer, flanking dots while moving the central dot (see Fig. 1). While in each of the 12 tasks the patient’s attention and his fovea or his best fixating extrafoveal spot remains on the mobile dot, the test examines the two areas of the macula where the flanking dots are seen. In Fig. 2 we show the representation of the tested dots on the central and paracentral macula in relation to the Amsler grid [3]. In an emmetropic eye, this test covers 12.7° field of view, while the Amsler grid covers 20°, assuming a test distance of about 30cm. Technical specifications are available from the company’s website (https://alleye.io/#/product-alleye). The test is performed monocularly after covering the non-tested eye.
A representative screen shot of the Alleye dot alignment test. The patient’s task is to align the movable target dot in between the two fixed outer dots to finally form a straight line. The deviation between the final position of the target dot and the ideal straight line is used to calculate the test score
Different examples of individual tasks testing central and paracentral areas of the macula. The full test consists out of 12 individual tasks with the fixation dot set to test all four major axes with three repeats per axis using different offset from the center dots for the target dot to test central and paracentral areas of the macula
Patients with AMD
Patients attending the AMD ward were informed by means of posters in the waiting room, and by the treating physician who checked the inclusion criteria. In positive cases, patients were provided with detailed oral and written information about the study and were asked whether they were willing to participate. Participating patients provided written informed consent. Patients with dry AMD and patients with active choroidal neovascularization (CNV) secondary to AMD, either newly diagnosed (treatment-naive) or under current treatment with anti-VEGF agents, were included in the study and underwent a complete ophthalmologic examination. If both eyes were affected by AMD, both were included in the study. Patients with a neurological or physical illness that impeded them from using a mobile device to adequately perform the Alleye test were excluded.
Healthy eyes
We sampled two groups of subjects providing data on healthy eyes: an age-matched group of patients attending the AMD clinic who had a monocular condition and an unaffected eye and a group of young healthy subjects. These young healthy subjects were recruited from the hospital staff, researchers, and their family members. Participating healthy subjects received a detailed oral information about the study and provided written informed consent. The tested eye was randomly selected using a computer-generated randomization list.
Examination setting
Relevant clinical characteristics of all participants were recorded. Following ophthalmological examination, an initial Alleye task to test for the ability to use the app on a mobile device was conducted. After receiving brief instruction on self-administration of the test, participants performed subsequent self-measurements on their own. Each participant received an instruction manual, and the research fellows provided technical assistance during the examination if needed. Participants performed the test with their glasses, and were instructed how to cover one eye as this is a monocular test. The test had to be performed according to the label. In total, all participants performed four measurements: one training test followed by three valid consecutive measurements. If something unexpected happened during the test, the result was discarded and the test was repeated. We recorded the time spent to perform the test.
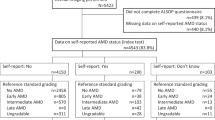
Test–re-test data and test accuracy
Three consecutive tests were performed in 63 wet AMD, 26 dry AMD, and 19 age-matched healthy eyes. In addition, the test was performed in 34 young healthy eyes.
The average Alleye score was calculated for each eye and group. We compared and tested healthy with dry and wet AMD eyes and assessed the extent to which the test discriminated between healthy subjects and patients with dry and wet AMD using the area under the receiver operating characteristic curve (AUC). In total, we fitted six logistic regression models for the following contrasts: age-matched healthy eyes vs. dry AMD and vs. wet AMD, dry AMD vs. wet AMD, and young healthy eyes vs. age-matched healthy eyes, vs. dry AMD and vs. wet AMD. Analyses were performed using the Stata 14.2 statistics software package (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX, USA: StataCorp LP.)
Results
Description of patients with wet and dry AMD
The mean age of patients with wet AMD was 74 years (standard deviation (SD) 10.3; range: 63–88 years), mean total number of intravitreal injections (IVIs) prior to inclusion was 15.7 (SD 11.6; range: 0–49 IVIs), and the mean best-corrected visual acuity (BCVA) at study entry was 71.9 letters (SD 13.8, range 31–93 letters) on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart.
The mean age of patient with dry AMD was 81 years (SD 6.2; range 70–93 years) and the mean BCVA at study entry was 77.2 letters (SD 13.1; range 32–93 letters).
Description of healthy groups
The mean age of age-matched subjects without a retinal condition was 67 years (SD 10.1; range 49–86) and the BCVA was 86.2 letters (SD 7.1; range 73–98). The mean age of 34 healthy eyes was 38 years (SD 15.0; range 17–56 years). Ten subjects (38.5%) performed the test with spectacles. One 31-year-old female had undergone refractive surgery 2 years prior to testing. The median BCVA was 102 letters on the ETDRS acuity chart (range 100–110 letters).
Alleye scores within groups
The mean Alleye score (SD) in wet AMD eyes was 49.5 (16.1). In dry AMD the scores were higher 62.1 (22.5); p = 0.004. The mean score found in age-matched healthy eyes was 69.8 (10.2). The highest mean Alleye scores were found among young healthy subjects (85.3 (10.0); p < 0.001 compared to age-matched healthy group). The difference in scores between the two healthy groups may be explained by the large age difference and the slightly higher BCVA found in the young healthy group.
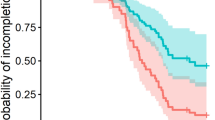
Diagnostic performance
Table 1 summarizes the AUCs found for six different contrasts. Not surprisingly, the highest AUC (95% confidence interval) was found for the comparison of young healthy subjects and wet AMD (0.969 (0.940–0.997)) as this comparison reflected the most extreme sampling. More clinically relevant is the comparison between age-matched healthy and wet AMD. The corresponding AUC was 0.845 (0.759–0.932). This indicates that the test works in a screening context. The discrimination between dry and wet AMD was moderate (AUC 0.660 (0.520–0.799)). Again, in more extreme sampling, when discriminating between young healthy subjects and dry AMD, the corresponding AUC was 0.799 (0.675–0.923). Figure 3 summarizes the receiver operating characteristic curves of the different contrasts.
Discussion
Similar to the Amsler grid test, this mobile self-monitoring test of macular function is an intuitive task that needs very little explanation for first time users [11]. As it is a test for hyperacuity, it is hardly affected by visual acuity, but strongly by even subtle structural irregularities of the macula [4, 12]. In contrast to the Amsler grid test, it provides quantitative results and allows patients to self-test the function of their central and paracentral macular areas up to 6.4° from the fovea. In these test–retest experiments, the Alleye scores were reliable making it suitable for self-testing, especially for patients with AMD that experience subtle changes in metamorphopsia caused by fluctuations in macular function.
Recently, the advantages and disadvantages of several technologies used in the detection of AMD have been assessed [6, 13]. Besides optical coherence tomography, Schwartz and Loewenstein assessed the Amsler grid test, near vision acuity, PHP, shape-discrimination hyperacuity with the myVisiontrack®, macular mapping test, and the Noisefield perimeter [10]. They concluded that despite the availability of several promising technologies for the detection of CNV, the tools require further development before they allow the retina specialist to improve wet AMD management.
In our study, the scores obtained in healthy subjects could drop to surprisingly low values. The reason for this remains incompletely understood. We speculate that these participants were slightly less motivated to complete the task or became tired from repeated measurements.
In a previous analysis, decrease of 13 score points indicated a worsening, and a drop of 25 score points indicated a significant worsening of metamorphopsia [14]. The clinical interpretation of this finding is not completely straightforward. As all psychophysical tests, results do not translate directly to anatomical features. We assume that the drop in test performance is due to photoreceptor misalignment and therefore a linear dimension rather than a proportional dimension as expected from Weber’s law, since hyperacuity is based on higher visual functions that are not affected by retinal disorders. While the misalignment of photoreceptors does affect the perceived position of an object, it does not necessarily affect the precision of hyperacuity. The visual system detects the position of an object still with high precision, but due to misalignment of the photoreceptors in a wrong position. Thus, misalignment of photoreceptors does not affect acuity and hyperacuity in the same way.
To our knowledge, myVisiontrack® and Alleye are the only two FDA approved medical software applications running on mobile devices. myVisiontrack® uses a shape discrimination task [15,16,17]. Respondents need to identify changes in the shapes of circles. They showed that the app was capable to detect advanced stages of AMD accurately. The test is currently available on prescription in the USA. This new self-monitoring dot alignment test (Alleye® Oculocare medical Inc.) has several characteristics in common; however, compared to myVisiontrack®, which is intended for the detection and characterization of the central three degrees of metamorphopsia, this task covers 12.7°, allowing to screen almost the complete macular area [14]. In our understanding this is an important asset of Alleye, as macular disease often extends within the vascular arcades. Therefore, testing of these areas is required to assess macular function. The test pattern oversamples the central retina by its star like configuration. As normal acuity, hyperacuity decreases with eccentricity. This is compensated as the test compares the deviation in relation to the performance of normal subjects at a given location. In a recent systematic review, the pooled sensitivity of studies assessing the Amsler grid was 0.78 (95% confidence intervals: 0.64–0.87), and the pooled specificity was 0.97 (95% confidence intervals: 0.91–0.99). The pooled sensitivity of studies assessing the PHP was 0.85 (95% confidence intervals: 0.80–0.89), and specificity was 0.87 (95% confidence intervals: 0.82–0.91). Our results for the detection of wet AMD were well in line with those found in the systematic review [6]. For monitoring, longitudinal data need to be collected over a longer period of time. The cross-sectional contrast between Alleye scores obtained from patients with dry vs. wet AMD was only moderate. To further understand the relationship between changes of the Alleye score and the transition of dry to wet AMD, further studies are needed. Possibly the Alleye algorithm needs adaptations to attain a higher performance.
Implications for further research
Further evaluations by people with no affiliation to Alleye should be performed. In view of the encouraging results obtained here, further studies should be designed to quantify the clinical efficacy when using Alleye in the management of patients with AMD with and without CNV. In addition, the value of the test in a (mass-) screening setting and as a monitoring tool needs to be investigated, particularly the optimization of treatment outcomes in a treat-and-extend treatment regimen. Benefits in terms of patient-relevant outcomes when comparing standard of care with management using Alleye monitoring need to be assessed in a randomized clinical trial or in health service research settings.
In conclusion, the new dot alignment test is a reliable, intuitive, and freely available self-monitoring tool allowing patients to screen and monitor their macular function regularly at home using their own smart phone or tablets. Further studies are currently in progress to determine which patient groups (i.e., age, diagnosis, vision) will profit most from this improved hyperacuity test.
Summary
What was known before
For accurate prognosis of visual outcome, self-monitoring of macular function has been shown to be indispensable in patients suffering from wet AMD treated according to established anti-VEGF regimens. A novel CE-marked and FDA-cleared dot patient self-monitoring test for the detection and characterization of metamorphopsia in AMD has been developed.
What this study adds
The test is highly accurate to detect wet AMD and reasonably accurate to classify dry vs. wet AMD. Similar to the Amsler grid test, this mobile self-monitoring test of macular function is an intuitive task that needs very little explanation for first time users.
References
Chew EY, Clemons TE, Bressler SB, Elman MJ, Danis RP, Domalpally A, et al. Randomized trial of a Home Monitoring System for Early Detection of Choroidal Neovascularization Home Monitoring of the Eye (HOME) study. Ophthalmology. 2014;121:535–44.
Schmidt-Erfurth U, Chong V, Loewenstein A, Larsen M, Souied E, Schlingemann R, et al. Guidelines for the management of neovascular age-related macular degeneration by the European Society of Retina Specialists (EURETINA). Br J Ophthalmol. 2014;98:1144–67.
Amsler M. L’Examen qualitatif de la fonction maculaire. Ophthalmologica. 1947;114:248–61.210.1159/000300476.
Westheimer G. Editorial: visual acuity and hyperacuity. Invest Ophthalmol. 1975;14:570–2.
Simunovic MP. Metamorphopsia and its quantification. Retina. 2015;35:1285–91.
Faes L, Bodmer NS, Bachmann LM, Thiel MA, Schmid MK. Diagnostic accuracy of the Amsler grid and the preferential hyperacuity perimetry in the screening of patients with age-related macular degeneration: systematic review and meta-analysis. Eye. 2014;28:788–96.
Crossland M, Rubin G. The Amsler chart: absence of evidence is not evidence of absence. Br J Ophthalmol. 2007;91:391–3.
Fine AM, Elman MJ, Ebert JE, Prestia PA, Starr JS, Fine SL. Earliest symptoms caused by neovascular membranes in the macula. Arch Ophthalmol. 1986;104:513–4.
Chew EY, Clemons TE, Bressler SB, Elman MJ, Danis RP, Domalpally A, et al. Randomized trial of the ForeseeHome monitoring device for early detection of neovascular age-related macular degeneration. The HOme Monitoring of the Eye (HOME) study design—HOME Study report number 1. Conte Clin Trials. 2014;37:294–300.
Schwartz R, Loewenstein A. Early detection of age related macular degeneration: current status. Int J Retin Vitr. 2015;1:20.
Lienhard KR, Legner C. Principles in the design of mobile medical apps: guidance for those who care. In: Proceedings of the 13th International Conference on Wirtschaftsinformatik (WI), St Gallen, Switzerland; 2017.
Geisler WS. Physical limits of acuity and hyperacuity. J Opt Soc Am A. 1984;1:775–82.
Keane PA, de Salvo G, Sim DA, Goverdhan S, Agrawal R, Tufail A. Strategies for improving early detection and diagnosis of neovascular age-related macular degeneration. Clin Ophthalmol. 2015;9:353–66.
Schmid MK, Faes L, Bachmann LM, Thiel MA. Accuracy of a self-monitoring test for identification and monitoring of age-related macular degeneration: a diagnostic case–control study. Open Ophthalmol J. 2018;12:19–28.
Kaiser PK, Wang YZ, He YG, Weisberger A, Wolf S, Smith CH. Feasibility of a novel remote daily monitoring system for age-related macular degeneration using mobile handheld devices: results of a pilot study. Retina. 2013;33:1863–70.
Wang YZ, He YG, Mitzel G, Zhang S, Bartlett M. Handheld shape discrimination hyperacuity test on a mobile device for remote monitoring of visual function in maculopathy. Invest Ophthalmol Vis Sci. 2013;54:5497–505.
Wang YZ, Wilson E, Locke KG, Edwards AO. Shape discrimination in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2002;43:2055–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LMB, MAT, KL, and MKS are founders of Oculocare medical Inc., which develops innovative products in eye care, such as the self-monitoring test described in this paper. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schmid, M.K., Thiel, M.A., Lienhard, K. et al. Reliability and diagnostic performance of a novel mobile app for hyperacuity self-monitoring in patients with age-related macular degeneration. Eye 33, 1584–1589 (2019). https://doi.org/10.1038/s41433-019-0455-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0455-6
This article is cited by
-
Remote Monitoring of Visual Function in Patients with Maculopathy: The Aphelion Study
Ophthalmology and Therapy (2024)
-
Teleophthalmology and retina: a review of current tools, pathways and services
International Journal of Retina and Vitreous (2023)
-
System usability, user satisfaction and long-term adherence to mobile hyperacuity home monitoring—prospective follow-up study
Eye (2023)
-
Home vision monitoring in patients with maculopathy: current and future options for digital technologies
Eye (2023)
-
Transforming ophthalmology in the digital century—new care models with added value for patients
Eye (2023)