Abstract
Objectives
To determine whether administration of local anaesthetic at the site of skin incision during open lacrimal drainage surgery under general anaesthesia alters the total dosage of anaesthetic drugs required during total intravenous anaesthesia (TIVA), and whether it alters postoperative pain and recovery.
Study design
Masked comparison of a randomized, two-group interventional study.
Patients and methods
Patients undergoing unilateral external dacryocystorhinostomy under total intravenous general anaesthesia were recruited from the lacrimal service at Moorfields Eye Hospital between September 2012 and February 2014. The patients were randomised to receive, after induction and stabilisation of general anaesthesia, infiltration of the ipsilateral paranasal tissues with 2.5 ml of 0.5% bupivacaine with 1:100000 epinephrine (“treatment” group), or a sham injection (“control” group); the infiltration was performed about 7 min prior to the skin incision. The infusion rates for propofol and remifentanil were adjusted to maintain a steady intra-operative mean blood pressure of 55–70 mmHg and BIS score of 40–60%. The time taken for extubation of the patient after cessation of TIVA was recorded, and postoperative pain scores (on a Likert scale from 0–10) were taken at regular intervals after extubation. The average intra-operative mean blood pressures, total drug usage, extubation time and pain scores for each of the two groups were compared using two-tail Student's t-testing and Wilcoxon rank sum testing.
Results
There were 12 patients (7 female; 58%) in the treatment group and 11 (7 female; 64%) in the control group, with similar average age at surgery (59 years treatment, 53 years control; p = 0.38) The average operative time was 45 min in the treatment group (median 42, range 30–55) and 47 min (median 45; range 37–61) in the control group (p = 0.52). The mean dosage of propofol required to maintain satisfactory GA was significantly less in the “treatment” group (89.8 mcg/kg/min) as compared to the “control” group (mean 126 mcg/kg/min) (p = 0.0007). Likewise, remifentanil dosage was significantly less in the “treatment” group (100 ng/kg/min) as compared to controls (259 ng/kg/min) (p = 0.00007). The mean non-invasive blood pressure was consistently lower during surgery in the “treated” group, and showed less intra-operative variation. After surgery, the patients receiving LA had a significantly shorter extubation time (mean time 6.0 min in “treated” group, 12.1 min in “controls”; P < 0.0002) and also significantly lower pain scores at 10, 30, 60, 120 and 180 min after extubation (p < 0.01, p < 0.01, p < 0.01, p < 0.01 and p < 0.05, respectively).
Conclusions
Ipsilateral infiltration of local anaesthesia containing epinephrine in the paranasal tissues just prior to open dacryocystorhinostomy under total intravenous anaesthesia is associated with a 28% reduction in mean propofol usage, and a 61% reduction in remifentanil usage. LA usage during GA also produces improved and less variable intra-operative mean blood pressures, a significantly shorter extubation time and significantly lower postoperative pain scores.
Similar content being viewed by others
Introduction
External dacryocystorhinostomy (DCR) can successfully be performed under general or local anaesthesia (LA), with or without sedation and both approaches have some merits [1,2,3]. General anaesthesia (GA) maybe preferred over LA only for its versatility in allowing controlled hypotension—with potentially less operative blood loss—and provision of complete patient analgesia and unconsciousness [4].
Surgery under GA can be supplemented with infiltration of LA, sometimes with admixed epinephrine to promote local vasoconstriction, although usage of this is not consistent [4].
External DCR has been performed as a day case at Moorfields Eye Hospital for many years [5], this being facilitated in recent years by total intravenous anaesthesia (TIVA), using target-controlled infusions of propofol (a hypnotic) and remifentanil (an ultra-short-acting opiate). Anecdotal experience at Moorfields Eye Hospital had suggested to one author (MJA) that, in patients undergoing adnexal surgery under GA, pre-operative LA infiltration of the incision site reduces not only the “volatility” of intra-operative blood pressures, but also the quantity of anaesthetic drugs required during surgery.
This prospective, masked study was designed to investigate whether pre-operative infiltration of LA during DCR under GA alters the total requirement for anaesthetic agents to maintain satisfactory operating conditions, and whether this was associated with changes in postoperative analgesia and recovery.
Methods
The study was a prospective, randomized and single masked investigation with appropriate Institutional board review; it adhered to tenets of the Declaration of Helsinki.
Patients requiring unilateral DCR at Moorfields Eye Hospital were offered participation in the study, and exclusion criteria included age <18 years, patients without capacity for consent, and those in whom GA was contraindicated.
Randomisation was provided by the Moorfields Research Department, the assignment being notified (to the surgeon alone) immediately prior to anaesthesia. Both groups underwent surgery under TIVA but—after stabilization of the GA—one group received ipsilateral paranasal infiltration with 2.5 ml of 0.5% bupivacaine with 1:100000 epinephrine (“treated” group). For “untreated” patients (“control” group), the preparatory sequence was identical, but the local anaesthesia was returned unused to the surgical assistant; because of the arrangements of drapes, the anaesthetist was unable to ascertain whether or not local anaesthesia had been administered.
During surgery the heart rate, mean arterial pressure and bispectral index (BIS monitor: Medtronic Limited) were recorded every 5 min.
All surgery was performed by a single surgeon (DHV) and GA by the same anaesthetist (MJA). Reverse Trendelenberg positioning to 15° head-up (verified by clinometer) was set for all patients during surgery and, in all cases, 3 cotton-buds moistened with 1:1000 epinephrine were positioned antero-superiorly within the ipsilateral nasal space. External DCR was performed in accordance with a previously published technique [6].
General anaesthesia
All GA was to a fixed protocol (Appendix 1): after induction of anaesthesia and establishment of a safe airway with assisted ventilation, anaesthesia was maintained using continuous intravenous infusions of remifentanil (40 mcg/ml) and propofol 2% (20 mg/ml). The infusion rates of each drug were adjusted throughout surgery to maintain pre-defined physiological parameters—that of remifentanil being used to alter (and try to maintain a near-constant) mean non-invasive arterial pressure (MAP) and that of propofol being adjusted to maintain a constant depth of anaesthesia, as measured by Bispectral Index (BIS) monitoring. The MAP was maintained at 55–70 mmHg, and the BIS at 40–60%, these parameters being measured (and acted upon) every 5 min throughout the procedure. At the end of surgery each patient received 0.1 mg of intravenous morphine sulfate.
The interval from cessation of TIVA to extubation was recorded and, whilst in the recovery area, all patients completed a standardised visual analogue pain and nausea questionnaire (11 point Likert scale) at regular times after surgery. Nursing staff were permitted to impartially record the patient’s pain and nausea scores, and all responses were independent of the operative surgeon and anaesthetist.
Outcomes and analysis
The primary outcomes measures were (a) the required dosage (mcg/kg/minute-propofol or ng/kg/minute-remifentanil, calculated for each patient) of each TIVA drug used, (b) the time (min) taken to extubate the patient once TIVA had ceased and (c) the postoperative pain and nausea scores. Other collected data included the patient’s age, gender, weight, the operative time from incision to final skin suture, requirement for analgesia over the first 3 h after surgery and any complications during or after surgery.
Parametric variables were compared by 2-tail Student's t-testing, and non-parametric measures compared with Wilcoxon rank sum testing. An α-risk of 0.05 was considered clinically significant.
Results
Twenty-three (14 female; 61%) patients completed the study, 11 under GA alone (“Control” Group 1) and 12 under GA with paranasal LA infiltration (Group 2). The patient age, weight, body mass index (BMI), and duration of surgery were similar in both groups (Table 1).
Although—as compared to the control (GA) group—the mean heart rate in the treatment (GA + LA) group was slightly higher at each time point, there was no major difference between each group (Table 1). Likewise, the mean arterial pressure showed a peak in the control group at 5 min, but thereafter settled to steady levels in both groups (Table 1). The mean BIS showed only minor variation between groups at each time point, and ranged from 40–45 in the GA group to 39–43 in the GA + LA group (Table 1).
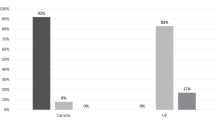
The mean quantity of intravenous anaesthesia agents required to maintain GA showed a highly significant difference between the two groups (Table 2): a mean patient dosage of remifentanil was 259 ng/kg/min (median 241; range 119–457) in the control group under GA alone, as compared to 100 ng/kg/min (median 100; range 39.0–188) for surgery under GA with LA infiltration (treatment group; 39% of control dosage; p = 0.00007). Similarly, the mean propofol dosage was 126 mcg/kg/min (median 127; range 94.4–183) for GA alone (control group), compared with 89.8 mcg/kg/min (median 88.4; range 65.3–120) for GA with LA infiltration (treatment group; 71% of control dosage; p = 0.0007).
The average extubation time from cessation of surgery was 6.5 min (median 5.5; range 3–12) in the treatment group, as compared to 12.1 min with GA alone (median 13; range 6–17) (p = 0.0008; Wilcoxon rank sum). Postoperative pain showed major differences between the two groups at 10, 30, 60, 120 and 180 min after surgery (Table 2); the highest mean score of 0.64 at 10 min after surgery in the treatment (GA + LA) group contrasts with the average score of 5.3 in the control group at this time. In both groups, postoperative nausea was absent or mild in almost all patients after surgery. Intra-operative blood loss was less than 50 mls in each patient, and there were no intra-operative or postoperative complications.
Discussion
This prospective, randomized study has shown that paranasal local anaesthetic infiltration under general anaesthesia has three major benefits: First, a need for only 39% of the usual dosage of intravenous remifentanil for maintaining stable GA, and about 30% less propofol; secondly, a significantly faster extubation time; and, thirdly, a major reduction in postoperative pain scores.
Many studies have reported surgical and patient outcomes for general surgery under LA or GA [7, 8], but there are very few accurate comparisons for GA as compared to GA with LA. Combining regional infiltration with general anaesthesia in abdominal surgery has been used for a century, with authors of that period advocating the benefits of “local nociceptor blockade” to facilitate a ‘light ether or nitrous oxide general anaesthesia’, and to mitigate the risk of shock [9, 10]. A systematic review from 1995 found 6/7 studies to not demonstrate a benefit from combining LA with GA [11], but a later review cited 9 published studies in which local or epidural anaesthesia was beneficial when combined with GA [12]; none of these studies included ophthalmic surgery. As with our study, many of these papers record that LA infiltration during GA is associated with less postoperative pain, and addition of epidural anaesthesia during abdominal surgery under GA allowed patients to wake faster and require half the amount of intravenous opiate during surgery [13]. Our investigation similarly showed that paranasal LA infiltration reduced the intra-operative opiate requirement to just 39% of that under GA alone (100 vs. 259 mcg/kg/min), and the extubation time was nearly halved with combined LA and GA (6.5 vs. 12 min).
In Ophthalmic surgery pre-emptive peribulbar LA during vitreoretinal surgery under GA has been reported to reduce the oculo-cardiac reflex, and reduce pain and vomiting after surgery [14,15,16,17]. Postoperative nausea was rare with our patients, possibly because they all received prophylactic 5HT3 antagonists. In oculoplastic literature one study demonstrated that pre-incisional retrobulbar LA was associated with lower intra-operative blood pressure and reduced postoperative pain. To our knowledge no other ophthalmic studies have demonstrated the physiological effect of reduced general anaesthesia agents and the faster extubation noted in our investigation.
Multiple ascending and descending pathways in the central and peripheral nervous system are known to modulate pain perception [12, 18] and, by attenuation of inhibitory mechanisms, repeated stimulation of peripheral nociceptors may sensitize central pain pathways. Likewise, peripheral stimulation within a “primed” central nervous system may induce a stronger synaptic response—this reducing the usually high threshold potential for peripheral nociceptor activation. Neuronal plasticity may also lead to “receptive field expansion”, with recruitment and activation of afferent fibres outside the original area of stimulation, and further amplifying the noxious sensation. LA may attenuate or halt this neurosensitization “cascade”—as illustrated by assays of serum beta-endorphins, a marker for pain receptor activation. Intra-operative beta-endorphin levels more than double during tooth extraction under GA, whereas addition of LA during GA blocked any significant rise of beta-endorphins [19].
The safety of modern general anaesthesia is excellent and, although postoperative delirium and cognitive decline does not appear more prevalent in GA as compared to LA, there still exist concerns about such side effects of GA [20, 21]; in this context, the significant reduction in total dosage of GA agents required in our patients can only be beneficial. Intra-operative stress and raised noradrenaline levels have, moreover, been associated with a greater risk of postoperative delirium [22].
There are significant cost savings with the markedly reduced total dosage of propofol and remifentanil, and the significantly faster extubation time should improve operating theatre utilization; the 6 min reduction should be viewed in the light of an estimated theatre cost of £1200 per hour in the National Health Service [23]. It is likely that these findings are applicable to other ophthalmic, oculoplastic or surgical procedures under general anaesthesia.
Summary
What was known before
-
Dacryocystorhinosotmy may be performed under general anaesthesia or/and LA.
-
Adding LA to general anaesthesia may result in reduced postoperative pain. Using LA in while undergoing general anaesthesia surgery may result in lower intra-operative blood pressure
What this study adds
-
Infiltration of LA in patients under general anaesthesia for DCR surgery results in reduced general anaesthesia requirements . Adding LA results in faster extubation of patients and reduced postoperative pain.
References
McNab AA, Simmie RJ. Effectiveness of local anaesthesia for external dacryocystorhinostomy. Clin Exp Ophthalmol. 2002;30(4):270–2.
Ciftci F, Pocan S, Karadayi K, Gulecek O. Local versus general anesthesia for external dacryocystorhinostomy in young patients. Ophthal Plast Reconstr Surg. 2005;21(3):201–6.
Knežević MM, Vlajković GP, Stojković MŽ, Rašić DM, Stanković BR, Božić MM. Comparison of postoperative pain and satisfaction after dacryocystorhinostomy in patients operated on under local and general anesthesia. Med Sci Monit. 2012;18(5):CR265–70.
Hart RH, Allen M, Rose GE. In: Adam JC, Michael M, Brian B, editors. The Lacrimal System: Diagnosis, Management, and Surgery, 2nd Edition. New york: Springer-Verlag; 2014.
Hanna IT, Powrie S, Rose GE. Open lacrimal surgery: a comparison of admission outcome and complications after planned day case or inpatient management. Br J Ophthalmol. 1998;82:392–6.
Verity DH, Rose GE. External dacryocystorhinostomy. In: Albert DM, Lucarelli MJ, Eds. Clinical atlas of procedures in ophthalmic and oculofacial surgery.. Chapter 98. Oxford: Oxford University Press; 2012. p. 1021–32.
Vaniyapong T, Chongruksut W, Rerkasem K. Local versus general anaesthesia for carotid endarterectomy. Cochrane Database Syst Rev. 2013;19(12):CD000126.
Al-Moraissi EA, Ellis E 3rd. Local versus general anesthesia for the management of nasal bone fractures: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2015;73(4):606–15.
Crile GW. The kinetic theory for shock and its preven- tion through anoci-association (shockless operation). Lancet. 1913;ii:7–16.
Ryfkogel HA, Carlson E. The use of local anaesthesia alone or combined with general anaesthesia in abdominal surgery. Cal West Med. 1926;25(1):65–70.
McQuay HJ. Pre-emptive analgesia: a systematic review of clinical studies. Ann Med. 1995;27(2):249–56.
Kaufman E, Epstein JB, Gorsky M, Jackson DL, Kadari A. Preemptive analgesia and local anesthesia as a supplement to general anesthesia: a review. Anesth Prog. 2005;52(1):29–38. Spring
Handley GH, Silbert BS, Mooney PH, Schweitzer SA, Allen NB. Combined general and epidural anesthesia versus general anesthesia for major abdominal surgery: postanesthesia recovery characteristics. Reg Anesth. 1997;22(5):435–41.
Shende D, Sadhasivam S, Madan R. Effects of peribulbar bupivacaine as an adjunct to general anaesthesia on peri-operative outcome following retinal detachment surgery. Anaesthesia. 2000;55(10):970–5.
Ghali AM, El Btarny AM. The effect on outcome of peribulbar anaesthesia in conjunction with general anesthesia for vitreoretinal surgery. Anaesthesia. 2010;65(3):249–53.
Subramaniam R, Subbarayudu S, Rewari V, Singh RP, Madan R. Usefulness of pre-emptive peribulbar block in pediatric vitreoretinal surgery: a prospective study. Reg Anesth Pain Med. 2003;28(1):43–7.
Yeatts RP, Doneyhue W, Scuderi PE, Brasington CR, James R. Effect of preemptive retrobulbar analgesia on perioperative hemodynamics and postoperative pain after enucleation. Ophthal Plast Reconstr Surg. 2004;20(3):226–31.
Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288(5472):1765–9. Review
Gordon SM, Dionne RA, Brahim J, Jabir F, Dubner R. Blockade of peripheral neuronal barrage reduces postoperative pain. Pain. 1997;70(2-3):209–15.
GL Bryson, Wyand A. Evidence-based clinical update: general anesthesia and the risk of delirium and postoperative cognitive dysfunction. Can J Anaesth. 2006;53(7):669–77.
Paredes S, Cortínez L, Contreras V, Silbert B. Post-operative cognitive dysfunction at 3 months in adults after non-cardiac surgery: a qualitative systematic review. Acta Anaesthesiol Scand.2016;60:1043–58.
Deiner S, Lin HM, Bodansky D, Silverstein J, Sano M. Do stress markers and anesthetic technique predict delirium in the elderly? Dement Geriatr Cogn Disord. 2014;38(5-6):366–74.
The Productive Operating Theatre team. The NHS Institute for Innovation and Improvement. www.institute.nhs.uk/theatres. Accessed on October 2017.
Acknowledgements
The authors thank Dr. Catey Bunce, lately senior medical statistician at Moorfields Eye Hospital, for her advice and assistance with this work. Professor Geoffrey Rose receives some funding from the Department of Health’s NIHR Biomedical Research Centre for Ophthalmology at Moorfields Eye Hospital and UCL Institute of Ophthalmology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Appendix 1: Anaesthetic protocol for DCR Study
Appendix 1: Anaesthetic protocol for DCR Study
A single protocol-driven approach was utilized, by a single consultant anaesthetist (MJA) throughout this investigation.
Pre-operative preparation
Patient was pre-medicated on ward with oral metoclopramide (10 mg) and ranitidine (150 mg).
Induction and maintenance of anaesthesia
Intravenous anaesthetic agents were prepared at these concentrations: remifentanil (40 mcg/ml) and propofol 2% (20 mg/ml).
The following anaesthetic sequence was employed in each patient:
-
IV access was established in the dorsum of the patient’s hand (22 g cannula)
-
Standard monitoring attached—Bispectral Index Monitor (BIS), ECG, SPO2 and NIBP
-
Note was made of baseline pulse rate, blood pressure & BIS (Time “0”)
-
The patient was pre-oxygenated with 100% oxygen for 3 min
-
Commence 500mls of Hartmann’s solution over 1 h (~25 drips every 10 s)
-
An induction bolus of remifentanil (1 mcg/kg) was given, followed by an infusion rate of 0.20 mcg/kg/min; thereafter the remifentanil rate was titrated according to the patient’s BP
-
The propofol infusion was then be started at 6 mcg/ml, together with a 40 mg bolus of intravenous lidocaine, to reduce any pain associated with the propofol infusion
-
The propofol infusion was reduced to 3 mcg/ml when the patient was asleep, and the rate then titrated according to BIS readings
-
Satisfactory ventilation was checked and atracurium given (0.5 mg/kg)
-
2 min later cuffed endotracheal intubation was placed (7.0 mm for women; 7.5 mm for men)
-
A throat pack was placed and ventilation set to maintain an End-tidal CO2 of 4.0–4.5 kPa
-
Dexamethasone 8 mg, ondansetron 8 mg, paracetamol 1 g and cefuroxime 1.5 g were all given before surgery
-
When starting suture of the posterior mucosal flaps, 0.1 mg/kg intravenous morphine sulfate was given to all patients
Control of Target MAP to 55–70 mmHg
If MAP was >70 mmHg: the remifentanil infusion was increased, up to a maximum of 0.6 mcg/kg/min. If the MAP remains >70 mmHg 5 min later (at the next check), administration of labetolol (0.1 mg/kg) was considered if the heart rate was > 70bpm—or hydralazine (0.1 mg/kg) if the heart rate was 70 bpm or less.
If MAP <55 mmHg: the infusion rates for both anaesthetic agents were adjusted, and ephedrine 6 mg given until BP restored. An anticholinergic drug was considered if the heart rate was <50bpm.
Control of Target BIS (40–60%)
If BIS > 60%, the infusion site was checked and propofol dosage increased up to a maximum of 5 mcg/ml. If BIS remained > 50%, the infusion site was checked and addition of sevoflurane inhalation anaesthesia considered.
If BIS < 40%, then the rate of propofol infusion was reduced.
Rights and permissions
About this article
Cite this article
Scawn, R.L., Allen, M.J., Rose, G.E. et al. Randomised, masked study of local anaesthesia administered prior to external dacryocystorhinostomy under general anaesthesia. Eye 33, 374–379 (2019). https://doi.org/10.1038/s41433-018-0201-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0201-5