Abstract
BRCA1-associated protein-1 (BAP1) is a recognised tumour suppressor gene. Germline BAP1 pathogenic/likely pathogenic variants are associated with predisposition to multiple tumours, including uveal melanoma, malignant pleural and peritoneal mesothelioma, renal cell carcinoma and specific non-malignant neoplasms of the skin, as part of the autosomal dominant BAP1-tumour predisposition syndrome. The overall lifetime risk for BAP1 carriers to develop at least one BAP1-associated tumour is up to 85%, although due to ascertainment bias, current estimates of risk are likely to be overestimated. As for many rare cancer predisposition syndromes, there is limited scientific evidence to support the utility of surveillance and, therefore, management recommendations for BAP1 carriers are based on expert opinion. To date, European recommendations for BAP1 carriers have not been published but are necessary due to the emerging phenotype of this recently described syndrome and increased identification of BAP1 carriers via large gene panels or tumour sequencing. To address this, the Clinical Guideline Working Group of the CanGene-CanVar project in the United Kingdom invited European collaborators to collaborate to develop guidelines to harmonize surveillance programmes within Europe. Recommendations with respect to BAP1 testing and surveillance were achieved following literature review and Delphi survey completed by a core group and an extended expert group of 34 European specialists including Geneticists, Ophthalmologists, Oncologists, Dermatologists and Pathologists. It is recognised that these largely evidence-based but pragmatic recommendations will evolve over time as further data from research collaborations informs the phenotypic spectrum and surveillance outcomes.
Similar content being viewed by others
Introduction
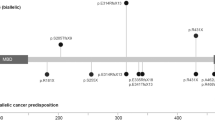
BRCA1-associated protein-1 (BAP1) was identified as a tumour suppressor gene in 2008 [1]. Germline pathogenic variants (GPV, including likely pathogenic variants) in BAP1 have subsequently been associated with a variety of tumours resulting in the recognition of BAP1-associated tumour predisposition syndrome (BAP1-TPDS) [2, 3]. GPV were originally associated with familial occurrence of cutaneous melanocytic tumours but the spectrum of tumours is now accepted to include uveal melanoma, malignant mesothelioma of the pleura and the peritoneum, renal cell carcinoma and specific non-malignant neoplasms of the skin. More recently additional tumour types including meningioma, cholangiocarcinoma and hepatocellular carcinoma have been suggested as possible associations with BAP1-TPDS [2, 4].
Lifetime cancer risks for individuals with a BAP1 GPV (henceforth referred to as BAP1 carriers) are reported to be 20–25% for mesothelioma, uveal and cutaneous melanoma, with lower lifetime risks reported for renal cell carcinoma and other associated cancers. The overall lifetime risk for at least one BAP1-associated tumour is up to 85% [2, 5]. However, due to ascertainment bias, current estimates of cancer risk are likely to be overestimated.
BAP1 GPV are inherited in an autosomal dominant manner and once a GPV is identified in an individual, predictive (also known as pre-symptomatic) testing can be offered to relatives. This facilitates assessment of cancer risk and discussion of options for early detection and/or cancer prevention. De novo GPV in BAP1 have been reported in almost 10% (2/21) in a Dutch patient cohort [4]. The exact incidence is unknown but considered low.
For almost all rare cancer predisposition syndromes there is limited scientific evidence of reduced morbidity or mortality for surveillance, meaning it is difficult to achieve the fine balance between too much surveillance (leading to unnecessary further investigations such as biopsy), and too little (resulting in missed opportunities to detect a cancer at a treatable stage). Opinions on surveillance can vary greatly between clinicians based on experience and the health care systems in which they work.
Whilst surveillance guidelines have been published from American and Australian groups [5, 6] (Supplementary Table 1) there remains limited evidence and conflicting recommendations. To date, European recommendations have not been published. In a survey of UK Genetics centres in late 2019, BAP1 was identified as a gene considered to be a priority for guideline development (personal communication H. Hanson). Guidelines are necessary due to both the emerging phenotype of this recently described syndrome and increased identification of BAP1 GPV carriers via large gene panels. It is important to consider the European model of healthcare, in which services are, in general, funded through taxes and/or social contributions. Thus, guidelines need to consider both the cost and burden on healthcare systems, as well as the balance of desirable versus undesirable outcomes and quality of evidence.
To address these issues, the Clinical Guideline Working Group of the CanGene-CanVar project in the United Kingdom invited European collaborators to join them to develop guidelines for BAP1 carriers to harmonize surveillance programmes within Europe. The recommendations are summarised in this report.
Scope of the guideline
The overarching aim of the guidance is to provide a resource to healthcare professionals to aid in the identification and surveillance of individuals with BAP1-TPDS by considering a number of key questions (Table 1). It was decided that the management and treatment of specific tumours associated with BAP1 GPV and assessment of BAP1 variants of uncertain significance was outside the scope of this guideline. It is important to note that these guidelines do not represent a legal standard of care, and whilst they should support clinical practice, they should not replace clinical judgement.
Methods
CanGene-CanVar (a Cancer Research UK funded research group) commissioned the guidelines and invited clinicians from the UK and Europe to participate in the expert clinical group. The core group consisted of 10 members and an extended expert group of 34 additional members. Members of the group were invited due to a known interest in this area and via email invitation to the European Reference Network for genetic tumour risk syndromes (ERN GENTURIS) group to ensure that relevant clinical specialties were represented, including Genetics, Ophthalmology, Oncology, Dermatology and Pathology.
The scope and purpose of the guidelines were initially discussed in November 2020, following which a set of key questions were formulated (Table 1).
The core group members had six virtual meetings between November 2020 and June 2022 to discuss the questions, agree on methodology and allocate specific topics to each member of the core group. A literature search was undertaken in January 2021 with predefined search terms, using PUBMED and subsequent extended searches via citation chasing and limiting to articles in English. Evidence levels and recommendations were assessed using a modified GRADE system as utilised by the ERN GENTURIS network in PTEN Hamartoma Tumour Syndrome (PHTS) guideline development [7]. The questions were reviewed and initial draft statements formulated by the core group to be reviewed by the extended group via a modified electronic Delphi process methodology [8]. Delphi is a structured process in which opinions of a large number of experts are gathered on statements for which there is limited or weak evidence. Each statement was scored by each member of the group using a five-point scale (strongly disagree to strongly agree). To achieve consensus, at least 80% agreement of respondents to that statement was required. Where there was disagreement and an 80% consensus not reached, the comments and discussion from the Delphi group were used to amend recommendations for a subsequent round of Delphi. If consensus was not reached after two rounds, the statement was excluded from the final guidelines. Even if consensus was met, the statements were still modified if comments indicated clearer wording or format. The results of the Delphi survey were reviewed by the core group to agree the final statements and recommendations.
Results
As is common within the rare disease field, there is limited peer-reviewed evidence available to inform guideline development with only limited numbers of BAP1 carriers reported in the literature (Supplementary Table 2) and scant evidence addressing surveillance within this patient group.
In round 1 of the Delphi, 29 statements reached consensus (80% or greater consensus) and 13 did not. For Delphi round 2, 23 statements were put forward (13 that did not achieve consensus and 10 reworded following comments on clarity or consistency). At the end of round 2, consensus was reached on all but four statements. The final recommendations are detailed in Table 2a–d, with the evidence weighting using the modified GRADE system outlined in the ERN GENTURIS PHTS guidelines [7] (Strong evidence: Consistent evidence and new evidence unlikely to change recommendation and expert consensus; Moderate evidence: Expert consensus or majority decision but with inconsistent evidence or significant new evidence expected and weak evidence: inconsistent evidence and limited expert agreement).
Rationale for the recommendations
Phenotype and prevalence of germline BAP1 pathogenic variants
In 2016 Rai et al. undertook a literature review to assess the phenotypic spectrum of BAP1 –TPDS [5]. They noted that 31% (54/174) of BAP1 carriers were diagnosed with a uveal melanoma, 22% (39/174) had a malignant mesothelioma (26/39 of which were pleural), 13% (23/174) of cases had a cutaneous melanoma and 10% (18/174) had renal cell carcinoma. A subsequent comprehensive literature review of 181 families with GPV in BAP1 by Walpole et al. [2] assessed cancers associated with BAP1 GPV and suggested that mesothelioma (peritoneal and pleural), uveal melanoma, cutaneous melanoma, and renal carcinoma are core cancers in the phenotype, occurring in 24.5%, 36.2%, 23.4%, and 5.7% of 141 proband carriers and 16.9%, 15.9%, 12.0%, and 4.9% of 183 non-proband carriers respectively. BAP1-inactivated melanocytic tumours (BIM) have since been considered to be a feature of BAP1-associated tumour syndrome, identified in up to 72% of cases [9, 10]. Other cancers proposed to be associated with BAP1 GPV include meningioma, hepatocellular carcinoma, cutaneous basal cell cancer and cholangiocarcinoma [11,12,13].
In agreement with Walpole et al. [2], consensus was achieved that mesothelioma (peritoneal and pleural), uveal melanoma, cutaneous melanoma, and renal carcinoma, along with BIM are core cancers associated with BAP1-TPDS. The group also agreed that the evidence supports an association for meningioma, but that it should not be considered part of the core phenotype. Further evidence was required to confirm an association for hepatocellular carcinoma, cholangiocarcinoma or other cancers (Table 2a).
The group also discussed the potential association of specific histological subtypes of cancer with BAP1 GPV, specifically whether rhabdoid compared to non-rhabdoid meningioma is more strongly associated as suggested by some studies [14] or whether a specific type of renal cancer is associated with BAP1 GPV. After two Delphi rounds, consensus was not achieved, and it was felt that further studies are required to support an association of specific histological subtypes.
Prevalence of BAP1 pathogenic variants
Population studies of patients with cutaneous melanoma, ocular melanoma, malignant mesothelioma, and renal cell carcinoma identified BAP1 GPV in less than 1% of patients [15,16,17]. Subsequent studies have refined the criteria to improve detection rates, using additional information from tumour based testing or personal/family history of BAP1- associated tumours.
The Danish registry study [18] demonstrated a 25% detection rate in cutaneous melanoma families with two or more cases of uveal melanoma as well as cutaneous melanoma. Familial uveal melanoma is far more likely to be due to BAP1 GPV than sporadic cases with a pick up rate of 25% [19].
Panou et al. [20] undertook mutation testing in 195 cases of mesothelioma but only identified six BAP1 GPV. Of these, four cases had a family history of a BAP1-associated tumour, one had personal history of another malignancy and one was an isolated case, again demonstrating a higher detection rate in the presence of relevant personal or family history.
The probability of identifying a GPV in BAP1 is also low in most cases of renal cell carcinoma (RCC). Popova et al. [21] described the association of RCC with BAP1 GPV in 2013 in a family with multiple cancer types and four first-degree relatives with RCC; however, on evaluation of 32 other RCC families they failed to identify any further BAP1 GPV. Other studies assessing familial cases of RCC also failed to identify any GPV [22]. A large study of 254 cases with advanced renal cell carcinoma identified BAP1 GPV in 1% (3/254) of cases. All of these tumours demonstrated loss of BAP1 on IHC [23]. There is some suggestion that early onset cases may have an increased pick up rate although Wu et al. [24] only identified 3 BAP1 GPV in 190 cases (1.6%) diagnosed under 45 years of age.
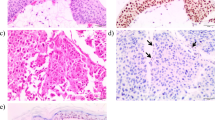
Cabaret et al. [9] identified BAP1 GPV in 24% (12/49) of individuals with BIM demonstrating loss of BAP1 on immunohistochemistry (IHC). The majority of the patients with a BIM demonstrating loss of BAP1 on IHC and a BAP1 GPV had a personal or family history of any other BAP1 associated tumour (10/12 cases).
Meningioma has been proposed as part of BAP1-TPDS. However, the data around the prevalence of mutations are limited. Shankar et al. [11] demonstrated a detection rate of BAP1 GPV of 3% in the rhabdoid subtypes (an uncommon aggressive form). However, rhabdoid subtypes are rare and thus the evidence is limited and consensus was not achieved for an association with a particular subtype.
Likewise, cholangiocarcinoma has been investigated due to the high somatic mutation rate in BAP1 in these tumours [12, 25]. However, only a single BAP1 GPV was identified in 131 cases (0.7%) in an individual with a family history of BAP1- associated tumours. Other germline cases described have been in individuals with a personal or family history of BAP1-associated tumours [13, 26].
Conversely, somatic variants in BAP1 are common in a number of malignancies. Carbone et al. [27] reviewed the literature and stated that somatic variants of BAP1 were identified in 60–70% of mesotheliomas, 45% of uveal melanomas, 15% of renal cell carcinomas, and 5% of cutaneous melanomas. Somatic BAP1 mutations have also been identified in other malignancies, including cholangiocarcinoma and thymic cancers. A recent paper has confirmed these somatic variant rates [28].
BAP1 germline testing indications
As for many other cancer predisposition genes, existing BAP1 testing criteria have generally been based on personal history of BAP1-TPDS associated tumours or a personal and family history of BAP1-TPDS associated tumours [5]. More recent guidelines have suggested the addition of young age of onset of a BAP1-associated tumour [4]. Whilst in general, thresholds for genetic testing are decreasing due to diminishing costs and labour of genetic testing, most European countries apply a threshold at which genetic testing can be offered. In the UK and other European countries this has historically been set at approximately 10%, with the exception of genes where there are therapeutic implications for cancer management and/or clear risk reducing interventions, where lower thresholds may be considered.
The implementation of next generation sequencing gene panels, facilitating testing for specific indications have resulted in much broader eligibility criteria e.g., panels for inherited renal cancer or familial melanoma https://panelapp.genomicsengland.co.uk/panels/522/https://panelapp.genomicsengland.co.uk/panels/521/. Increasing implementation of large solid tumour panel tests and paired whole genome sequencing means that BAP1 testing may also be undertaken in patients with cancer outside the known spectrum of BAP1-TPDS. At present, disease causing BAP1 variants are not on the list of ACMG actionable secondary findings due to concerns around penetrance and management of carriers in the context of identification in unrelated conditions [29].
As described in the prevalence section, the detection rate for a germline BAP1 pathogenic variant is higher where there is a personal or family history of other BAP1-associated tumours and lower for isolated cases. The group felt that targeted germline testing of BAP1 was most relevant in the situation of a strong personal or family history of BAP1-associated tumours, whereas in the case of an isolated BAP1-related tumour without other suggestive features, where the detection rate is lower, testing may be indicated based on country specific guidelines or may be more appropriate in the setting of a larger panel.
Due to the high somatic rate of BAP1 variants, it was felt that reflex BAP1 germline testing was not appropriate and the decision to proceed to germline testing should only be undertaken in the context of a BAP1-associated tumour with additional supportive information e.g., IHC loss, age of onset and personal /family history. This is consistent with the paper by Kuzbari et al. [30], suggesting that if a threshold of 10% for detection of germline variants following somatic variant detection is recommended, BAP1 germline testing should not be undertaken.
Predictive genetic testing (i.e., genetic testing for a known familial variant) should only be offered if the familial variant in BAP1 is likely pathogenic or pathogenic according to ACMG/ACP guidelines [31]. Offering predictive testing was felt to be appropriate in late teens when surveillance may start (see next section). There may be situations where testing family members for a variant of unknown significance (VUS) is helpful for the purpose of segregation studies if this helps in the evaluation of the pathogenicity of the variant. Also, when awaiting the outcome of functional testing in a research setting for a VUS, it may be appropriate to consider dermatologic and ophthalmic screening in first degree relatives, but this may be best decided in the context of specialist MDT discussion.
Cancer risks and surveillance for BAP1-associated cancer
The malignancy risk associated with germline BAP1 pathogenic variants is unclear due to limited data on long term follow up of individuals ascertained via cascade testing following a diagnostic test in an affected individual. Due to ascertainment bias, the current estimates of risk are likely to be overestimated. A summary of published studies are detailed in Supplementary Table 2.
The largest reported study of BAP1-TPDS carriers (n = 181 families) suggests that lifetime cancer risks were reported to be different for truncating compared to missense variants [2]. The frequency of cancers reported in probands with truncating and missense variants for uveal melanoma was 36% (36/141) and 23% (9/40), for melanoma 23% (33/141) and 45% (18/40), for malignant mesothelioma 25% (35/141) and 15% (6/40), and for renal cell cancer 6% (8/141) and 10% (4/40). The frequency of cancers described for the non-probands were lower suggesting ascertainment bias. The age of onset of the cancers is younger than in the general population with an estimated worse survival of cases of uveal melanoma, cutaneous melanoma and renal cell carcinoma. Conversely, there is some evidence that individuals with mesothelioma and BAP1 GPV have a better survival [32].
Uveal melanoma
Uveal melanoma (UM) is the most frequently occurring primary malignancy in the eye of adults. UM is generally assumed not to be a hereditary disease, though the occurrence of bilateral UM is more common than predicted by chance alone [33]. Furthermore, about 1–6% of patients with UM has a family history of this disease [16, 34]. A fraction of these cases can be explained by BAP1-TPDS [19].
In the largest described cohort to date, the occurrence of UM in probands of BAP1-TPDS families is 51/141 (36.2%). The occurrence in non-proband variant carriers is 29/183 (15.9%) [2]. A more recent study has estimated the point prevalence of 2.8% (95% CI 0.88–4.81%) of UM in patients with BAP1-TPDS, compared to 0.0061% in Non-Finnish population (95% CI 0.0058–0.0063%) [35]. Whilst it is clear that patients with BAP1-TPDS have an increased risk of developing UM relative to the general population, the penetrance of UM in BAP1-TPDS has not yet been completely elucidated.
Patients with BAP1-TPDS develop UM at a younger age compared to the patients with incidental UM [2]. Of the approximately 100 published cases of UM in BAP1-TPDS, the youngest patient was 15 years old. However, imaging suggested ocular melanocytosis in this patient, which is another risk factor for developing UM [25, 36]. Patients with oculo(dermal) melanocytosis have an estimated life time risk of 1/400 (0.0025%) of developing UM [8, 37]. Other studies suggest that the median age of onset of uveal melanoma in BAP1-TPDS is in the 6th decade [2, 38].
There was strong consensus from the group that regular surveillance for UM is indicated. Ophthalmological examination is non-invasive and relatively simple to perform. There is also evidence that smaller local lesions have a significantly improved prognosis compared to metastatic disease and that treating high risk smaller lesions will improve mortality [39, 40]. Surveillance may therefore lead to improved visual outcomes and better survival if UM is diagnosed at an earlier stage. Future prospective studies are needed to prove this assumption. There are few data about the required frequency of surveillance.
Skin tumours
The background incidence of malignant melanoma depends on a variety of genetic and environmental factors including skin type and sun exposure. There are a number of genetic conditions that can predispose to cutaneous melanoma with clearly established screening strategies. It has been long demonstrated that complete cutaneous examination by dermatologists increases the diagnosis of early malignant melanoma [41].
Whilst there is a clear association of cutaneous melanoma and BIM with BAP1 GPV, the exact risk of cutaneous malignancy is unclear.
Star et al. [6] postulated guidelines for BAP1 tumour surveillance which suggested that high risk melanoma surveillance be tailored for individuals with BAP1 GPV. There are data to suggest that self-examination increases the rate of diagnosis of early lesions in families with increased risk of melanoma that may be relevant to BAP1 GPV carriers [42, 43]. The group reached consensus that annual dermatological review including full body examination and photography should be offered to all BAP1 carriers, but consensus was not reached about the frequency of self-examination.
According to expert opinion, the transformation risk of BAP1-inactivated melanocytic nevi/tumours into melanoma is low, similar to atypical/dysplastic nevi (Clark nevi). Thus, the suggested clinical approach would be similar to Clark nevi. BAP1-inactivated melanocytic nevi/tumours that are clinically suspicious for melanoma following assessment by a dermatologist should be excised, Pre-emptive excision of all BAP1-inactivated melanocytic nevi/tumours may not be feasible, and the benefit of this approach remains unclear.
Mesothelioma
Mesothelioma is a rare tumour with European standardised incidence rates of 1.7 per 100,000 men and 0.4 per 100,000 women. There is a clear association with asbestos exposure but, even in those areas with very high exposure, the lifetime estimate is only about 5%. There is also a clear association with age, with risks increasing substantially from the age of 50 years. The median survival from mesothelioma is 9–12 months [44].
The lifetime risk of mesothelioma for BAP1 GPV carriers has been estimated at between 15–25% [2]. Mesothelioma is recognised as an aggressive tumour with a poor prognosis, most typically caused by asbestos exposure. To date, no surveillance programme for mesothelioma has been implemented, even for those known to be at high risk due to environmental exposure. However, there is some evidence to suggest that mesothelioma occurring as a result of a BAP1 GPV, may be associated with better survival compared to population-based cases [32, 45, 46]. Given the improved survival, the guideline group discussed that surveillance may be of use as this may allow earlier intervention. However, there are no published studies and the modality (e.g., (computed tomography [CT], magnetic resonance imaging [MRI]) and frequency of surveillance is unclear. Therefore, it was considered that surveillance for mesothelioma may only be appropriate in a research setting that allows prospective data collection and study of the long-term outcomes of screening. The U.S. National Cancer Institute (NCI) has opened two clinical trials to prospectively study frequency of mesotheliomas and other cancers in individuals with BAP1 GPV, which may address some of these questions [46].
Renal tumours
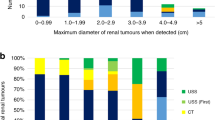
Randomised control trials of renal surveillance in BAP1 carriers have not been undertaken. Most studies have identified the frequency of renal cancer in germline BAP1 carriers, and in many studies the type of renal cancers have not been histopathologically verified. There have been reports of both multifocal and bilateral RCC in BAP1 carriers, and the average age of onset is around 10 years younger than in sporadic RCC.
However, multiple studies have shown that somatic loss of BAP1 in renal cell carcinoma is associated with a more aggressive clinical behaviour and worse prognosis [47].
In addition, a single small study of six tumours from two patients demonstrated an increased growth rate of tumours in BAP1 carriers [48]. The age at which renal cancer is diagnosed is lower in individuals with a pathogenic variant in BAP1 with a range of between 32–80 years.
Ultrasound scans are low-cost and easily available. However, whilst 77% of RCC < 30 mm are in general hyperechoic and detectable by ultrasound, a proportion are not detected [49]. The detection of isoechoic or hypoechoic tumours is more challenging, and whilst there are currently no data available regarding whether BAP1 tumours are hyperechoic, MRI could be considered as the preferred surveillance modality. This would be consistent with the recommendation for patients with hereditary leiomyomatosis and renal cell carcinoma (HLRCC) who are at risk of more aggressive renal tumours.
Consensus was reached that annual renal imaging should be offered to all BAP1 carriers, and that the preferred modality of imaging would be MRI. However, USS could be used as an alternative should MRI not be available. Given the reported age of onset of renal cancer in BAP1 carriers, starting from age 30 years reached consensus. It was recognised, as for the other tumours that long term data collection is required to evaluate the long-term benefit of surveillance.
Other recommendations for BAP1 carriers
Whilst not specifically discussed as part of the Delphi process, the core group considered that BAP1 carriers should be given appropriate lifestyle advice, including but not limited to avoiding occupations with asbestos exposure, being aware of residential exposure during renovations, non-smoking and limiting UV exposure.
Discussion
As with many rare conditions, data around management are limited. BAP1 GPV are now being identified not only in individuals with BAP1-associated tumours, but also as incidental findings as part of larger gene panels.
The currently established risk figures for malignancies associated with GPV in BAP1 are likely to be overestimates due to ascertainment bias in the reported series and long term follow up over many years will be required in order to more accurately determine risks. By virtue of the small numbers of individuals affected, randomised trials of surveillance will never be possible and long-term, prospective observation of patients undergoing surveillance is to be recommended.
These guidelines are a pragmatic approach, based on the best current available evidence along with expert opinion. We recognise the limitations of this approach, given the limited experience each individual clinician has with families with BAP1 GPV. However, a Delphi process allows for discussion with a wide group of experts in a number of clinical fields. This approach also enables consideration of the healthcare systems across Europe.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Ventii KH, Devi NS, Friedrich KL, Chernova TA, Tighiouart M, Van Meir EG, et al. BRCA1-associated protein-1 is a tumor suppressor that requires deubiquitinating activity and nuclear localization. Cancer Res. 2008;68:6953–62.
Walpole S, Pritchard AL, Cebulla CM, Pilarski R, stautberg M, Davidorf FH, et al. Comprehensive study of the clinical phenotype of germline BAP1 variant-carrying families worldwide. J Natl Cancer Inst. 2018;110:1328–41.
Pilarski R, Cebulla CM, Massengill JB, Rai K, Rich T, Strong L, et al. Expanding the clinical phenotype of hereditary BAP1 cancer predisposition syndrome, reporting three new cases. Genes Chromosomes Cancer. 2014;53:177–82.
Chau C, van Doorn R, van Poppelen NM, van der Stoep N, Mensenkamp AR, Sijmons RH, et al. Families with BAP1-tumor predisposition syndrome in The Netherlands: path to identification and a proposal for genetic screening guidelines. Cancers (Basel). 2019;11:1114.
Rai K, Pilarski R, Cebulla CM, Abdel-Rahman MH. Comprehensive review of BAP1 tumor predisposition syndrome with report of two new cases. Clin Genet. 2016;89:285–94.
Star P, Goodwin A, Kapoor R, Conway RM, Long GV, Scolyer RA, et al. Germline BAP1-positive patients: the dilemmas of cancer surveillance and a proposed interdisciplinary consensus monitoring strategy. Eur J Cancer. 2018;92:48–53.
Tischkowitz M, Colas C, Pouwels S, Hoogerbrugge N, PHTS Guideline Development Group, european Reference Network GENTURIS. Cancer Surveillance Guideline for individuals with PTEN hamartoma tumour syndrome. Eur J Hum Genet. 2020;28:1387–93.
Diamond IR, grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67:401–9.
Cabaret O, Perron E, Bressac-de Paillerets B, Soufir N, de la Fouchardière A. Occurrence of BAP1 germline mutations in cutaneous melanocytic tumors with loss of BAP1-expression: a pilot study. Genes Chromosomes Cancer. 2017;56:691–4.
Soares De Sá BC, de Mecedo MP, Torrezan GT, Braga JCT, Fidalgo F, Moredo LF, et al. BAP1 tumor predisposition syndrome case report: Pathological and clinical aspects of BAP1-inactivated melanocytic tumors (BIMTs), including dermoscopy and confocal microscopy. BMC Cancer. 2019;19:1–8.
Shankar GM, Abedalthagafi M, Vaubel RA, Merrill PH, Nayyar A, Gill CM, et al. Germline and somatic BAP1 mutations in high-grade rhabdoid meningiomas. Neuro Oncol. 2017;19:535–45.
Jiao Y, Pawlik TM, Anders RA, Selaru FM, Streppel MM, Lucas DJ, et al. Exome sequencing identifies frequent inactivating mutations in BAP1, ARID1A and PBRM1 in intrahepatic cholangiocarcinomas. Nat Genet. 2013;45:1470–3.
Brandi G, Deserti M, Palloni, A, turchetti, D, Zuntini, R, Pedica, F et al. Intrahepatic cholangiocarcinoma development in a patient with a novel Bap1 germline mutation and low exposure to asbestos. Cancer Genet. 2020. https://doi.org/10.1016/j.cancergen.2020.10.001.
Shankar GM, Santagata S. BAP1 mutations in high-grade meningioma: implications for patient care. Neuro Oncol. 2017;19:1447–56.
O’Shea SJ, Robles-Espinoza CD, McLellan L, Harrigan J, Jacq X, Hewinson J, et al. A population-based analysis of germline BAP1 mutations in melanoma. Hum Mol Genet. 2017;26:717–28.
Turunen JA, Markkinen S, Wilska R, Saarinen S, Raivio V, Täll M, et al. BAP1 germline mutations in Finnish patients with uveal melanoma. Ophthalmology. 2016;123:1112–7.
Betti M, Casalone E, Ferrante D, Romanelli A, Grosso F, Guarrera S, et al. Inference on germline BAP1 mutations and asbestos exposure from the analysis of familial and sporadic mesothelioma in a high-risk area. Genes Chromosomes Cancer. 2015;54:51–62.
Wadt KAW, Aoude LG, Krogh L, sunde L, Bojesen A, Grønskov K, et al. Molecular characterization of melanoma cases in Denmark suspected of genetic predisposition. PLoS One. 2015;10:e0122662.
Repo P, Järvinen RS, Jäntii JE, Markkinen S, Täll M, Raivio V, et al. Population-based analysis of BAP1 germline variations in patients with uveal melanoma. Hum Mol Genet. 2019;28:2415–26.
Panou V, Gadiraju M, Wolin A, Weipert CM, Skarda E, Husain AN, et al. Frequency of germline mutations in cancer susceptibility genes in malignant mesothelioma. J Clin Oncol. 2018;36:2863–71.
Popova T, Herdert L, Jacquemin V, Gad S, Caux-Moncoutier V, Dubois-d’Enghien C, et al. Germline BAP1 mutations predispose to renal cell carcinomas. Am J Hum Genet. 2013;92:974–80.
Christensen MB, Wadt K, Jensen UB, Lautrup CK, Bojesen A, Krogh LN, et al. Exploring the hereditary background of renal cancer in Denmark. PLoS One. 2019;14:e0215725.
Carlo MI, Mukherjee S, Mandelker D, vijal J, Kemel Y, Zhang L, et al. Prevalence of germline mutations in cancer susceptibility genes in patients with advanced renal cell carcinoma. JAMA Oncol. 2018;4:1228–35.
Wu J, Wang H, Ricketts CJ, Yang Y, Merino MJ, Zhang H, et al. Germline mutations of renal cancer predisposition genes and clinical relevance in Chinese patients with sporadic, early-onset disease. Cancer. 2019;125:1060–9.
Maynard H, Stadler ZK, Berger MF, Solit DB, Ly M, Lowery MA, et al. Germline alterations in patients with biliary tract cancers: a spectrum of significant and previously underappreciated findings. Cancer 2020;126:1995–2002.
Shinozaki-Ushiku A, Kohsaka S, Kage H, Oda K, Miyagawa K, Nakajima J, et al. Genomic profiling of multiple primary cancers including synchronous lung adenocarcinoma and bilateral malignant mesotheliomas: Identification of a novel BAP1 germline variant. Pathol Int. 2020;70:775–80.
Carbone M, Harbour JW, Brugarolas J, Bononi A, Pagano I, Dey A, et al. Biological mechanisms and clinical significance of BAP1 mutations in human cancer. Cancer Discov. 2020;10:1103–20.
Laitman Y, Newberg J, Molho RB, Jin DX, Friedman E. The spectrum of tumors harboring BAP1 gene alterations. Cancer Genet. 2021;256–257:31–35.
Miller DT, Lee K, chung WK, Gordon AS, Herman GE, Klein TE, et al. ACMG SF v3.0 list for reporting of secondary findings in clinical exome and genome sequencing: a policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2021;23:1381–90.
Kuzbari Z, Bandlamundi C, Loveday C, Garrett A, Mehine M, George A, et al. Germline-focused analysis of tumour-detected variants in 49,264 cancer patients: ESMO Precision Medicine Working Group recommendations. Ann Oncol Off J Eur Soc Med Oncol. 2022. https://doi.org/10.1016/j.annonc.2022.12.003.
Richards S, aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Hassan R, Moroow B, Thomas A, Walsh T, Lee MK, Gulsuner S, et al. Inherited predisposition to malignant mesothelioma and overall survival following platinum chemotherapy. Proc Natl Acad Sci USA. 2019;116:9008–13.
Singh AD, Shields CL, Shields JA, De Potter P. Bilateral primary uveal melanoma. Bad luck or bad genes? Ophthalmology. 1996;103:256–62.
Nielsen M, Dogrusöz M, Bleeker JC, Kroes WG, van Asperen CA, Marinkovic M, et al. The genetic basis of uveal melanoma. J Fr Ophtalmol. 2015;38:516–21.
Singh N, Singh R, Bowen RC, Abdel-Rahman MH, Singh AD. Uveal melanoma in BAP1 tumor predisposition syndrome: estimation of risk. Am J Ophthalmol. 2020. https://doi.org/10.1016/j.ajo.2020.12.005
Young KZ, Fossum SL, Lowe L, Else T, Fecher LA, Demirci A, et al. An adolescent with uveal melanoma and BAP1 tumor predisposition syndrome. JAAD Case Rep. 2020;6:563–6.
Singh AD, De Potter P, Fijal BA, Shields CL, Shields JA, Elston RC. Lifetime prevalence of uveal melanoma in white patients with oculo(dermal) melanocytosis. Ophthalmology. 1998;105:195–8.
Cebulla CM, Binkley EM, Pilarski R, Massengill JB, Rai K, Liebner DA, et al. Analysis of BAP1 germline gene mutation in young uveal melanoma patients. Ophthalmic Genet. 2015;36:126–31.
Shields CL, Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009;127:989–98.
Hussain RN, Coupland SE, Kalirai H, Taktak AFG, Eleuteri A, damato BE, et al. Small high-risk uveal melanomas have a lower mortality rate. Cancers (Basel). 2021;13:2267.
Rigel DS, Friedman RJ, Kopf AW, Weltman R, Prioleau PG, safai B, et al. Importance of complete cutaneous examination for the detection of malignant melanoma. J Am Acad Dermatol. 1968;14:857–60.
Geller AC, Emmons KM, Brooks DR, Powers C, Zhang Z, Koh HK, et al. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107:806–14.
Titus LJ, Clough-Gorr K, Mackenzie TA, Perry A, Spencer SK, Weiss J, et al. Recent skin self-examination and doctor visits in relation to melanoma risk and tumour depth. Br J Dermatol. 2013;168:571–6.
Alpert N, van Gerwen M, Taioli E. Epidemiology of mesothelioma in the 21st century in Europe and the United States, 40 years after restricted/banned asbestos use. Transl Lung Cancer Res. 2020;9:S28–38.
Baumann F, Flores E, Napolitano A, Kanodia S, Taioli E, Pass H, et al. Mesothelioma patients with germline BAP1 mutations have 7-fold improved long-term survival. Carcinogenesis. 2015;36:76–81.
Carbone M, Pass HI, Ak G, Alexander HR Jr, Bass P, Baumann F, et al. Medical and surgical care of patients with mesothelioma and their relatives carrying germline BAP1 mutations. J Thorac Oncol. 2022;17:873–89.
Kapur P, Peña-Llopis S, Christie A, Zhrebker L, Pavía-Jiménez A, Rathmell WK, et al. Effects on survival of BAP1 and PBRM1 mutations in sporadic clear-cell renal-cell carcinoma: a retrospective analysis with independent validation. Lancet Oncol. 2013;14:159–67.
Ball MW, An JY, Gomella PT, Gautam R, Ricketts CJ, Vocke CD, et al. Growth rates of genetically defined renal tumors: implications for active surveillance and intervention. J Clin Oncol. 2020;38:1146–53.
van Oostenbrugge TJ, Fütterer JJ, Mulders PFA. Diagnostic imaging for solid renal tumors: a pictorial review. Kidney Cancer. 2018;2:79–93.
Acknowledgements
We would like to acknowledge Professor Clare Turnbull and Professor Diana Eccles for procurement of funding for this work as part of the CanGene-CanVar project. We would like to acknowledge the support of ERN GENTURIS in allowing us to approach their members to participate in the Delphi survey.
Funding
HH, FL, BT and MT are supported by Cancer Research CRUK Catalyst Award, CanGene-CanVar (C61296/A27223). MT was supported by the NIHR Cambridge Biomedical Research Centre (NIHR203312).
Author information
Authors and Affiliations
Consortia
Contributions
BAP1 Core group: FL, AK, CC, MN, MS, JS, RvD, KW MT and HH. Organisation and administration: BT and MH. Manuscript draft: HH and FL; Editing and review of manuscript; FL, AK, CC, MN, MS, JS, RvD, KW and MT, HH. Delphi survey: All listed authors. Final manuscript review: All listed authors
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lalloo, F., Kulkarni, A., Chau, C. et al. Clinical practice guidelines for the diagnosis and surveillance of BAP1 tumour predisposition syndrome. Eur J Hum Genet 31, 1261–1269 (2023). https://doi.org/10.1038/s41431-023-01448-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-023-01448-z
This article is cited by
-
Identification and validation of a costimulatory molecule-related signature to predict the prognosis for uveal melanoma patients
Scientific Reports (2024)
-
Deep phenotyping and population-level data can help resolve genomic variants
European Journal of Human Genetics (2023)