Abstract
Genetic services have historically been housed in tertiary care, requiring referral, which can present access barriers. While integrating genetics into primary care could facilitate access, many primary care physicians lack genomics expertise. Integrating genetic counsellors (GCs) into primary care could theoretically address these issues, but little is known about how to do this effectively. To understand and describe the process of integrating a GC into a multidisciplinary primary care setting, we qualitatively explored the perceptions, attitudes and reactions of existing team members prior to, and after the introduction of a GC. Semi-structured interviews were conducted immediately prior to (T1), and 9 months after (T2), the GC joining the clinic. Interviews were recorded, transcribed verbatim and analyzed concurrently with data collection using interpretive description. Twenty-four interviews were conducted with 17 participants (13 at T1, 11 at T2). Participants described several distinct, progressive stages of interaction with the GC: Disinterest or Resistance, Pre-Collaboration, Initial Collaboration, and Effective Collaboration/Integration of the GC into the team. At each stage, specific needs had to be met in order to advance to the next stage of collaboration. A variety of barriers and facilitators attended movement between different stages of the model. The Stepwise Process of Integration Model describes the process through which primary care staff and clinicians integrate a GC into their practice. The insight provided by this model could be used to facilitate more effective integration of GCs into other primary care settings.
Similar content being viewed by others
Introduction
With the rapid expansion of knowledge and technologies, genomic medicine is increasingly relevant across many areas of medicine. Further, the evidence base demonstrating that genetic counselling produces positive outcomes for people with common complex diseases is expanding [1,2,3]. Accordingly, pressure is mounting to incorporate genetics services more efficiently into clinical care.
Historically, genetics services have been largely siloed in tertiary care settings (typically large academic medical centres [4]). This results in geographic, financial and psychological barriers to access for large segments of the population [5], which can contribute to the disparities in health outcomes (e.g., urban vs. rural) [5], and as such, is an important ethical issue within both genetics and healthcare more broadly.
Theoretically, one of the best ways to more efficiently and equitably incorporate genetics into healthcare would be to create opportunities for patients to access genetic services in the context of primary care, which is associated with reduced patient costs and travel time [6, 7]. However, family doctors lack confidence in their competence to deliver genomic medicine [8,9,10,11,12]. Further, though the majority of primary care physicians agreed that advances in genomic medicine would improve patients’ health outcomes, most felt that incorporating genomic medicine was not their responsibility [8].
Increasingly, medicine is moving towards multidisciplinary teams as a model for the effective delivery of healthcare [13], and has been shown to improve patient outcomes for a variety of conditions [14,15,16,17]. Indeed, genetic counsellors (GCs) have successfully been integrated into oncology and cardiovascular clinic teams, where reported effects included: increases in the number of patients seen, decreased wait times and appointment length [18,19,20,21], better identification and triage of patients for genetic counselling and an increased referral rate for patients with syndromic features for a complete genetics consultation [19]. GCs also play an important role in utilization management through patient identification and triage [22, 23] and through reviewing genetic test requests [24,25,26,27], resulting in a reduction in inappropriate testing [25, 27]. All of this suggests that integrating GCs into primary care/family practice teams could create benefits both for patients and the healthcare system. Therefore, we set out to understand and describe the process of integrating a GC into a Canadian multidisciplinary primary care setting, by exploring the perceptions, Attitudes and reactions of existing team members prior to, and after the introduction of a GC into their team.
Methods
Context
As part of a larger study investigating the optimisation of genomic counselling in Canada (GenCOUNSEL), we conducted a qualitative (interpretive description) semi-structured interview-based study, for which we purposively recruited clinicians and staff from the primary care clinic (called the Cool Aid Community Health Centre, in Victoria, British Columbia) into which a GC was being embedded for a 1-year trial. Within the Canadian healthcare system, primary care is publicly funded and delivered through provincial health systems [28, 29]. Though the majority of primary care is provided through traditional physician clinic settings, a shift towards team-based care is underway [28]. The Cool Aid clinic is a unique, multidisciplinary clinic that serves ~7000 patients (age 19+) which includes a high proportion of people who are homeless or marginally housed, and people who use substances. Registered patients access physicians and nurses using “same day access” (booking day-of appointments), and other clinicians (e.g., counsellors, dieticians) by booking an appointment in advance or by clinician “referral” to another clinician (either by an in-person introduction, a real-time consult or a recommendation that the patient book an appointment with another clinician). The Cool Aid clinic was selected for the trial due to its unique patient population (typically underserved by genetics), and its culture, in which multidisciplinary collaboration is routine.
JA conducted two education sessions for staff and clinicians prior to the introduction of the GC. These sessions involved the provision of basic information about GCs’ training, skillset, and potential roles for a GC in a primary care setting (e.g. family history taking and review/triaging for referral for specialty genetics consults (e.g. cancer, cardio), genetic counselling for psychiatric disorders, etc). Based on this information, together with their knowledge of their clinical context and needs, the team decided that the GC’s role should largely be to provide psychiatric genetic counselling [1], as well as counselling and facilitating referrals for testing for genetic indications. Genetic counselling is not a regulated profession in Canada [30], but in this context, the counsellor was not ordering tests, or making diagnoses (i.e., was not performing any “regulated acts”), and carried their own liability insurance. The Research Ethics Board at BC Children’s and Women’s Hospital approved this study (H18-03333). Data from the GC’s experience will be analyzed and published separately.
Data collection
Semi-structured interviews were conducted just prior to (T1), and 9 months after (T2) the GC joining the clinic. A completed T1 interview was not required to participate at T2.
Participants were recruited from the selected clinic via study adverts that were circulated around the clinic space, announcements at team meetings, and email invitation by the clinic administrative coordinator. Interested individuals contacted the study team and provided written informed consent prior to the study interview. A combination of convenience, purposive and snowball recruitment was used to maximise the number of participants and range of participant positions. One-on-one semi-structured interviews were conducted remotely from participants’ workplace or homes via BlueJeans videoconference software, by a research GC (CS or EM [both MSc, female; trained in qualitative and quantitative methods with 5+ years of professional research experience, and no prior relationships with the participants/clinic]). Participants were informed of the interviewers’ background as a GC, and encouraged to share their perspectives openly. Interview guide development (see Supplementary Material) was informed by the Structuration Model of Collaboration, [31] which provides a framework with which to analyze interprofessional or interorganizational collaboration. Interviews comprised open-ended questions exploring participants’ perceptions of, experiences with, and opinions and attitudes around genetic counselling/collaborating with a GC. In one instance, an MSc genetic counselling student was present for observation purposes. As data collection and analysis progressed, interview guides were refined to ensure emerging areas of interest were captured in further interviews, and to ensure the interview guide for T2 was informed by the data collected at T1. Interviews were audio or video recorded per participant preference, transcribed verbatim and checked for accuracy before being analyzed. NVivo 12 [32] was used to store, organise and manage data.
Analysis
Interview data were analyzed concurrently with data collection using interpretive description [33, 34], an inductive qualitative approach that aims to understand the range of subjective human experiences to develop clinical understanding in an applied healthcare setting. The frames of reference for this study included the interviewers’ and broader study team’s genetic counselling background (specifically, belief in the unique value provided by genetic counselling and desire to increase access to genetic counselling in Canada) and the Structuration Model of Collaboration [31].
Analysis began with analyzing transcripts line by line for basic conceptual units and to delineate the properties that characterise them [34]. CS and EM independently coded the first three interviews, then came together to discuss codes and develop a coding framework, which CS then applied to remaining interviews. The coding framework was iteratively revised based on findings from new transcripts and applied to earlier interviews when relevant. Axial coding was then used to identify the main concepts from the coding framework, the conditions that give rise to them and the relationships between them. These concepts were used to inductively develop a model of the process of integrating a GC into the team—CS, EM and JA met on a regular basis to modify and verify the main concepts and to discuss the theoretical linkages between concepts, until the major concepts formed a cohesive theoretical model. Throughout the analysis process, written memos were used to capture decisions regarding the data and to record salient themes. Transcripts, codes and memos were iteratively reviewed to discuss and resolve discrepancies. Rather than aiming for “saturation” as a recruitment end point (which has been critiqued as a concept in qualitative research for a variety of reasons) [35], we employed the concept of theoretical sufficiency, which asks whether the model constructed is adequate in terms of the use for which it was envisioned [36]. We did not conduct any member checking due to Covid-19-related constraints.
Results
Participants
Twenty-four interviews were conducted with 17 participants over the two timepoints: 13 T1 (Oct 2019–Jan 2020); and 11 T2 interviews (Oct–Nov 2020). Seven participants completed interviews at both timepoints. Interviews averaged 33.5 min in length (range 11–54 min). Participants were between 34 and 64 years of age (median 46), had been practicing at the clinic between 11 months and 18 years (median 5), and most (13 of 17) identified as women. See Table 1 (and Supplementary Tables S1, S2).
Overview of the “Stepwise Process of Integration” Model
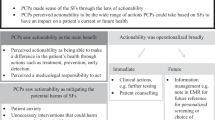
Participants described several distinct, progressive stages of interaction with the GC, as shown in Fig. 1. Advancement of the relationship and collaboration with the GC, and thus movement between stages was dependent on various participant needs being met, which were also influenced by numerous barriers and facilitators. See Table 2.
Staff and clinicians experience several distinct, progressive stages of interaction with the GC, ranging from disinterest or resistance, to effective collaboration and the perception that the GC is an integrated member of the team. Advancement of the relationship and collaboration with the GC, and thus movement between stages is dependent on various participant needs being met (Table 2). At each stage, barriers that could prevent these needs from being met, and facilitators that help the process advance are important. Foundational to the advancement of the relationship between the individual staff member/clinician and the GC is trust—the building of which occurs within the context of the specific clinic, which in turn influences the values and evidence required to further one’s trust with the GC and progress to a more advanced stage of collaboration. GC Genetic Counsellor. * The first step of integration occurs at the clinic management level: an initial need for clinic management to support the introduction of a GC into the clinic, and to discuss or plan how to adapt the genetic counselling skillset to the particular clinic needs. (In this case, the incoming GC was selected based on their expertise in psychiatric genetic counselling.) Once accepted at the clinic level, each individual clinician/staff enters the process of building collaboration with the GC. **Colour gradients indicate that each stage is not static/identical throughout. E.g., someone at the far-right side of “initial collaboration” would have more of a relationship and interaction with the GC than someone on the left side. *** Some individual clinicians/staff begin in the Pre-collaboration stage if their perception of genetic counselling already aligns with their personal values (see Table 2). **** Participants speculated that in the event of loss of trust with the GC, an individual clinician/staff may move backwards into earlier stages of collaboration. *****Based on participants’ experiences working with other HCPs, which they believed would also apply to their relationship with the GC.
Disinterest or resistance
This stage was characterised by participants’ protectiveness over their patients and an unwillingness to “expose” them to genetic counselling. This was associated with strong distrust and often, fear or negative perceptions of genetic counselling.
I have that apprehension because I don’t know what it is. And it’s like, I was talking about with my [child] this morning where we usually are scared of things we don’t understand.—Participant 1, T1
This fear was maintained as long as genetic counselling was seen as something “other” that could be at odds with participants’ own clinical goals and practice. Participants described wanting to “know the training of the GC” and that the genetic counselling profession as a whole engaged in patient-centred, values-aligned care.
Pre-collaboration
Once participants felt that the genetic counselling profession aligned with their personal or clinic values (see Table 2), they could move into the pre-collaboration stage. Participants who had prior positive experiences with or perceptions of genetic counselling, or a strong inherent trust in and value for other healthcare professionals (HCPs), began in the pre-collaboration stage (skipping the disinterest/resistance stage). In pre-collaboration, participants struggled to understand the genetic counselling role—particularly in primary care—but most described feeling “cautiously curious” and were willing to trial working with the GC.
I still don’t feel like I have like a great understanding of what that’s gonna look like but yeah, overall I feel very interested to hear kind of what they’ll offer and see how that will kind of benefit our patients I guess.—Participant 7, T1
Several participants, though also struggling to understand the GC’s role, were excited about the incoming GC and the idea of expanding the services available.
I think it’s going to be amazing… to have another person that can help people with the emotional side of things as well as understanding the nature of some of the medical concerns and issues that are genetic, I think would be really helpful. Yeah, I’m excited.—Participant 3, T1
At T1, most participants were in this pre-collaboration stage. Before moving on to initial collaboration, participants needed to confirm that the GC was a safe person for patients to interact with, and that the GC demonstrated certain clinic-specific values; in the context of this team, the most important of which was a trauma-informed approach.
We are very much focused on the fact that we are working with people who have experienced a lot of trauma… I think the person who comes in would need to tread very carefully and figure out how they’re going to react and respond and be with people in a way that is deeply respectful and, you know, really reflects the lived experience of the people that we’re working with.—Participant 10, T1
This issue was associated with varying degrees of hesitancy for different participants—no participants progressed beyond this stage at T1 (prior to meeting and interacting with the GC; see Supplementary Table S2). But, all bar one (who had minimal interaction with the GC) had moved beyond this stage by T2, at which point they described experiences with/attributes of the GC that facilitated the development of trust.
Yeah, I think [the GC] is both warm and calm, and non-judgmental… You know, part of our culture is very much patient-centred, trauma informed, equity based, and it did take a couple of conversations to say, you know… genetic counsellors are trained very much… to support, be patient-centred, to be trauma informed. And then she embodied it too when she came into the clinic, and I think that really helped.—Participant 4, T2
Initial collaboration
In initial collaboration, participants would refer at least a couple of patients to the GC, but a strong referral routine or relationship with the GC had yet to be established. At this point, significantly more barriers arose that impeded the transition to effective collaboration, particularly around the referral process; participants described discomfort with raising the option of genetic counselling to patients in some contexts.
So for example, sometimes people were coming in for a very simple [intervention]. There was no deep conversation happening… [so] it was completely out of context, and it kind of felt like here I am just bringing up all this really heavy, huge thing in the context of a really not-heavy visit… Like it felt like it was me knowing better than them. I didn’t feel like I was meeting the clients where they were at. That was the discomfort for me.—Participant 14, T2
Further, despite having a basic or theoretical understanding of genetic counselling, participants didn’t know what a genetic counselling encounter was like on a practical level, and struggled with how to introduce it to their patients.
I’m not as familiar with it still even though I’m kind of getting my head around like what [the GC] does and what she offers… I’m so much more familiar with what like a registered clinical counsellor would be doing versus the genetic counsellor.—Participant 7, T2
One participant described having negative perceptions of the genetic counselling encounter, which added to the discomfort of raising it as an option for patients.
I used to say lots of things to clients that would make most people uncomfortable, and I’m not bothered by it, but for some reason this just made me feel like I’m asking these people to talk about these really private things with somebody that they’ve never met. It just felt a bit intrusive…I did assume that [that genetic counselling would be scary or uncomfortable]. And maybe that’s my own bias… And maybe it would be uncomfortable for me, and that’s why I think that, I don’t know.—Participant 14, T2
Effective Collaboration/Integration into the team
Several participants progressed to the beginning of the effective collaboration stage, in which a routine had been established between the clinician and the GC with more regular referrals and two-way communication and follow-up. These participants all described a strong, stable sense of trust with the GC which had been developed and reinforced through their experience working together. The effective collaboration stage (like all stages) is not static—participants foresaw their relationship with the GC continuing to grow and develop with time and experience working together; or, if participants had not yet reached this stage, compared their relationship with the GC to relationships they had with other clinicians with whom they had been working for years, and with whom they had a deep working relationship.
When [one of the clinic nurses] tells me she’s worried, like, I get a chill, I freak, a cold sweat and I start to worry, freak out because if [this nurse] is worried, it’s serious. And how do I know that? Because we’ve been working together for 13 years, right. And I know what her thresholds are… None of us have that with a genetic counsellor. Even generically, generally with any genetic counsellor.—Participant 4, T1
In contrast to the initial collaboration stage, participants in the effective collaboration stage had a deeper understanding of genetic counselling that seemed to come from seeing it in practice; despite having had educational in-services and handouts about genetic counselling, participants described needing more “hands-on” or “tangible” education—suggesting that an intellectual understanding of genetic counselling is insufficient for effective collaboration.
[The GC] was patient, well at explaining her role…But then also practically, she would talk about [patients] that she had worked with [in the past] and gave some ways in which it was helpful to them, to sort of demonstrate the purpose of the work or the benefit of the work that she did. So that helped in a more tangible way to see.—Participant 5, T2
Participants in the effective collaboration stage also described having witnessed—either directly or from patient report—positive effects of genetic counselling on their patients, which also helped with understanding the purpose and role of genetic counselling in patient care. This was critical evidence that encouraged participants on to further collaboration with the GC and led them to endorse the value of having a GC available at the clinic.
[Patients] come to me in distress less. Yeah, I could definitely say that, that the people who have seen [the GC] for counselling regarding psychiatric conditions and the potential genetic links are somehow able to manage their own emotional distress a little better… and just following my patients leads. So if my patient said that [the GC] is great, I go with that… I think it’s great. I think we should have the position.—Participant 1, T2
Logistical barriers
In addition to stage-specific barriers to developing further collaboration with the GC, participants described several logistical difficulties that were not tied to a particular stage of collaboration and that could occur at any point for a particular participant; see Fig. 2; Table 3.
Discussion
This is the first study of which we are aware to explore the perceptions, attitudes and reactions of primary care staff and clinicians to the introduction of a GC into their team. The Stepwise Process of Integration describes the stages through which staff and clinicians progress in their interactions with a newly embedded GC, and the needs, facilitators and barriers that affect movement between stages.
GCs have been deployed in primary care systems in order to facilitate population genetic screening (e.g., Sanford Health Imagenetics program [37], MedCan), to provide genetic educational outreach services [6, 38], or genetic counselling through local outreach clinics [6, 7]; however, these GCs typically provide genetic services through external consultations as opposed to being fully embedded within a clinic. Existing literature reports on the outcomes of these service delivery models (e.g., patient experience [6, 7, 37], practitioner experience [38], genetic testing metrics [37]) and overall process [6, 7, 37, 38], but does not address the team integration process. In 2021, 2% of GCs reported working in a physician’s private practice and 1% provided private genetic consultations [39], but there are no reports on the process of, or requirements for, embedding GCs into primary care. Thus, there is little existing literature within the GC field with which to compare our findings. However, GCs working in private practice settings in Australia and New Zealand reported difficulty defining the boundaries of their role [40], and primary care practitioners in the UK were reported to be unsure of how they might utilize an outreach GC and needed guidance on what the GC could offer [38]; this was echoed by our participants’ need to really understand what the GC would do and to identify how the GC could help meet patient needs within the context of this particular clinic and patient population. Indeed, having defined, shared goals and roles are crucial for effective collaboration [31, 41,42,43]. This was a barrier for many of our participants, who required a more hands-on or practical understanding of genetic counselling, and evidence of the utility of genetic counselling for their patients, before they could understand who and why they should refer to the GC. This finding is reinforced by a study of Canadian nurses working in primary care, who reported that initially, their role in the clinic was vague—physicians “did not know what [the nurses] could do”—which resulted in lower utilization of nursing services [44]. However, over time and after “selling [themselves]” to demonstrate the value of nursing in primary care, nurses felt they had become important members of the team. This need to “pitch” or “advertise” one’s role is magnified when considering a lesser known, and commonly misunderstood profession like genetic counselling, and emphasises the need for contracting between HCPs to define the roles and goals of each team member. This was described by several participants who, once they heard of or witnessed positive impacts of genetic counselling for their patients and understood the goals or purpose of the GC, were keen to continue referring to the GC. Despite these participants identifying shared goals towards which they could work with the GC, others—especially those whose practices were focused on more immediate, acute opioid crisis care (see Box 2)—did not have a shared goal to work towards with the GC and therefore had much more limited collaboration with the GC.
Other aspects of the Stepwise Process of Integration—though novel in the context of genetic counselling—are robustly supported by existing work in other areas; in particular, our finding that trust and relationship-building were essential to progression through the various stages of integration is supported by the literature in primary care and other medical settings. Trust is a crucial component of an effective team [31, 41, 43], and is associated with better performance in interdisciplinary hospital settings [45]. A systematic review of teamwork and interprofessional collaboration in primary health care settings found that HCPs’ teamwork required trust, frequent communication and time together [43]. Similarly, a review of team-based primary care in Canada found that effective communication and trust must be built proactively to support effective team function; but that the significant time required to build relationships was a common barrier [42]. This was also evident among Canadian nurses who were integrated into primary care, who reported that with time and the development of mutual trust, team relationships improved and collaboration increased which resulted in better coordination of patient care [44]. Furthermore, the most critical piece of successful interprofessional collaboration that emerged from an integrative literature review was frequent, shared informal communication [46]. These elements—needing time and experience together, a need for trust and both intentional and casual relationship building—were frequently discussed by our participants at every stage of collaboration with increasing intensity. This was particularly salient at the transition from initial to effective integration, at which point a deeper level of trust and a developing relationship with the GC was required.
The Covid-19 pandemic presented a major barrier to participants achieving further collaboration with the GC. This resulted in numerous challenges to be overcome, including a lack of actual opportunity to interact and work with the GC and the disconnection between HCPs due to remote working arrangements. This is supported by a review of Canadian clinics in which sharing physical space was helpful for collaboration [42], and the study of Canadian nurses which found that decentralized models—in which team members were working in different locations—created a barrier to effective communication and teamwork [44]. Furthermore, Covid-19 caused major disruptions and shifts to the clinic structure, management and leadership priorities, all of which are crucial for effective teamwork [31, 41, 46] and which had a major impact on how participants experienced the integration of the GC.
Participants also experienced difficulty with referral processes, lack of time within their appointments with which to discuss genetic counselling, and difficulty accessing a geneticist when required. These barriers reflect the need for operational or procedural support that is needed for effective collaboration [31, 41], and demonstrates the need for significant attention to be paid to workflow issues when attempting the integration of a new specialty—particularly a lesser-known specialty—into a clinic’s processes.
Considerations for introducing a GC into a multidisciplinary or primary care setting
Participants expressed specific recommendations that could serve as facilitators of integration; see Table 4. Attention should be paid to the alignment between the clinical needs of the specific setting and the expertise of the GC to be integrated.
Limitations
Interview timepoints were selected due to practical issues caused by the Covid-19 global pandemic; interviews had initially been scheduled for three timepoints (before, during and after the 1-year trial), but this timeline was modified due to significant clinical and logistical strains introduced by the pandemic. Due to clinical challenges and pressures facing potential participants, we were unable to include the perspectives of all HCP positions at the clinic. It is possible that those who declined participation may have been resistant/disinterested in engaging with the GC.
Our model was developed from the experiences of a single clinic with a particular patient population, at a particular point in time. The Stepwise Process of Integration may not be generalizable to all clinical contexts; but it may be useful for establishing relationships with HCPs, particularly those who are less familiar with genetic counselling, who work with vulnerable patient groups, and/or who have less experience with team-based care.
Conclusions
Few GCs currently work in family practice, but growing pressure to expand and democratize access to genetic services is leading to increased use of varied genetic service delivery models [47, 48], including incorporation of genetic services into primary care.
The Stepwise Process of Integration Model describes the successive stages staff and clinicians experience when integrating a GC into their practice. Our findings of the needs, barriers and facilitators of these stages provide important guidance for future attempts at integrating GCs into primary care and healthcare more broadly.
Data availability
Data are available from the corresponding author on reasonable request.
Change history
07 March 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41431-022-01063-4
References
Austin JC. Evidence-Based Genetic Counseling for Psychiatric Disorders: A Road Map. Cold Spring Harb Perspect Med. 2020;10:a036608.
Ison HE, Ware SM, Schwantes-An T, Freeze S, Elmore L, Spoonamore KG. The impact of cardiovascular genetic counseling on patient empowerment. J Genet Counseling. 2019;28:570–7.
Madlensky L, Trepanier AM, Cragun D, Lerner B, Shannon KM, Zierhut H. A rapid systematic review of outcomes studies in genetic counseling. J Genet Counseling. 2017;26:361–78.
Battista RN, Blancquaert I, Laberge A-M, van Schendel N, Leduc N. Genetics in Health Care. Public health genomics. 2012;15:34–45. https://doi.org/10.1159/000328846.
Hawkins AK, Hayden MR. A grand challenge: Providing benefits of clinical genetics to those in need. Genet Med : Off J Am Coll Med Genet. 2011;13:197–200.
Westwood G, Pickering R, Latter S, Little P, Gerard K, Lucassen A, et al. A primary care specialist genetics service: a cluster-randomised factorial trial. Br J Gen Pract. 2012;62:e191–7. https://doi.org/10.3399/bjgp12X630089.
Westwood G. Feasibility and acceptability of providing nurse counsellor genetics clinics in primary care. 2006;8:129. https://doi.org/10.1111/j.1442-2018.2006.00272_17.x.
Carroll JC, Allanson J, Morrison S, Miller FA, Wilson BJ, Permaul JA, et al. Informing integration of genomic medicine into primary care: an assessment of current practice, attitudes, and desired resources. Front Genet. 2019;10:1189.
Haga SB, Carrig MM, O’Daniel JM, Orlando LA, Killeya-Jone LA, Ginsburg GS, et al. Genomic Risk Profiling: Attitudes and Use in Personal and Clinical Care of Primary Care Physicians Who Offer Risk Profiling 2011;26:834–40.
Shields AE, Burke W, Levy DE. Differential use of available genetic tests among primary care physicians in the United States: results of a national survey. Genet Med. 2008;10:404–14.
Suchard MA, Yudkin P, Sinsheimer JS, Fowler GH. General practitioners’ views on genetic screening for common diseases. Br J Gen Pract. 1999;49:45–6.
Freedman AN, Wideroff L, Olson L, Davis W, Klabunde C, Srinath KP, et al. US physicians’ attitudes toward genetic testing for cancer susceptibility. Am J Med Genet Part A. 2003;120A:63–71.
Leach B, Morgan P, Strand de Oliveira J, Hull S, Østbye T, Everett C. Primary care multidisciplinary teams in practice: a qualitative study. BMC Fam Pract. 2017;18:115.
Saint-Pierre C, Herskovic V, Sepúlveda M. Multidisciplinary collaboration in primary care: a systematic review. Fam Pract. 2018;35:132–41.
Chwastiak LA, Jackson SL, Russo J, DeKeyser P, Kiefer M, Belyeu B, et al. A collaborative care team to integrate behavioral health care and treatment of poorly-controlled type 2 diabetes in an urban safety net primary care clinic. Gen hospital psychiatry. 2016;44:10–5.
Jones SL. Diabetes case management in primary care: the New Brunswick experience and expanding the practice of the certified diabetes educator nurse into primary care. Can J Diabetes. 2015;39:322–4.
Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525.
Kentwell M, Dow E, Antill Y, Wrede CD, McNally O, Higgs E, et al. Mainstreaming cancer genetics: A model integrating germline BRCA testing into routine ovarian cancer clinics. Gynecologic Oncol. 2017;145:130–6.
Helm BM, Freeze SL, Spoonamore KG, Ware SM, Ayers MD, Kean AC. The Genetic Counselor in the Pediatric Arrhythmia Clinic: Review and Assessment of Services. J Genet Counseling. 2018;27:558–64.
Senter L, O’Malley DM, Backes FJ, Copeland LJ, Fowler JM, Salani R, et al. Genetic consultation embedded in a gynecologic oncology clinic improves compliance with guideline-based care. Gynecologic Oncol. 2017;147:110–4.
Tan R, Met-Domestici M, Zhou K, Guzman A, Thye Lim S, Chee et al. Using Quality Improvement Methods and Time-Driven Activity Based Costing to Improve Value-Based Cancer Care Delivery at a Cancer Genetics Clinic. 2016;12:e320-31.
Kubendran S, Sivamurthy S, Schaefer GB. A novel approach in pediatric telegenetic services: Geneticist, pediatrician and genetic counselor team. Genet Med. 2017;19:1260–7.
Eichmeyer JN, Burnham C, Sproat P, Tivis R, Beck TM. The Value of a Genetic Counselor: Improving Identification of Cancer Genetic Counseling Patients with Chart Review. J Genet Counseling. 2014;23:323–9.
Suarez CJ, Yu L, Downs N, Costa HA, Stevenson DA. Promoting appropriate genetic testing: the impact of a combined test review and consultative service. Genet Med. 2017;19:1049–54.
Miller CE, Krautscheid P, Baldwin EE, Tvrdik T, Openshaw AS, Hart K, et al. Genetic counselor review of genetic test orders in a reference laboratory reduces unnecessary testing. Am J Med Genet A. 2014:1094–101.
Dickerson JA, Cole B, Conta JH, Wellner M, Wallace SE, Jack RM, et al. Improving the value of costly genetic reference laboratory testing with active utilization management. Arch Pathol Lab Med. 2014;138:110–3.
Wakefield E, Keller H, Mianzo H, Nagaraj CB, Tawde S, Ulm E. Reduction of Health Care Costs and Improved Appropriateness of Incoming Test Orders: the Impact of Genetic Counselor Review in an Academic Genetic Testing. Laboratory. 2018;27:1067–73.
Government of Canada. About Primary Health Care 2012. https://www.canada.ca/en/health-canada/services/primary-health-care/about-primary-health-care.html. Accessed 4 Nov 2021.
Ormond KE, Laurino MY, Barlow‐stewart K, Wessels T, Macaulay S, Austin J, et al. Genetic counseling globally: Where are we now? Am J Med Genet Part C Semin Med Genet. 2018;178:98–107. https://doi.org/10.1002/ajmg.c.31607.
Lambert DM, Patrinos D, Knoppers BM, Zawati MH. Genetic counselors and legal recognition: A made‐for‐Canada approach, J Genet Counseling. 2021. https://doi.org/10.1002/jgc4.1468.
D’Amour D, Goulet L, Labadie J-F, Martín-Rodriguez LS, Pineault R. A model and typology of collaboration between professionals in healthcare organizations. BMC Health Serv Res. 2008;8:188.
QSR International Pty Ltd. NVivo (Version 12). https://Www.Qsrinternational.Com/Nvivo-Qualitative-Data-Analysis-Software/Home: 2018.
Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive Description: A Noncategorical Qualitative Alternative for Developing Nursing Knowledge. Res Nurs health. 1997;20:169–77.
Thorne S, Kirkham SR, O’Flynn-Magee K. The Analytic Challenge in Interpretive Description. Int. J Qual Meth. 2004;3:1–11. https://doi.org/10.1177/160940690400300101.
Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol. 2018;18:148. https://doi.org/10.1186/s12874-018-0594-7.
Dey I. Grounding grounded theory: Guidelines for qualitative inquiry. San Diego: Academic Press; 1999.
Christensen KD, Bell M, Zawatsky CLB, Galbraith LN, Green RC, Hutchinson AM, et al. Precision population medicine in primary care: the Sanford Chip experience. Front. Genet. 2021. https://doi.org/10.3389/fgene.2021.626845.
Drury N, Bethea J, Guilbert P, Qureshi N. Genetics Support to Primary Care Practitioners—A Demonstration Project. J Genet Counseling. 2007;16:583–91. https://doi.org/10.1007/s10897-007-9096-1.
National Society of Genetic Counselors. 2021 Professional Status Survey: Work Environment. 2021. https://www.nsgc.org/Policy-Research-and-Publications/Professional-Status-Survey. Retrieved Jan 25, 2022.
Collis S, Gaff C, Wake S, McEwen A. Genetic Counsellors and Private Practice: Professional Turbulence and Common Values. J Genet Couns. 2018;27:782–91.
Levesque J-F, Harris MF, Scott C, Crabtree B, Miller W, Halma LM, et al. Dimensions and intensity of inter-professional teamwork in primary care: evidence from five international jurisdictions. Fam Pract. 2018;35:285–94.
Fletcher SC, Bellwood P, Hill TT, Martin S, Ashe MC, Price M. A review and synthesis of TBPCC evaluation in Canada: Looking beyond the quadruple aim. Under Review. https://doi.org/10.21203/rs.2.18076/v1.
Sangaleti C, Schveitzer MC, Peduzzi M, Zoboli ELCP, Soares CB. Experiences and shared meaning of teamwork and interprofessional collaboration among health care professionals in primary health care settings: a systematic review. JBI Database Syst Rev Implement Rep. 2017;15:2723–88.
Al Sayah F, Szafran O, Robertson S, Bell NR, Williams B. Nursing perspectives on factors influencing interdisciplinary teamwork in the Canadian primary care setting. J Clin Nurs. 2014;23:2968–79.
Sifaki-Pistolla D, Melidoniotis E, Dey N, Chatzea V-E. How trust affects performance of interprofessional health-care teams. J Interprof Care. 2020;34:218–24.
Morgan S, Pullon S, McKinlay E. Observation of interprofessional collaborative practice in primary care teams: an integrative literature review. Int J Nurs Stud. 2015;52:1217–30.
Stoll K, Kubendran S, Cohen SA. The past, present and future of service delivery in genetic counseling: Keeping up in the era of precision medicine. Am J Med Genet Part C, Semin Med Genet. 2018;178:24–37.
Unim B, De Vito C, Hagan J, Villari P, Knoppers BM, Zawati M. The provision of genetic testing and related services in Quebec. Canada. 2020;11:127.
Acknowledgements
The authors would like to thank Patricia Birch for her assistance with ethics approval. The GenCOUNSEL Study is led by AME, JA, Bartha Maria Knoppers, and Larry D. Lynd with Project Manager Alivia Dey, and includes the following co-investigators: Shelin Adam, Nick Bansback, Patricia Birch, Lorne Clarke, Nick Dragojlovic, Jan Friedman, Deborah Lambert, Daryl Pullman, Alice Virani, Wyeth Wasserman, and Ma’n H. Zawati. JA was supported by the Canada Research Chairs program and BC Mental Health and Substance Use services. The authors offer gratitude to the Coast Salish Peoples, including the xʷməθkwəy̓əm (Musqueam), Skwxwú7mesh (Squamish), Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh), lək̓ʷəŋən (Lekwungen)—Esquimalt and Songhees Nations, on whose traditional, unceded and ancestral territory we have the privilege of working.
Funding
GenCOUNSEL was funded through the Large Scale Applied Research Project (LSARP) Genome Canada competition with co-funding from: Canadian Institute for Health Research (CIHR), Genome BC, Genome Québec, Provincial Health Services Authority, BC Children’s Hospital Foundation and BC Women’s Hospital Foundation.
Author information
Authors and Affiliations
Consortia
Contributions
CS was responsible for developing study protocols, recruitment, data collection, data analysis, development of the theoretical model, and writing the manuscript. EM was responsible for study recruitment, data collection, data analysis, development of the theoretical model and critical review of the manuscript. MP was responsible for study design and critical review of the manuscript. AME was responsible for study design, modifications to the theoretical model and critical review of the manuscript. JA was responsible for study design, development of the theoretical model, and critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
MP works as a physician at the Cool Aid Community Health Centre.
Ethical approval
This study received harmonised ethical approval from the BC Children’s and Women’s Research Ethics Board (H18-03333) and Island Health (VIHA).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Slomp, C., Morris, E., GenCOUNSEL Study. et al. The stepwise process of integrating a genetic counsellor into primary care. Eur J Hum Genet 30, 772–781 (2022). https://doi.org/10.1038/s41431-022-01040-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-022-01040-x
This article is cited by
-
A collaborative model for Medical Genetics services delivery in Portugal: a multidisciplinary perspective
Journal of Community Genetics (2024)
-
The urgency for a change in genetics healthcare provision: views from Portuguese medical geneticists
Journal of Community Genetics (2024)
-
2022: the year that was in the European Journal of Human Genetics
European Journal of Human Genetics (2023)
-
A qualitative exploration of interprofessional collaborative practice between genetic counselors and mental health providers
Journal of Community Genetics (2023)
-
Clinical genomics testing: mainstreaming and globalising
European Journal of Human Genetics (2022)