Abstract
Background/Objectives
Resting energy expenditure (REE) constitutes the largest component of total energy expenditure and undergoes an age-related decline that is unexplained by decreased fat-free mass. Phase angle (PhA) is a cellular health indicator that is possibly associated with REE. We investigated the association of REE and PhA in hospitalized older adults.
Subjects/Methods
This single-center, cross-sectional analysis utilized the baseline data from a prospective longitudinal study and included 131 eligible patients aged ≥70 years. The REE was measured using indirect calorimetry, and PhA and body composition were assessed using bioelectrical impedance. The association between REE, PhA, and body composition was examined, and REE was compared using previously reported PhA cutoff values.
Results
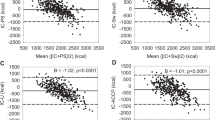
In this cohort with a mean (±standard deviation) age of 87.4 (±7.0) years, 34.4% of the participants were men. REE and PhA correlated strongly (r: 0.562, p < 0.001) and significantly after adjusting for age and sex (r: 0.433, p < 0.001). Multivariate analysis showed a significant independent association between REE and PhA and skeletal muscle mass (standardized β [95% CI]; 28.072 [2.188–53.956], p = 0.035) without any significant interaction between PhA and age on REE. The low PhA group had a significantly lower REE (kcal/day; 890 [856–925] vs. 1077 [1033–1122], p < 0.001), and this remained significant after adjusting for age, sex, and skeletal muscle mass index.
Conclusions
PhA is associated with REE in older adults. Adjusting REE calculation algorithms based on PhA values and correcting predicted REE according to PhA may aid in determining more accurate energy requirements.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to privacy reasons and ethical restrictions related to patient data but are available from the corresponding author upon reasonable request.
References
Kyu HH, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–922.
Maeda K, Ishida Y, Nonogaki T, Mori N. Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr. 2020;39:180–4.
Leij-Halfwerk S, Verwijs MH, van Houdt S, Borkent JW, Guaitoli PR, Pelgrim T, et al. Prevalence of protein-energy malnutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults ≥65 years: a systematic review and meta-analysis. Maturitas. 2019;126:80–9.
Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet. 2019;393:2312–21.
Bendavid I, Lobo DN, Barazzoni R, Cederholm T, Coëffier M, De Van Der Schueren M, et al. The centenary of the Harris–Benedict equations: How to assess energy requirements best? Recommendations from the ESPEN expert group. Clinical Nutrition. 2021;40:690–701.
Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care. 2016;20:367.
Omura T, Tamura Y, Yamaoka T, Yoshimura Y, Sakurai T, Umegaki H, et al. Assessing the association between optimal energy intake and all‐cause mortality in older patients with diabetes mellitus using the Japanese Elderly Diabetes Intervention Trial. Geriatr Gerontol Int. 2020;20:59–65.
Soares MJ, Müller MJ. Resting energy expenditure and body composition: critical aspects for clinical nutrition. Eur J Clin Nutr. 2018;72:1208–14.
Achamrah N, Delsoglio M, De Waele E, Berger MM, Pichard C. Indirect calorimetry: the 6 main issues. Clin Nutr. 2021;40:4–14.
Pontzer H, Yamada Y, Sagayama H, Ainslie PN, Andersen LF, Anderson LJ, et al. Daily energy expenditure through the human life course. Science. 2021;373:808–12.
Manini TM. Energy expenditure and aging. Ageing Res Rev. 2010;9:1–11.
Ward LC, Brantlov S. Bioimpedance basics and phase angle fundamentals. Rev Endocr Metab Disord. 2023;24:381–91.
Norman K, Stobäus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin Nutr. 2012;31:854–61.
Slee A, Birc D, Stokoe D. Bioelectrical impedance vector analysis, phase-angle assessment and relationship with malnutrition risk in a cohort of frail older hospital patients in the United Kingdom. Nutrition. 2015;31:132–7.
Yamada Y, Yoshida T, Murakami H, Kawakami R, Gando Y, Ohno H. et al. Phase angle obtained via bioelectrical impedance analysis and objectively measured physical activity or exercise habits. Sci Rep. 2022;12:17274.
Norman K, Herpich C, Müller-Werdan U. Role of phase angle in older adults with focus on the geriatric syndromes sarcopenia and frailty. Rev Endocr Metab Disord. 2023;24:429–37.
Martins PC, Alves Junior CAS, Silva AM, Silva DAS. Phase angle and body composition: a scoping review. Clin Nutr ESPEN. 2023;56:237–50.
Garlini LM, Alves FD, Ceretta LB, Perry IS, Souza GC, Clausell NO. Phase angle and mortality: a systematic review. Eur J Clin Nutr. 2019;73:495–508.
Marra M, Di Vincenzo O, Cioffi I, Sammarco R, Morlino D, Scalfi L. Resting energy expenditure in elite athletes: development of new predictive equations based on anthropometric variables and bioelectrical impedance analysis derived phase angle. J Int Soc Sports Nutr. 2021;18:68.
Marra M, Cioffi I, Sammarco R, Santarpia L, Contaldo F, Scalfi L, et al. Are raw BIA variables useful for predicting resting energy expenditure in adults with obesity? Nutrients. 2019;11:216.
Marra M, Sammarco R, Cioffi I, Morlino D, Di Vincenzo O, Speranza E, et al. New predictive equations for estimating resting energy expenditure in subjects with normal weight and overweight. Nutrition. 2021;84:111105.
Kojima G, Iliffe S, Taniguchi Y, Shimada H, Rakugi H, Walters K. Prevalence of frailty in Japan: a systematic review and meta-analysis. J Epidemiol. 2017;27:347–53.
Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56:M366–72.
Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67:254–66.
Yamada M, Kimura Y, Ishiyama D, Nishio N, Otobe Y, Tanaka T, et al. Phase angle is a useful indicator for muscle function in older adults. J Nutr Health Aging. 2019;23:251–5.
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300–7.e2.
Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69–71.
Iacobucci D, Schneider MJ, Popovich DL, Bakamitsos GA. Mean centering, multicollinearity, and moderators in multiple regression: the reconciliation redux. Behav Res Methods. 2017;49:403–4.
R Core Team. R: A Language and Environment for Etatistical Computing. Vienna, Austria: R Foundation for Statistical Computing. 2023. https://R-project.org/.
Austin PC, Steyerberg EW. The number of subjects per variable required in linear regression analyses. J Clin Epidemiol. 2015;68:627–36.
Harrell FE Jr., Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87.
Marra M, Cioffi I, Morlino D, Vincenzo OD, Pagano MC, Imperatore N, et al. New predictive equations for estimating resting energy expenditure in adults with Crohn’s disease. J Parenter Enteral Nutr. 2020;44:1021–8.
Müller MJ, Geisler C, Hübers M, Pourhassan M, Braun W, Bosy-Westphal A. Normalizing resting energy expenditure across the life course in humans: challenges and hopes. Eur J Clin Nutr. 2018;72:628–37.
Neelemaat F, van Bokhorst-de van der Schueren MA, Thijs A, Seidell JC, Weijs PJ. Resting energy expenditure in malnourished older patients at hospital admission and three months after discharge: predictive equations versus measurements. Clin Nutr. 2012;31:958–66.
Kawase F, Masaki Y, Ozawa H, Imanaka M, Sugiyama A, Wada H, et al. Resting energy expenditure in older inpatients: a comparison of prediction equations and measurements. Nutrients. 2022;14:5210.
Itoi A, Yamada Y, Yokoyama K, Adachi T, Kimura M. Validity of predictive equations for resting metabolic rate in healthy older adults. Clin Nutr ESPEN. 2017;22:64–70.
Visser M, van Venrooij LM, Wanders DC, de Vos R, Wisselink W, van Leeuwen PA, et al. The bioelectrical impedance phase angle as an indicator of undernutrition and adverse clinical outcome in cardiac surgical patients. Clin Nutr. 2012;31:981–6.
Lahaye C, Derumeaux-Burel H, Guillet C, Pereira B, Boirie Y. Determinants of resting energy expenditure in very old nursing home residents. J Nutr Health Aging. 2022;26:872–8.
Pourhassan M, Daubert D, Wirth R. Measured and predicted resting energy expenditure in malnourished older hospitalized patients: a cross-sectional and longitudinal comparison. Nutrients. 2020;12:2240.
Del Giorno R, Quarenghi M, Stefanelli K, Rigamonti A, Stanglini C, De Vecchi V, et al. Phase angle is associated with length of hospital stay, readmissions, mortality, and falls in patients hospitalized in internal-medicine wards: a retrospective cohort study. Nutrition. 2021;85:111068.
Genton L, Herrmann FR, Spörri A, Graf CE. Association of mortality and phase angle measured by different bioelectrical impedance analysis (BIA) devices. Clin Nutr. 2018;37:1066–9.
Acknowledgements
We would like to thank the medical staff at Asuke Hospital for their support and assistance with data collection. We would also like to thank Editage (http://www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Contributions
Conceptualization: FK, YM, HO, MI, AS, HW, SK, and TT; Data curation: FK, HO, HW, MI, and AS; Formal analysis: FK; Investigation: FK, HO, HW, MI, AS, and HW; Methodology: FK, YM, and TT; Project administration: FK, YM, SK, and TT; Roles/Writing—original draft: FK; Writing—review and editing: FK, YM, HO, MI, AS, HW, SK, and TT. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kawase, F., Masaki, Y., Ozawa, H. et al. Association of resting energy expenditure with phase angle in hospitalized older patients: a cross-sectional analysis. Eur J Clin Nutr 78, 187–192 (2024). https://doi.org/10.1038/s41430-023-01370-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01370-z