Abstract
Background
The persistent high prevalence of anaemia among Indian women of reproductive age (WRA) despite aggressive long-term iron supplementation could be related to over-diagnosis from an inappropriately high haemoglobin (Hb) diagnostic cut-off. To develop an appropriate cut-off for Indian WRA, we hypothesized that during iron-folic acid (IFA) supplementation to a mixed (anaemic/non-anaemic) WRA population, the positive slope of the Hb-plasma ferritin (PF) response in anaemic women would inflect into a plateau (zero-response) as a non-anaemic status is reached. The 2.5th percentile of the Hb distribution at this inflection point will be the diagnostic Hb cut-off for iron-responsive anaemia.
Method
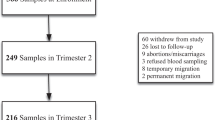
A hierarchical mixed effects model, with a polynomial mean and variance model to account for intraclass correlation due to repeated measures, was used to estimate the response curve of Hb to PF, or body iron stores, in anaemic and non-anaemic WRA (without inflammation), who were receiving a 90-day IFA supplementation.
Results
The Hb response curve at low PF values showed a steep increase, which inflected into a plateau at a PF of 10.1 µg/L and attained a steady state at a PF of 20.6 µg/L. The Hb distribution at the inflection was a normal probability distribution, with a mean of 12.3 g/dL. The 2.5th percentile value of this distribution, or the putative diagnostic Hb cut-off for anaemia, was 10.8 g/dL (~11 g/dL).
Conclusion
The derived Hb cut-off is lower than the current adult values of 12 g/dL and could partly explain the persistently high prevalence of anaemia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
International Institute for Population Sciences (IIPS). National Family Health Survey (NFHS-5), 20119-20: fact sheets: Key Indicators 22 States/UTs from phase I; 2020. http://rchiips.org/nfhs/factsheet_NFHS-5.shtml.
Ministry of Health and Family Welfare (MoHFW), Government of India, Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi. 2019. https://nhm.gov.in/WriteReadData/l892s/1405796031571201348.pdf.
Pasricha SR, Armitage AE, Prentice AM, Drakesmith H. Reducing anaemia in low income countries: control of infection is essential. BMJ 2018;362:k3165.
Kulkarni B, Peter R, Ghosh S, Pullakhandam R, Thomas T, Reddy GB, et al. Prevalence of Iron Deficiency and its Sociodemographic Patterning in Indian Children and Adolescents: Findings from the Comprehensive National Nutrition Survey 2016-18. J Nutr. 2021;151:2422–34.
Nair K, Dripta R, Konapur A. Appropriate doses of iron for treatment of anemia amongst. Indian J Community Health 2018;30:39–53.
Neufeld LM, Larson LM, Kurpad A, Mburu S, Martorell R, Brown KH. Hemoglobin concentration and anemia diagnosis in venous and capillary blood: biological basis and policy implications. Ann N. Y Acad Sci. 2019;1450:172–89.
World Health Organization. Regional Office for Europe & United Nations Children’s Fund (UNICEF). (2001). Prevention and control of iron-deficiency anaemia in women and children : report of the UNICEF/WHO regional consultation, Geneva, Switzerland 3-5 February 1999. Copenhagen: WHO Regional Office for Europe. https://apps.who.int/iris/handle/10665/108513.
WHO. Hemoglobin concentrations for the diagnosis of anemia and assessment of severity (WHO/NMH/NHD/MNM/11.1). 2011. https://apps.who.int/iris/handle/10665/85839 (accessed 13 March 2023).
Garcia-Casal MN, Pasricha S-R, Sharma AJ, Peña-Rosas JP. Use and interpretation of hemoglobin concentrations for assessing anemia status in individuals and populations: results from a WHO technical meeting. Ann N. Y Acad Sci. 2019;1450:5.
Sachdev HS, Porwal A, Acharya R, Ashraf S, Ramesh S, Khan N, et al. Haemoglobin thresholds to define anaemia in a national sample of healthy children and adolescents aged 1-19 years in India: a population-based study. Lancet. Glob Health. 2021;9:e822–e31.
Sarna A, Porwal A, Ramesh S, Agrawal PK, Acharya R, Johnston R, et al. Characterisation of the types of anaemia prevalent among children and adolescents aged 1–19 years in India: a population-based study. Lancet Child Adolesc Health. 2020;4:515–25.
Gupta A, Kant S, Ramakrishnan L, Pandey RM, Khandelwal R, Kapil U, et al. Impact of daily-supervised administration of a package of iron and folic acid and vitamin B12 on hemoglobin levels among adolescent girls (12-19 years): a cluster randomized control trial. Eur J ClinNutr. 2021;75:1588–97.
Gera T, Sachdev H, Nestel P. Effect of combining multiple micronutrients with iron supplementation on Hb response in children: Systematic review of randomized controlled trials. Public Health Nutr. 2009;12:756–73.
Palika R, Dasi T, Ghosh S, Peter R, Parasannanavar DJ, Pradhan AS, et al. Efficacy of iron-folic acid treatment for reducing anemia prevalence and improving iron status in women of reproductive age: A one-year longitudinal study. ClinNutr ESPEN. 2022;49:390–7.
Kulkarni B, Augustine LF, Pullakhandam R, Pradhan AS, Dasi T, Palika R, et al. ‘Screen and Treat for Anaemia Reduction (STAR)’ strategy: study protocol of a cluster randomised trial in rural Telangana, India. BMJ Open. 2021;11:e052238.
MOHFW. Intensified National Iron Plus Initiative, Anaemia Mukt Bharat Operational Guidelines. Government of India; 2018. https://www.fitterfly.com/site/pdf/anemia-mukt-bharat.pdf.
Dasi T, Palika R, Pullakhandam R, Augustine LF, Boiroju NK, Prasannanavar DJ. et al. Point-of-care Hb measurement in pooled capillary blood by a portable autoanalyser: Comparison with venous blood Hb measured by reference methods in cross-sectional and longitudinal studies. Br J Nutr. 2022;128:1108–17.
Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood 2003;101:3359–64.
Mercade L, Metzger M, Haymann JP, Thervet E, Boffa J-J, Martin Flamant. et al. The Relation of Hepcidin to Iron Disorders, Inflammation and Hemoglobin in Chronic Kidney Disease. PLoS ONE. 2014;9:e99781.
Varghese JS, Thomas T, Kurpad AV. Evaluation of haemoglobin cut-off for mild anaemia in Asians - analysis of multiple rounds of two national nutrition surveys. Indian J Med Res. 2019;150:385–9.
Müller SM, Dawczynski C, Wiest J, Lorkowski S, Kipp AP, Schwerdtle T. Functional Biomarkers for the Selenium Status in a Human Nutritional Intervention Study. Nutrients 2020;12:676.
Reddi AS. Riboflavin nutritional status and flavoprotein enzymes in streptozotocin- diabetic rats. BiochimBiophysActa. 1986;882:71–76.
Gera T, Sachdev HP, Nestel P, Sachdev SS. Effect of iron supplementation on haemoglobin response in children: systematic review of randomised controlled trials. J PediatrGastroenterolNutr. 2007;44:468–86.
Addo OY, Yu EX, Williams AM, Melissa FY, Andrea JS, Zuguo M, et al. Evaluation of hemoglobin cutoff levels to define anemia among healthy individuals. JAMA Netw Open. 2021;4:e2119123.
Ohuma EO, Young MF, Martorell R, Ismail LC, Peña-Rosas JP, Purwar M, et al. International values for haemoglobin distributions in healthy pregnant women. EClinical Med 2020;29e30:100660.
Sezgin G, Monagle P, Loh TP, Ignjatovic V, Hoq M, Pearce C, et al. Clinical thresholds for diagnosing iron deficiency: comparison of functional assessment of serum ferritin to population based centiles. Sci Rep. 2020;10:18233.
Funding
This secondary analysis was not funded. The human data came from a study that was funded by the Indian Council of Medical Research (ICMR), Government of India to BK, in turn nested in a larger study supported by a grant from the Systems Biology Research Initiative from the International Crops Research Institute for the Semi-Arid Tropics (ICRISAT) to RKV. The ICRISAT funding contributed to some activities related to data collection in the present study.
Author information
Authors and Affiliations
Contributions
SG and AVK wrote the first draft of the paper. All authors commented and edited draft versions and then approved the final version of the paper. SG, HSS, AVK and BK had primary responsibility for final content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
No separate ethical approval was required for this secondary analysis. The original study was nested within a trial (CTRI No: 2019/02/017806, http://ctri.nic.in/) to evaluate the effect of IFA supplementation on the gut microbiome and Hb. The original study was approved by the ethics committee of ICMR-National Institute of Nutrition (IEC: 06/II/2018). Prior informed consent from the participants and approval of the college authorities was taken for the study participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghosh, S., Palika, R., Dasi, T. et al. Haemoglobin diagnostic cut-offs for anaemia in Indian women of reproductive age. Eur J Clin Nutr 77, 966–971 (2023). https://doi.org/10.1038/s41430-023-01308-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01308-5