Abstract
Celiac Disease (CD) continues to require a strict lifetime gluten-free diet (GFD) to maintain healthy status. Many studies have assessed the GFD nutritional adequacy in their cohorts, but an overall picture in adults and children would offer a lifetime vision to identify actionable areas of change. We aimed at assessing the nutrient intakes of adult and pediatric CD patients following a GFD diet and identifying potential areas of improvement. Systematic review was carried out across PubMed, Scopus and Scholar up to October 2022, including full-text studies that assessed the nutrient intakes of CD patients on GFD, in terms of macro- and/or micronutrients (absolute or percentage daily average). Random-effect meta-analysis and univariable meta-regression were applied to obtain pooled estimates for proportions and influencing variables on the outcome, respectively. Thirty-eight studies with a total of 2114 patients were included. Overall, the daily energy intake was 1995 (CI 1884–2106) Kcal with 47.8% (CI 45.7–49.8%) from carbohydrates, 15.5% (CI 14.8–16.2%) from proteins, and 35.8% (CI 34.5–37.0%) from fats. Of total fats, 13.2% (CI 12.4–14.0%) were saturated fats. Teenagers had the highest consumption of fats (94.9, CI 54.8–134.9 g/day), and adults presented insufficient dietary fiber intake (18.9 g, CI 16.5–21.4 g). Calcium, magnesium, and iron intakes were particularly insufficient in adolescence, whereas vitamin D was insufficient in all age groups. In conclusion, GFD may expose CD patients to high fat and low essential micronutrient intakes. Given GFD is a lifelong therapy, to prevent the occurrence of diseases (e.g. cardiovascular or bone disorders) dietary intakes need to be assessed on long-term follow-ups.
Similar content being viewed by others
Introduction
Coeliac disease (CD) is an autoimmune condition that entails chronic enteropathy and affects ~1% of the general population [1]. It is triggered by the ingestion of gluten in genetically predisposed individuals, and it is characterized by specific serological and histological findings [1]. Currently, the only effective therapy available is strict lifetime adherence to a gluten-free diet (GFD), which leads to the remission of symptoms and to the normalization of serological and histological patterns in most patients [1].
Due to the prevalence of CD and to the recent identification and mass-media spreading of the non-coeliac gluten sensitivity condition, which has been self-reported by up to 13% of the population [2], a significant proportion of people in industrialized countries are currently consuming GFDs. However, GFD can be nutritionally incomplete if education steps are not taken. Numerous studies have tried to assess the dietary intakes of CD patients on GFD and have found mixed results [3,4,5,6,7]. Some studies blamed GFD to be unbalanced, leaning toward high-fat intake, especially of saturated fats [8, 9]. This aspect might increase cardiovascular risk throughout patients’ life [10]. This is especially true for pediatric patients who may start GFD at a very early age.
Data on GFD dietary assessments mostly come from single-center studies reflecting the local habits. A worldwide picture would be helpful to verify whether the GFD is appropriate and to identify potential areas of improvement for the patient’s health and wellbeing. Therefore, the primary aim of this systematic review and meta-analysis was to comprehensively assess the absolute and relative dietary intakes in terms of macro and micronutrients of GFDs followed by adult and pediatric CD patients in the world.
Methods
The present systematic review was performed according to the guidelines of the preferred reporting items for systematic review and meta-analyses (PRISMA-P; see Supplementary Table 1) [11]. The methodological quality of the included studies was rated through the Newcastle–Ottawa scale [12], which was simplified to two items (i.e., representativeness of the exposed cohort and assessment of outcome) given the outcome of interest, i.e., the absolute and relative proportion of macro- and micro-nutrients in GFD.
Literature search and study selection
A comprehensive literature search was independently performed by three investigators (MG; LF; US) up to October 2022 by querying PubMed, Scopus, and Scholar using controlled vocabulary, medical subject headings (MeSH) terms, and using different combinations of the following terms: “gluten-free diet”, “composition”, “nutrition”, “coeliac disease”, “nutrient intake”, “micronutrient intake”, “macronutrient intake”, “vitamin intake”, “mineral intake” and “fiber intake”. The PubMed search string was: (diet, gluten free[MeSH Terms]) OR (composition[All fields] OR nutrition[All fields]) AND (coeliac disease[MeSH Terms]).
We included studies on coeliac patients on GFD providing data on the average daily absolute energy intake or the average daily percentage or absolute intake of nutrients, i.e., carbohydrates, proteins, fats, saturated fats, fibers, sodium, calcium, iron, magnesium, and vitamin D. Papers with information on at least one nutrient and assessing daily intake with 24-h, 3-day or 7-day dietary records were included. Prospective and retrospective studies with no minimum number of patients, published in the English language were considered for inclusion. We excluded studies published in abstract form or considering non-CD patients on GFD. CD patients were defined as those with a confirmed diagnosis of CD based on clinical symptoms, immunological tests, and histopathological pictures of biopsies taken from the duodenum.
Titles and abstracts were first screened. Subsequently, the authors assessed the full body of potentially relevant screened studies and included those satisfying the inclusion criteria. Disputes were resolved by collegial discussion. The reason for excluding studies from the selection process was recorded.
Data extraction
The same three authors who performed the search (MG; LF; US) extracted data independently from the included studies on a pre-specified datasheet. Discrepancies were resolved by verifying from the full text of the study of concern. The following data were extracted from each study: design and country, number of centers involved, study size, demographics of patients (i.e., mean age and gender distribution), duration of GFD, absolute and relative macronutrient (i.e., carbohydrates, proteins, fats, saturated fats, and fibers) and micronutrient (i.e., sodium, calcium, iron, magnesium, and vitamin D) intake. For the purpose of the analyses, data on absolute energy intake expressed as KJ or MJ were converted into Kcal. Values expressed as mmol/day were converted into g/day or mg/day, as appropriate.
Outcome assessment
The primary outcome was the average daily percentage of intake of nutrients provided by the GFD. The key secondary outcome was the absolute daily average intake of energy (Kcal) and nutrients for the GFD, according to age groups (<9, 9–<13, 13–<18, and >18). In the age stratification analysis, five studies could not be included as age distribution was not available. Studies providing outcome data separately for males and females were included on a per-arm basis. However, a stratified analysis by gender was not feasible due to the limited number of studies providing data separately for males and females.
To offer an easy interpretation of data to all health professionals, especially those not specialized in nutrition, the recommended intakes provided by the “Dietary Reference Values for nutrients—Summary Report” of the European Food Safety Authority (EFSA) [13] were taken into consideration as benchmark. Given the global overview of this study, the “2020–2025 Dietary Guidelines for Americans” of the U.S. Dept. of Health and Human services and U.S. Dept. of Agriculture [14] were also considered.
Statistical analysis
Means were pooled through a random effects model, and presented as point estimates with a 95% confidence interval (CI). Statistical heterogeneity was computed through the I2 statistic, defined as high if I2 > 50%, and tested through the Q2 test (statistical significance set as p < 0.1). To explore possible sources of heterogeneity, we performed meta-regression and subgroup analyses. Variables potentially impacting on the outcomes were selected a priori and included: publication year, country, study design, and mean age of patients. In meta-regression analysis, we computed the R2 statistic, being the proportion of variance explained by the model for each potential predictor. In subgroup analysis, we compared subsets through a likelihood ratio test to assess for significant differences. To investigate publication bias, we drew a funnel plot and performed the Egger regression test. All the analyses were performed with R statistical software [15] with metafor package [16].
Results
Study characteristics and quality
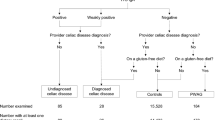
The literature search yielded 3515 articles (Fig. 1). Based on the inclusion criteria, 38 published articles were included in the systematic review, for a total of 2114 CD patients on a GFD. The patients’ age ranged from 8 to 59 years, and 32–95% were females. Twenty-nine studies [1774 (84%) patients] were performed in Europe, and 9 [340 (16%) patients] outside Europe. Twenty-two studies [1048 (49.6%) patients] were retrospective in design, whereas 16 [1066 (50.4%) patients] prospective. The publication year ranged from 1994 to 2022. The GFD mean duration ranged from 1 to 21 years. Characteristics and main outcomes of the included studies are summarized in Table 1.
Nutrient intakes as a percentage of the gluten-free diet
Main outcomes are reported in Fig. 2. Nineteen studies including 1351 coeliac subjects on GFD reported data on the daily average percentage intake of carbohydrates [the pooled result was 47.8% (CI, 45.7–49.8%) with high heterogeneity (I2 = 98%)]. Nineteen studies including 1274 coeliac subjects on GFD reported data on the daily average percentage intake of proteins [the pooled result was 15.5% (CI, 14.8–16.2%) with high heterogeneity (I2 = 96%)]. Twenty studies including 1388 coeliac subjects on GFD reported data on the daily average percentage intake of fats [the pooled result was 35.8% (CI, 34.5–37%) with high heterogeneity (I2 = 95%)]. Fifteen studies including 1138 coeliac subjects on GFD reported data on the daily average percentage intake of saturated fats. The study by Larretxi et al. was considered an outlier and excluded from analysis. [17] The pooled result was 13.2% (CI, 12.4–14%) with high heterogeneity (I2 = 96%).
a Carbohydrates: summary effect = 47.8%, 95% CI (45.7–49.8%). b Proteins:summary effect = 15.5%, 95% CI (14.8–16.2%). c Fats:summary effect = 35.8%, 95% CI (34.5–37.0%). d Saturated fats: summary effect = 13.2% (of total fats), 95% CI (12.4–14.0%). Squares show mean values, the square’s size the weight while the lines reflect 95% confidence intervals (CI). Diamonds show pooled estimates.
Absolute nutrient intakes of the gluten-free diet
The overall pooled average intakes are reported in Fig. 3. All data showed high heterogeneity (I2). The average daily energy intake was 1995 Kcal (CI 1884–2106; I2 = 98%) with 239 g (CI 226–252, I2 = 96%) of carbohydrates, 77 g (CI 72–81, I2 = 97%) of proteins, 78 g (CI 73–83, I2 = 97%) of fats, 27 g (CI 23–31, I2 = 99%) of saturated fats, and finally 16 g (CI 15–18, I2 = 98%) of fiber.
a Energy: summary effect = 1995 kcal/day, 95% CI (1884–2106). b Carbohydrates: summary effect = 239 g/day, 95% CI (226–252). c Proteins: summary effect = 77 g/day, 95% CI (72–81). d Fats: summary effect = 78, 95% CI (73–83). e Saturated fats: summary effect = 27 g/day, 95% CI (23–31). f Fibers: summary effect = 16 g/day, 95% CI (15–18). Squares show mean values, the square’s size the weight while the lines reflect 95% confidence intervals (CI). Diamonds show pooled estimates.
Macronutrient and fiber intakes presented by age-stratification are summarized in Supplementary Figs. 1–3. The overall pooled average daily fiber intake was 15.5 g (CI 13.6–17.3) with high heterogeneity (I2 = 98%) with the following age-distribution: 13.4 (CI 8.4–18.5) g for children <9 years old, 12 (CI 9.3–14.7) g for children aged 9–<13, 13.3 (CI 7.8–18.8) g for adolescents aged 13–<18, and 18.9 (CI 16.5–21.4) g for adults (see Supplementary Fig. 2). The EFSA adequate fiber intake is 2 g/239 kcal (1MJ) from the age of 1 year and 25 g/day or 1.8–2.9 g/MJ in adults [13]. Applying the EFSA recommendations based on the average daily absolute energy intake (Supplementary Fig. 1a), the expected daily fiber intakes are as follows: 14.4 g for children <9 years old, 15.3 g between 9 and 13 years, and 18.3 g between 13 and 18 years. The expected fiber intake for adults is 18.8 g/day considering the average value (2.4 g/MJ) of the range above indicated.
The overall pooled average daily calcium intake was 896.2 (CI 787.8–1004.6) mg with high heterogeneity (I2 = 96%). When stratified by age, average calcium intake fulfilled recommendation in adults, but it did not in preadolescence and adolescence [578.0 (CI 224.7–931.2) mg for children <9 years old, 811.6 (CI 579.4–1043.7) mg for children aged 9–<13, 671.4 (CI 286.1–1056.7) mg for adolescents aged 13–<18, and 1004.9 (CI 866–1143.9) mg for adults] (Supplementary Fig. 4). Magnesium had a pooled average daily intake of 258.8 (CI 199.1–318.4) mg with high heterogeneity (I2 = 99%). Magnesium assumption complied with recommendation only in adults (357.2 CI 322.4–392.1 mg vs. 173.4 CI 68.2–278.7 mg in children <9 years old, 178.7 CI 114.6–242.7 mg in 9–<13 years old, and 184.6 CI 44.1–325.1 mg in 13–18 years old) (Supplementary Fig. 4). Daily iron intake averaged 10.7 (CI 8.9–12.5) mg with high heterogeneity (I2 = 99%). Adults (13.2 mg, CI 11.3–15) met the daily recommendations, whereas this was not true for preadolescents and adolescents [7.5 CI 4.7–10.2 mg <9 years old, 8 CI 5.3–10.8 mg in 9–<13, and 8.1 CI 3.0–13.2 mg in 13–18) (Supplementary Fig. 4). The overall pooled average daily vitamin D intake was 3.3 (CI 1.6–4.9) mcg with high heterogeneity (I2 = 99%). The EFSA vitamin D recommended adequate intake is 15 mcg/day for all healthy individuals over 1 year of age [13]. The lowest intakes occurred in children and adolescents [0.8 (CI −0.4–2.0) mcg for children <9 years old, 3.1 (CI 1.3–4.9) mcg for children aged 9–<13, 1.6 (CI −1.3–4.5) mcg for adolescents between 13 and 18 years old, and 5.1 (CI 1.4–8.8) mcg for adults] (Supplementary Fig. 5). Average daily sodium intake was 2203.9 (CI 1683.5–2724.4) mg with high heterogeneity (I2 = 99%), with the highest consumption in young children and adults (1725.6 CI 513.5–2937.7 mg in children <9 years old, 1707 CI 1079–2335 mg in 9–<13 years old, 1419 CI −29.4–2867.4 in 13–18 years old, and 2986.8 CI 2481.2–3492.5 mg in adults) (Supplementary Fig. 5).
Sensitivity analysis and publication bias
The heterogeneity impact of study design, publication year, country, and proportion of male patients is shown in Tables 2 and 3. In Northern Europe, GFDs had more saturated fats, as percentage (p < 0.001), and more absolute calories and nutrients except for sodium. Calcium (p < 0.001) resulted significantly higher in Northern than in Southern Europe. In Southern Europe, the percentage intake of protein (p = 0.04) and total fat (0.024) was higher than in Northern Europe. High fiber intake (p = 0.008) appears to be associated with prospective studies. Throughout years of publication, the absolute energy intake and quantity of carbohydrates significantly decreased (p 0.01 and p 0.001, respectively). This trend included protein, fat and saturated fat, calcium, magnesium, and iron intakes even though results were not statistically significant. Males consumed a higher relative proportion of saturated fats than females (p = 0.017).
The methodological quality of the included studies was judged as low, mostly due to retrospective design and unspecified adherence of patients to GFD. Study quality evaluation is detailed in Table 4. No significant publication bias was detected on the primary outcome (i.e., the percentage average daily intake of nutrients provided by the GFD), according to both the visual inspection of funnel plots (see Fig. 4) and the regression tests (p = 0.178, p = 0.492, p = 0.793, and p = 0.606 for carbohydrate, protein, fat, and saturated fat intake respectively).
Discussion
These systematic review and meta-analysis explored quality and quantity of GFD. The GFDs tended to abound in fats and especially saturated fats and to be inadequate in fiber intake. Further, calcium, magnesium and iron intakes were particularly inadequate among adolescents, whereas the vitamin D intake was insufficient for both children and adults. Protein intakes were overrepresented in all patients, while daily energy tended to be below recommendations. Most of these results are comparable to trends seen in the general population living in Western countries [18]. However, considering that GFD is a lifelong requirement for CD patients and these patients usually benefit from a follow-up, it is reasonable to guide them through valid eating habits. These eating habits may be even more effective if they take place in early life so as to be perpetuated thereafter.
In this analysis, GFDs tend to display a reversed trend in carbohydrate content, leaning toward the lower end of the EFSA recommended range, with a shift toward fats, which can cover more than 40% of the daily caloric intake [17, 19, 20]. This shift is a mimic of the high-fat (>35 E%) and low-carbohydrates (<50 E%) diet, whose long-term effects are unknown although some metabolic derangements potentially harm the vascular system due to chronic lipid profile unbalance and hyperhomocysteinemia [20,21,22]. When classified by age, absolute figures showed that teenagers consumed the largest quantity of total and saturated fat among all age groups. Preference for saturated fat seemed to start at 9 years of age and progressively increased peaking in adolescence. Such eating patterns can set the stage for early atherosclerosis and other metabolic dysfunctions in adulthood [21]. In a long-term follow-up study in Scottish CD patients, the authors found a four-fold increased standardized mortality ratio due to cerebrovascular diseases in childhood-diagnosed cases [23]. This result was not significant, but adequately powered follow-up studies are required. In this meta-regression analysis men had a considerable intake of saturated fats. This result is compatible with the hypothesis that men are motivated by the “strong taste” and are more prone to eating fatty and junk food than women [24]. Future studies may investigate this interesting association.
The overall dietary fiber intake was between 12 and 19 g/day among all age groups, being out of range for all. More specifically, the average fiber intake reached 93% of EFSA recommendations [13] in children below 9 years of age, 79% in those below 13 years, and 73% in adolescents. As for adults, fiber intake (19 g/day) was insufficient if the benchmark was the absolute recommended value of 25 g/day, but adequate when related to the average daily absolute energy intake. To have more than a benchmark can be confusing and this aspect needs to be considered when proposing reference intakes. In our opinion, the computation of fiber intake based on energy is more appropriate. When considering the USDA guidelines [14], fiber intakes did not reach two-thirds of the recommendations due to the more generous reference values in all age groups. It is not easy to introduce fiber when adhering to a GFD especially if people tend to stick to commercial products and do not use naturally gluten-free cereals. A recent population-based study in Sweden highlighted how the change from gluten-containing to GFD has led to a different food selection in adolescents [25]. Other recent systematic reviews underlined several nutritional deficiencies or excesses, which include some of our results [26,27,28]. In all these studies, it has been clear that CD patients need to be educated to adhere to a balanced diet, to the selection of naturally gluten-deprived food and pseudo-cereals during their follow-ups. Advocacy of a food composition database of gluten-free products in Canada was also suggested by Jamieson et al. [29]. Food labels will certainly improve knowledge of both CD patients and health professionals and will contribute to changes in eating habits. These changes should occur during youth to prevent the occurrence of non-communicable diseases. A low fiber intake, on top of being associated with constipation [30], may be an indirect cardiometabolic risk factor, expose to overweight due to a less satiating effect of food [31] and modify the microbiota.
Our study tried to expand previous isolated evidence showing that GFD may lead to micro-nutrient deficiencies [3]. Several nutrients such as calcium, magnesium and iron were insufficiently assumed in adolescents. Vitamin D dietary intake was also insufficient among all age groups, being at the lowest intake in children under 9 years, who did not reach 20% of the recommendations. These findings may imply both general and specific consequences such as skeletal alterations with reduced peak bone and increased risk of atopy and autoimmunity [32]. On the contrary, sodium intake was acceptable in children and adolescents, peaking in adults. This result was unexpected as saturated fat and sodium are often combinedly present in food items and sodium is also highly assumed when animal protein intakes are excessive. Sodium intake was assessed only in a small number of studies compared to other nutrients and this may explain the results.
Insightful hints come from the sensitivity analyses. Firstly, Northern Europe countries compared to Southern Europe yielded GFDs richer in saturated fats and calcium. One explanation might be related to the higher dietary content in butter and margarine in Northern Europe, compared with the higher consumption of olive oil in Southern Europe. Similar latitudinal comparisons could not be obtained in studies performed in the United States of America. Secondly, the absolute daily content in total calories tended to decrease over time. In detail, carbohydrate reduction was statistically significant in most recent studies. This may reflect a tendency toward a remodulation of GFD diets with a reduction of simple sugars. Intake of several other nutrients (i.e., calcium, iron, protein, fat and saturated fat) seems to have decreased over time. This might be explained by a decline in consumption of milk and red meat in recent years [33]. Nonetheless, such data should be taken cautiously, as metaregression and subgroup meta-analysis generally yield exploratory and not confirmatory results.
Our meta-analysis has strengths and limitations. The quality of most of the included studies was low, owing to the retrospective nature and the limited sample size. Moreover, the studies covered an extensive time span. This may imply changes in lifestyles, in selection of gluten-free products as well as changes in methodology assessment of investigators who have had access to different amount of information over the years. The list of gluten-free food has expanded considerably and food labels, even with a minimal description of nutrients, were not present in the past. Most studies were performed in Europe. The dietary intake assessment was not carried out uniformly across all studies, and not all studies reported exhaustive information on the patients’ characterization. Moreover, the analysis stratified by age groups was based on the mean age of the included subjects as the studies reported. Furthermore, very few studies covered nutrient intakes in children and adolescents. To monitor the diet of these age groups is an action to target. Taken altogether, such limitations clearly affect the degree of confidence in our estimates. However, we followed the PRISMA recommendations [11] for conducting systematic reviews and meta-analyses to offer a first comprehensive overview of gluten-free dietary patterns followed by CD patients belonging to all age groups, highlighting the pro and cons of such diet.
In conclusion, GFDs can expose to nutrient imbalance with potential health consequences in the long run. Whether that is due to specific nutrients, the whole diet and/or lifestyle habits is still to be determined. Given that life-long adherence to a GFD is the only treatment for CD, a thorough nutritional guidance (taking advantage of follow-ups) must be provided at any age but especially during youth, when disease prevention is possible and mandatory. These nutritional tips can also guide people with other diseases demanding GFD.
Data availability
Data will be made available upon request.
References
Caio G, Volta U, Sapone A, Leffler DA, Catassi C, Fasano A. Coeliac disease: a comprehensive current review. BMC Med. 2019;17. https://doi.org/10.1186/s12916-019-1380-z.
Vasagar B, Cox J, Herion JT, Ivanoff E. World epidemiology of non-coeliac gluten sensitivity. Minerva Gastroenterol Dietol. 2017;63:5–15. https://doi.org/10.23736/s1121-421x.16.02338-z.
Vici G, Belli L, Biondi M, Polzonetti V. Gluten free diet and nutrient deficiencies: a review. Clin Nutr. 2016;35:1236–41. https://doi.org/10.1016/j.clnu.2016.05.002.
Melini V, Melini F. Gluten-free diet: gaps and needs for a healthier diet. Nutrients. 2019;11. https://doi.org/10.3390/nu11010170.
Martin J, Geisel T, Maresch C, Krieger K, Stein J. Inadequate nutrient intake in patients with coeliac disease: results from a German dietary survey. Digestion. 2013;87:240–6. https://doi.org/10.1159/000348850.
Shepherd SJ, Gibson PR. Nutritional inadequacies of the gluten-free diet in both recently-diagnosed and long-term patients with coeliac disease. J Hum Nutr Diet J Br Diet Assoc. 2013;26:349–58. https://doi.org/10.1111/jhn.12018.
Wild D, Robins GG, Burley VJ, Howdle PD. Evidence of high sugar intake, and low fibre and mineral intake, in the gluten-free diet. Aliment Pharm Ther. 2010;32:573–81. https://doi.org/10.1111/j.1365-2036.2010.04386.x.
Jones AL. The gluten-free diet: fad or necessity? Diabetes Spectr Publ Am Diabetes Assoc. 2017;30:118–23. https://doi.org/10.2337/ds16-0022.
Niland B, Cash BD. Health benefits and adverse effects of a gluten-free diet in non–coeliac disease patients. Gastroenterol Hepatol. 2018;14:82–91.
Potter MDE, Brienesse SC, Walker MM, Boyle A, Talley NJ. Effect of the gluten-free diet on cardiovascular risk factors in patients with coeliac disease: a systematic review. J Gastroenterol Hepatol. 2018;33:781–91. https://doi.org/10.1111/jgh.14039.
Moher D, Liberati A, Tetzlaff J, Altam DG,PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9, W64.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011; http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
EFSA (European Food Safety Authority). Dietary reference values for nutrients summary report 2017—EFSA Supporting Publications-Wiley Online Library. 2017;e1521:98 pp. https://doi.org/10.2903/sp.efsa.2017.e15121.
U.S. Dept of Agricoltureand U.S. Dept of Health and Human Services. Dietary guidelines for Americans, 2020-2025 and online materials|Dietary Guidelines for Americans. https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
Viechtbauer W. Conducting meta-analyses in R with the metafor Package. J Stat Softw. 2010;36:1–48. https://doi.org/10.18637/jss.v036.i03.
Larretxi I, Simon E, Benjumea L, Miranda J, Bustamante MA, Lasa A, et al. Gluten-free-rendered products contribute to imbalanced diets in children and adolescents with coeliac disease. Eur J Nutr. 2019;58:775–83. https://doi.org/10.1007/s00394-018-1685-2.
Van Rossum C, Fransen H, Verkaik-Kloosterman J, Buurma-Rethans EJM, Ocke MC. Dutch National Food Consumption Survey 2007-2010: diet of children and adults aged 7 to 69 years. RIVM Rapp. 2011;350050006:148.
Babio N, Alcázar M, Castillejo G, Recasens M, Martínez-Cerezo F, Gutiérrez-Pensado V, et al. Patients with coeliac disease reported higher consumption of added sugar and total fat than healthy individuals. J Pediatr Gastroenterol Nutr. 2017;64:63–9. https://doi.org/10.1097/MPG.0000000000001251.
Ballestero Fernández C, Varela-Moreiras G, Úbeda N, Alonso-Aperte E. Nutritional status in Spanish children and adolescents with coeliac disease on a gluten free diet compared to non-coeliac disease controls. Nutrients. 2019;11. https://doi.org/10.3390/nu11102329.
Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–86. https://doi.org/10.1161/CIRCULATIONAHA.110.016170.
McFarlane XA, Marsham J, Reeves D, Bhalla AK, Robertson DAF. Subclinical nutritional deficiency in treated coeliac disease and nutritional content of the gluten free diet. J Hum Nutr Diet. 1995;8:231–7. https://doi.org/10.1111/j.1365-277X.1995.tb00316.x.
Quarpong W, Card TR, West J, Solaymani-Dodaran M, Logan RFA, Grainge MJ. Mortality in people with coeliac disease: long-term follow-up from a Scottish cohort. UEGJ. 2019;7:377–87. https://doi.org/10.1177/2050640618814662.
Grzymisławska M, Puch E, Zawada A, Grzymisławski M. Do nutritional behaviors depend on biological sex and cultural gender? Adv Clin Exp Med. 2020;29:165–72. https://doi.org/10.17219/acem/111817.
Kautto E, Rydén PJ, Ivarsson A, Olsson C, Norström F, Högberg L, et al. What happens to food choices when a gluten-free diet is required? A prospective longitudinal population-based study among Swedish adolescent with coeliac disease and their peers. J Nutr Sci. 2014;3:e2. https://doi.org/10.1017/jns.2013.24.
Cardo A, Churruca I, Lasa A, Navarro V, Vázquez-Polo M, Perez-Junkera G, et al. Nutritional imbalances in adult celiac patients following a gluten-free diet. Nutrients. 2021;13:2877. https://doi.org/10.3390/nu13082877.
Di Nardo G, Villa MP, Conti L, Ranucci G, Pacchiarotti C, Principessa L, et al. Nutritional deficiencies in children with celiac disease resulting from a gluten-free diet: a systematic review. Nutrients. 2019;11:1588. https://doi.org/10.3390/nu11071588.
Caeiro C, Pragosa C, Carreira Cruz M, Pereira CD, Gonçalves Pereira S. The role of pseudocereals in celiac disease: reducing nutritional deficiencies to improve well-being and health. J Nutr Metab. 2022. https://doi.org/10.1155/2022/8502169.
WW Jamieson JA, Gill K, Fisher S, English M. Development of a Canadian food composition database of gluten-free products. Foods. 2022;11:2215. https://doi.org/10.3390/foods11152215.
Macêdo MIP, Albuquerque MDFM, Tahan S, de MoraisIs MB. Is there any association between overweight, physical activity, fat and fiber intake with functional constipation in adolescents? Scand J Gastroenterol. 2020;55:414–20. https://doi.org/10.1080/00365521.2020.1749878.
Slavin JL. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2008;108:1716–31. https://doi.org/10.1016/j.jada.2008.08.007.
Bailey ADL, Fulgoni III VL, Shah N, Patterson AC, Gutierrez-Orozco F, Mathews RS, et al. Nutrient intake adequacy from food and beverage intake of US children aged 1-6 years from NHANES 2001-2016. Nutrients. 2021;13. https://doi.org/10.3390/nu13030827.
U.S. Dept of Agriculture - Economic Research Service. Food Availability and consumption Data System. 2012. https://www.ers.usda.gov/data-products/food-availability-per-capita-data-system/.
Author information
Authors and Affiliations
Contributions
Concept and design: MG, LFrazzoni and MLF. Analysis and interpretation of the data: MG, LFrazzoni, LFuccio and MLF. Drafting of the article: all authors. Collection and assembly of data: MG, LFrazzoni and US. Critical revision of the article for important intellectual content: all authors. Final approval of the article: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gessaroli, M., Frazzoni, L., Sikandar, U. et al. Nutrient intakes in adult and pediatric coeliac disease patients on gluten-free diet: a systematic review and meta-analysis. Eur J Clin Nutr 77, 784–793 (2023). https://doi.org/10.1038/s41430-023-01280-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01280-0