Abstract
Objective
To assess the effects of prepubertal BMI on pubertal growth patterns, and the influence of prepubertal BMI and pubertal growth patterns on long-term BMI among Chinese children and adolescents.
Methods
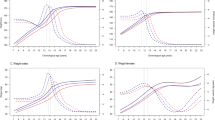
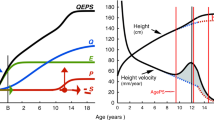
A total of 9606 individuals aged between 7 and 18 years from longitudinal surveys in Zhongshan city of China from 2005 to 2016 were enrolled. Age at peak height velocity (APHV) and peak height velocity (PHV) were estimated using Super-Imposition by Translation and Rotation (SITAR) model. Associations between prepubertal BMI, APHV, PHV, and long-term overweight and obesity were assessed by linear regression and multinominal logistic regression. Scatter plots were elaborated to show the associations between prepubertal BMI and pubertal growth patterns according to prepubertal BMI categories.
Results
Prepubertal BMI Z-Score was positively correlated with long-term BMI Z-Score, and negatively correlated with APHV in both sexes. In addition, there was a negative association between prepubertal BMI Z-Score and PHV in boys. With 1-year decrease in APHV, risk of long-term underweight decreased by 92%, while overweight increased by 33% in boys. Corresponding risk of long-term underweight and overweight for girls decreased by 42% and increased by 20%, respectively.
Conclusion
High prepubertal BMI levels were associated with earlier APHV and lower PHV, and the early onset of pubertal development could increase the risks of long-term overweight and obesity at 17–18 years of age both in boys and girls. Such evidence emphasized the importance of reducing prepubertal obesity risks combined with appropriate pubertal development timing, including later APHV and higher PHV, so as to prevent the obesity and related cardiovascular diseases in adulthood.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data are available from the corresponding author on reasonable request.
Code availability
The computer code and data sets generated and/or analyzed in the present study are not publicly available due to the need to protect participants privacy but are available from the corresponding author on reasonable request.
References
NCD Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395:65–74.
Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. 2017;377:2145–53.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51.
Patton GC, Viner R. Pubertal transitions in health. Lancet. 2007;369:1130–9.
Viner RM, Ross D, Hardy R, Kuh D, Power C, Johnson A, et al. Life course epidemiology: recognising the importance of adolescence. J Epidemiol Community Health. 2015;69:719–20.
Li W, Liu Q, Deng X, Chen Y, Liu S, Story M. Association between obesity and puberty timing: a systematic review and meta-analysis. Int J Environ Res Public Health. 2017;14:1266.
Gavela-Perez T, Garces C, Navarro-Sanchez P, Lopez Villanueva L, Soriano-Guillen L. Earlier menarcheal age in Spanish girls is related with an increase in body mass index between pre-pubertal school age and adolescence. Pediatr Obes. 2015;10:410–5.
Wagner IV, Sabin MA, Pfaffle RW, Hiemisch A, Sergeyev E, Korner A, et al. Effects of obesity on human sexual development. Nat Rev Endocrinol. 2012;8:246–54.
Barcellos Gemelli I, Farias E, Souza O. Age at menarche and its association with excess weight and body fat percentage in girls in the southwestern region of the Brazilian Amazon. J Pediatr Adolesc Gynecol. 2016;29:482–8.
Aksglaede L, Juul A, Olsen L, Sørensen T. Age at puberty and the emerging obesity epidemic. PLoS ONE. 2009;4:e8450.
Mouritsen A, Aksglaede L, Soerensen K, Hagen C, Petersen J, Main K, et al. The pubertal transition in 179 healthy Danish children: associations between pubarche, adrenarche, gonadarche, and body composition. Eur J Endocrinol. 2013;168:129–36.
Denzer C, Weibel A, Muche R, Karges B, Sorgo W, Wabitsch M. Pubertal development in obese children and adolescents. Int J Obes. 2007;31:1509–19.
Day FR, Elks CE, Murray A, Ong KK, Perry JR. Puberty timing associated with diabetes, cardiovascular disease and also diverse health outcomes in men and women: the UK Biobank study. Sci Rep. 2015;5:11208.
Wang Y. Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics. 2002;110:903–10.
Song Y, Ma J, Agardh A, Lau PW, Hu P, Zhang B. Secular trends in age at menarche among Chinese girls from 24 ethnic minorities, 1985 to 2010. Glob Health Action. 2015;8:26929.
Song Y, Ma J, Wang HJ, Wang Z, Hu P, Zhang B, et al. Trends of age at menarche and association with body mass index in Chinese school-aged girls, 1985-2010. J Pediatr. 2014;165:1172–7.e1.
Song Y, Ma J, Li L, Dong B, Wang Z, Agardh A. Secular trends for age at spermarche among Chinese boys from 11 ethnic minorities, 1995-2010: a multiple cross-sectional study. BMJ Open. 2016;6:e010518.
Cooper R, Blell M, Hardy R, Black S, Pollard TM, Wadsworth ME, et al. Validity of age at menarche self-reported in adulthood. J Epidemiol Community Health. 2006;60:993–7.
Walker IV, Smith CR, Davies JH, Inskip HM, Baird J. Methods for determining pubertal status in research studies: literature review and opinions of experts and adolescents. J Dev Orig Health Dis. 2020;11:168–87.
Malina R, Choh A, Czerwinski S, Chumlea W. Validation of maturity offset in the fels longitudinal study. Pediatr Exerc Sci. 2016;28:439–55.
Carrascosa A, Yeste D, Moreno-Galdo A, Gussinye M, Ferrandez A, Clemente M, et al. Pubertal growth of 1,453 healthy children according to age at pubertal growth spurt onset. The Barcelona longitudinal growth study. An Pediatr. 2018;89:144–52.
Gasser T, Sheehy A, Largo RH. Statistical characterization of the pubertal growth spurt. Ann Hum Biol. 2001;28:395–402.
Bygdell M, Kindblom JM, Celind J, Nethander M, Ohlsson C. Childhood BMI is inversely associated with pubertal timing in normal-weight but not overweight boys. Am J Clin Nutr. 2018;108:1259–63.
Chen LK, Wang G, Bennett WL, Ji Y, Pearson C, Radovick S, et al. Trajectory of body mass index from ages 2 to 7 years and age at peak height velocity in boys and girls. J Pediatr. 2021;230:221–9.e5.
Ahmed M, Ong K, Dunger D. Childhood obesity and the timing of puberty. Trends Endocrinol Metab. 2009;20:237–42.
Tzoulaki I, Sovio U, Pillas D, Hartikainen A, Pouta A, Laitinen J, et al. Relation of immediate postnatal growth with obesity and related metabolic risk factors in adulthood: the northern Finland birth cohort 1966 study. Am J Epidemiol. 2010;171:989–98.
Boeyer M, Middleton K, Duren D, Leary E. Estimating peak height velocity in individuals: a comparison of statistical methods. Ann Hum Biol. 2020;47:434–45.
Wang X, Dong B, Huang S, Ma Y, Zou Z, Ma J, et al. Body mass index trajectory and incident hypertension: results from a longitudinal cohort of Chinese children and adolescents, 2006-16. Am J Public Health. 2020;110:1689–95.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Silva AB, Capingana DP, Magalhaes P, Goncalves MA, Molina MD, Rodrigues SL, et al. Cardiovascular risk factors in pre-pubertal schoolchildren in Angola. Cardiovasc J Afr. 2016;27:315–21.
Buyken AE, Karaolis-Danckert N, Remer T. Association of prepubertal body composition in healthy girls and boys with the timing of early and late pubertal markers. Am J Clin Nutr. 2009;89:221–30.
Cole TJ, Donaldson MD, Ben-Shlomo Y. SITAR-a useful instrument for growth curve analysis. Int J Epidemiol. 2010;39:1558–66.
Cole TJ, Kuh D, Johnson W, Ward KA, Howe LD, Adams JE, et al. Using Super-Imposition by Translation And Rotation (SITAR) to relate pubertal growth to bone health in later life: the Medical Research Council (MRC) National Survey of Health and Development. Int J Epidemiol. 2016;45:1125–34.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17:95–107.
Starc G, Strel J. Tracking excess weight and obesity from childhood to young adulthood: a 12-year prospective cohort study in Slovenia. Public Health Nutr. 2011;14:49–55.
Fonseca M, Oliveira A, Azevedo I, Nunes J, Santos A. Association of pubertal development with adiposity and cardiometabolic health in girls and boys-findings from the generation XXI birth cohort. J Adolesc Health. 2019;65:558–63.
Sandhu J, Ben-Shlomo Y, Cole TJ, Holly J, Davey Smith G. The impact of childhood body mass index on timing of puberty, adult stature and obesity: a follow-up study based on adolescent anthropometry recorded at Christ’s Hospital (1936-64). Int J Obes. 2006;30:14–22.
He Q, Karlberg J. Bmi in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001;49:244–51.
Fan H, Lee Y, Hsieh R, Yang C, Chen Y. Body mass index growth trajectories, early pubertal maturation, and short stature. Pediatr Res. 2020;88:117–24.
Biro FM, Khoury P, Morrison JA. Influence of obesity on timing of puberty. Int J Androl. 2006;29:272–7.
Bygdell M, Kindblom JM, Jansson JO, Ohlsson C. Revisiting the critical weight hypothesis for regulation of pubertal timing in boys. Am J Clin Nutr. 2020;113:123–8.
Boyne MS, Thame M, Osmond C, Fraser RA, Gabay L, Taylor-Bryan C, et al. The effect of earlier puberty on cardiometabolic risk factors in Afro-Caribbean children. J Pediatr Endocrinol Metab. 2014;27:453–60.
Widen E, Silventoinen K, Sovio U, Ripatti S, Cousminer DL, Hartikainen AL, et al. Pubertal timing and growth influences cardiometabolic risk factors in adult males and females. Diabetes Care. 2012;35:850–6.
Reinehr T, Roth CL. Is there a causal relationship between obesity and puberty? Lancet Child Adolesc Health. 2019;3:44–54.
Clayton PE, Trueman JA. Leptin and puberty. Arch Dis Child. 2000;83:1–4.
Mayes JS, Watson GH. Direct effects of sex steroid hormones on adipose tissues and obesity. Obes Rev. 2004;5:197–216.
Prentice P, Viner R. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes. 2013;37:1036–43.
Silventoinen K, Haukka J, Dunkel L, Tynelius P, Rasmussen F. Genetics of pubertal timing and its associations with relative weight in childhood and adult height: the Swedish Young Male Twins Study. Pediatrics. 2008;121:e885–91.
Yoshii K, Isojima T, Piedvache A, Morisaki N, Tanaka T, Nagata S. Reduced pubertal growth in children with obesity regardless of pubertal timing. Endocr J. 2020;67:477–84.
Oh CM, Oh IH, Choi KS, Choe BK, Yoon TY, Choi JM. Relationship between body mass index and early menarche of adolescent girls in Seoul. J Prev Med Public Health. 2012;45:227–34.
Kindblom JM, Lorentzon M, Norjavaara E, Lonn L, Brandberg J, Angelhed JE, et al. Pubertal timing is an independent predictor of central adiposity in young adult males: the Gothenburg osteoporosis and obesity determinants study. Diabetes 2006;55:3047–52.
Rogol A, Clark P, Roemmich J. Growth and pubertal development in children and adolescents: effects of diet and physical activity. Am J Clin Nutr. 2000;72:521S–8S.
Acknowledgements
The authors would like to acknowledge the support from all the team members and the participating students, teachers, parents and local education and health staff in the programs.
Funding
The present study was supported by the National Natural Science Foundation (Grant 81673192 to JM; 82103865 to YD), and Beijing Natural Science Foundation (No. 7222244 to YD), as well as the China Postdoctoral Science Foundation (BX20200019 and 2020M680266 to YD).
Author information
Authors and Affiliations
Contributions
YL, DG, and JL conceptualized and designed the study, completed the statistical analyses, drafted the initial paper, and reviewed and revised the paper; YD and JM contributed to the conceptualization and design of the study, supervised the data collection, the statistical analyses and initial drafting of the paper, and reviewed and revised the paper; BD, YS, and SH assisted with the statistical analyses and critically reviewed and revised the paper; ZY, BW, LC, MC, YM, and TM assisted with the data processing, statistical analyses, and the interpretation of the data. All authors approved the final paper as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving students were approved by the Medical Research Ethics Committee of the Peking University Health Science Center (IRB00001052-20011). All participants and their parents signed informed consents voluntarily.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Li, Y., Gao, D., Liu, J. et al. Prepubertal BMI, pubertal growth patterns, and long-term BMI: Results from a longitudinal analysis in Chinese children and adolescents from 2005 to 2016. Eur J Clin Nutr 76, 1432–1439 (2022). https://doi.org/10.1038/s41430-022-01133-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01133-2