Abstract
Background/objectives
Diet is an important factor that can exacerbate or ameliorate chronic inflammation, which has been implicated in the pathogenesis of nonalcoholic fatty liver disease (NAFLD). However, no prospective study has yet investigated the relation between the inflammatory potential of diet and NAFLD. The aim of this study was to investigate the association between the inflammatory potential of the diet and the risk of NAFLD.
Subject/methods
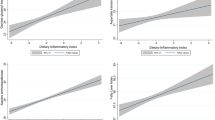
The study included 12,877 participants aged over 18 years (mean [standard deviation]: 39.4 [11.5] years). Dietary intake was assessed at baseline through food frequency questionnaires. Using white blood cell count as the inflammatory marker, we newly created a dietary inflammatory potential score by reduced rank regression and stepwise linear regression. NAFLD was identified by abdominal ultrasound during yearly health checkups. Cox proportional hazards regression models were used to estimate the association between the dietary inflammatory potential score and the risk of NAFLD.
Results
During a median follow-up period of 4.2 years, 2744 first incident cases of NAFLD occurred. After adjustment for potential confounders, the multivariable hazards ratios (95% confidence intervals) for NAFLD across increasing quartiles of the dietary inflammatory potential score were 1.00 (reference), 1.01 (0.90, 1.13), 1.15 (1.03, 1.29), and 1.26 (1.13, 1.41), with P for trend <0.0001. This positive association appeared greater in men than in women (P for interaction = 0.02).
Conclusions
Our results indicate that a dietary pattern with high inflammatory potential is associated with a higher risk of NAFLD. Such findings provide the support that inflammation may be a potential mechanism linking diet to the risk of NAFLD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Loomba R, Friedman SL, Shulman GI. Mechanisms and disease consequences of nonalcoholic fatty liver disease. Cell. 2021;184:2537–64. https://doi.org/10.1016/j.cell.2021.04.015.
Lee HW, Wong VW. Changing NAFLD epidemiology in China. Hepatology. 2019;70:1095–8. https://doi.org/10.1002/hep.30848.
Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69:896–904. https://doi.org/10.1016/j.jhep.2018.05.036.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62:S47–64. https://doi.org/10.1016/j.jhep.2014.12.012. 1 Suppl.
Mantovani A, Petracca G, Beatrice G, Tilg H, Byrne CD, Targher G. Non-alcoholic fatty liver disease and risk of incident diabetes mellitus: an updated meta-analysis of 501 022 adult individuals. Gut. 2021;70:962–9. https://doi.org/10.1136/gutjnl-2020-322572.
Mantovani A, Petracca G, Beatrice G, Csermely A, Lonardo A, Schattenberg JM, et al. Non-alcoholic fatty liver disease and risk of incident chronic kidney disease: an updated meta-analysis. Gut. 2022;71:156–62. https://doi.org/10.1136/gutjnl-2020-323082.
Wattacheril J. Extrahepatic manifestations of nonalcoholic fatty liver disease. Gastroenterol Clin North Am. 2020;49:141–9. https://doi.org/10.1016/j.gtc.2019.10.002.
Simon TG, Roelstraete B, Khalili H, Hagstrom H, Ludvigsson JF. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: results from a nationwide cohort. Gut 2020. https://doi.org/10.1136/gutjnl-2020-322786.
Petroni ML, Brodosi L, Bugianesi E, Marchesini G. Management of non-alcoholic fatty liver disease. BMJ. 2021;372:m4747 https://doi.org/10.1136/bmj.m4747.
Minihane AM, Vinoy S, Russell WR, Baka A, Roche HM, Tuohy KM, et al. Low-grade inflammation, diet composition and health: current research evidence and its translation. Br J Nutr. 2015;114:999–1012. https://doi.org/10.1017/S0007114515002093.
Ilich JZ, Kelly OJ, Kim Y, Spicer MT. Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Arh Hig Rada Toksikol. 2014;65:139–48. https://doi.org/10.2478/10004-1254-65-2014-2541.
He K, Li Y, Guo X, Zhong L, Tang S. Food groups and the likelihood of non-alcoholic fatty liver disease: a systematic review and meta-analysis. Br J Nutr. 2020;1–13. https://doi.org/10.1017/S0007114520000914.
Alferink LJ, Kiefte-de Jong JC, Erler NS, Veldt BJ, Schoufour JD, de Knegt RJ, et al. Association of dietary macronutrient composition and non-alcoholic fatty liver disease in an ageing population: the Rotterdam Study. Gut. 2019;68:1088–98. https://doi.org/10.1136/gutjnl-2017-315940.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipido. 2002;13:3–9. https://doi.org/10.1097/00041433-200202000-00002.
Tabung FK, Smith-Warner SA, Chavarro JE, Wu K, Fuchs CS, Hu FB, et al. Development and validation of an empirical dietary inflammatory index. J Nutr. 2016;146:1560–70. https://doi.org/10.3945/jn.115.228718.
Xia Y, Zhang Q, Liu L, Meng G, Wu H, Bao X, et al. Intermediary effect of inflammation on the association between dietary patterns and non-alcoholic fatty liver disease. Nutrition. 2020;71:110562 https://doi.org/10.1016/j.nut.2019.110562.
Chung GE, Yim JY, Kim D, Kwak MS, Yang JI, Chung SJ, et al. Associations between white blood cell count and the development of incidental nonalcoholic fatty liver disease. Gastroenterol Res Pr. 2016;2016:7653689 https://doi.org/10.1155/2016/7653689.
Wang S, Zhang C, Zhang G, Yuan Z, Liu Y, Ding L, et al. Association between white blood cell count and non-alcoholic fatty liver disease in urban Han Chinese: a prospective cohort study. BMJ Open. 2016;6:e010342 https://doi.org/10.1136/bmjopen-2015-010342.
Zhang S, Gu Y, Bian S, Lu Z, Zhang Q, Liu L, et al. Soft drink consumption and risk of nonalcoholic fatty liver disease: results from the Tianjin Chronic Low-Grade Systemic Inflammation and Health (TCLSIH) cohort study. Am J Clin Nutr. 2021;113:1265–74. https://doi.org/10.1093/ajcn/nqaa380.
Yang YX, Wang GY, XC P. China food composition, 2nd edn. Beijing, China: Peking University Medical Press; 2009.
Tabung FK, Wang W, Fung TT, Hu FB, Smith-Warner SA, Chavarro JE, et al. Development and validation of empirical indices to assess the insulinaemic potential of diet and lifestyle. Br J Nutr. 2016;1–12. https://doi.org/10.1017/S0007114516003755.
Hoffmann K, Schulze MB, Schienkiewitz A, Nothlings U, Boeing H. Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am J Epidemiol. 2004;159:935–44. https://doi.org/10.1093/aje/kwh134.
Farrell GC, Chitturi S, Lau GK, Sollano JD, Asia-Pacific Working Party on N. Guidelines for the assessment and management of non-alcoholic fatty liver disease in the Asia-Pacific region: executive summary. J Gastroenterol Hepatol. 2007;22:775–7. https://doi.org/10.1111/j.1440-1746.2007.05002.x.
National Workshop on Fatty L, Alcoholic Liver Disease CSoHCMA, Fatty Liver Expert Committee CMDA. [Guidelines of prevention and treatment for nonalcoholic fatty liver disease: a 2018 update]. Zhonghua Gan Zang Bing Za Zhi. 2018;26:195–203. https://doi.org/10.3760/cma.j.issn.1007-3418.2018.03.008.
Zhang S, Gu Y, Wang L, Zhang Q, Liu L, Lu M, et al. Association between dietary raw garlic intake and newly diagnosed nonalcoholic fatty liver disease: a population-based study. Eur J Endocrinol. 2019;181:591–602. https://doi.org/10.1530/EJE-19-0179.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. https://doi.org/10.1249/01.MSS.0000078924.61453.FB.
Lee HC, Chiu HF, Wing YK, Leung CM, Kwong PK, Chung DW. The Zung Self-rating Depression Scale: screening for depression among the Hong Kong Chinese elderly. J Geriatr Psychiatry Neurol. 1994;7:216–20. https://doi.org/10.1177/089198879400700404.
Zhou YJ, Li YY, Nie YQ, Huang CM, Cao CY. Natural course of nonalcoholic fatty liver disease in southern China: a prospective cohort study. J Dig Dis. 2012;13:153–60. https://doi.org/10.1111/j.1751-2980.2011.00571.x.
Zhou BF, Cooperative Meta-Analysis Group of the Working Group on Obesity in C. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults-study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96.
Ishikawa-Takata K, Tabata I. Exercise and physical activity reference for health promotion 2006 (EPAR2006). J Epidemiol. 2007;17:177 https://doi.org/10.2188/jea.17.177.
Yu YY, Cai JT, Song ZY, Tong YL, Wang JH. The associations among Helicobacter pylori infection, white blood cell count and nonalcoholic fatty liver disease in a large Chinese population. Medicine. 2018;97:e13271 https://doi.org/10.1097/MD.0000000000013271.
Lee YJ, Lee HR, Shim JY, Moon BS, Lee JH, Kim JK. Relationship between white blood cell count and nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42:888–94. https://doi.org/10.1016/j.dld.2010.04.005.
Li X, Yu C, Guo Y, Bian Z, Shen Z, Yang L, et al. Association between tea consumption and risk of cancer: a prospective cohort study of 0.5 million Chinese adults. Eur J Epidemiol. 2019;34:753–63. https://doi.org/10.1007/s10654-019-00530-5.
Yang J, Mao QX, Xu HX, Ma X, Zeng CY. Tea consumption and risk of type 2 diabetes mellitus: a systematic review and meta-analysis update. BMJ Open. 2014;4:e005632 https://doi.org/10.1136/bmjopen-2014-005632.
Liu X, Xu W, Cai H, Gao YT, Li H, Ji BT, et al. Green tea consumption and risk of type 2 diabetes in Chinese adults: the Shanghai Women’s Health Study and the Shanghai Men’s Health Study. Int J Epidemiol. 2018;47:1887–96. https://doi.org/10.1093/ije/dyy173.
Xia Y, Wang X, Zhang S, Zhang Q, Liu L, Meng G, et al. Daily tea drinking is not associated with newly diagnosed non-alcoholic fatty liver disease in Chinese adults: the Tianjin chronic low-grade systemic inflammation and health cohort study. Nutr J. 2019;18:71 https://doi.org/10.1186/s12937-019-0502-y.
Hassani Zadeh S, Mansoori A, Hosseinzadeh M. Relationship between dietary patterns and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2020; https://doi.org/10.1111/jgh.15363.
Yaskolka Meir A, Rinott E, Tsaban G, Zelicha H, Kaplan A, Rosen P, et al. Effect of green-Mediterranean diet on intrahepatic fat: the DIRECT PLUS randomised controlled trial. Gut. 2021; https://doi.org/10.1136/gutjnl-2020-323106.
Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006;48:677–85. https://doi.org/10.1016/j.jacc.2006.03.052.
Jones N, Blagih J, Zani F, Rees A, Hill DG, Jenkins BJ, et al. Fructose reprogrammes glutamine-dependent oxidative metabolism to support LPS-induced inflammation. Nat Commun. 2021;12:1209 https://doi.org/10.1038/s41467-021-21461-4.
Spruss A, Kanuri G, Wagnerberger S, Haub S, Bischoff SC, Bergheim I. Toll-like receptor 4 is involved in the development of fructose-induced hepatic steatosis in mice. Hepatology. 2009;50:1094–104. https://doi.org/10.1002/hep.23122.
Wang Y, Qi W, Song G, Pang S, Peng Z, Li Y, et al. High-fructose diet increases inflammatory cytokines and alters gut microbiota composition in rats. Mediators Inflamm. 2020;2020:6672636 https://doi.org/10.1155/2020/6672636.
Guerra S, Mocciaro G, Gastaldelli A. Adipose tissue insulin resistance and lipidome alterations as the characterizing factors of non-alcoholic steatohepatitis. Eur J Clin Invest. 2021;e13695. https://doi.org/10.1111/eci.13695.
Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542:177–85. https://doi.org/10.1038/nature21363.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–7. https://doi.org/10.1038/nature05485.
Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54:1082–90. https://doi.org/10.1002/hep.24452.
Acknowledgements
We are grateful to all the people that have made this study.
Funding
This study was supported by grants from the National Natural Science Foundation of China (Nos. 81941024 and 81872611), 2014 and 2016 Chinese Nutrition Society (CNS) Nutrition Research Foundation—DSM Research Fund (Nos. 2016-046, 2014-071 and 2016–023), Study of Diet and Nutrition Assessment and Intervention Technology (No. 2020YFC2006300) from Active Health and Aging Technologic Solutions Major Project of National Key R&D Program——Development and application of key technologies for nutrition and health food at specific physiological stages (Nos. 2020YFC2006304, 2020YFC2006302, and 2020YFC2006305), National Health Commission of China (No. SPSYYC 2020015) and SZ is a recipient of a scholarship under the China Scholarship Council to pursue his study in Sweden (No. 202006940030).
Author information
Authors and Affiliations
Contributions
SZ analyzed the data and wrote the paper. SZ, GM, QZ, LL, HW, YG, YW, TZ, XW, JZ, SS, XW, MZ, QJ, KS, and YW conducted research. LQ and KN designed the research and had primary responsibility for the final content. All authors had full access to all the data in the study and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, S., Meng, G., Zhang, Q. et al. Inflammatory potential of diet and risk of nonalcoholic fatty liver disease: a prospective cohort study. Eur J Clin Nutr 76, 1125–1132 (2022). https://doi.org/10.1038/s41430-022-01069-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01069-7
This article is cited by
-
The association between dietary inflammation scores and non-alcoholic fatty liver diseases in Iranian adults
BMC Gastroenterology (2022)