Abstract
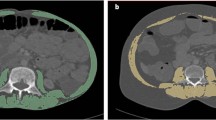
Skeletal muscle plays a crucial part in the metabolic and inflammatory response. “Sarcopenia”, defined as a pathological condition of reduced strength, quantity and quality of skeletal muscle mass, may often develop in the young age as the secondary consequence of a systemic inflammatory illness, like cancer. In children with cancer, sarcopenia is a common finding, playing a negative role in their prognosis. However, its prevalence in clinical practice is underestimated. Moreover, several pre- and post-natal factors may influence skeletal muscle development in childhood, making the issue more complex. Given the frequent use of radiological imaging in clinical practice, prompt analysis of body composition is feasible and able to detect the presence of reduced fat-free mass (FFM) among pediatric patients with cancer. We discuss the recent advances in the study of body composition in children with cancer, dissecting the role of the psoas muscle area (PMA) measure, obtained from computerized tomography (CT) or magnetic resonance images (MRI) as a marker of sarcopenia in this setting. Since age and sex-specific percentile curves for PMA and a PMA z-scores calculator are available online, such a tool may be useful to simply detect and treat sarcopenia and its consequences in childhood cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Landi F, Calvani R, Cesari M, Tosato M, Martone AM, Ortolani E, et al. Sarcopenia: an Overview on Current Definitions, Diagnosis and Treatment. Curr Protein Pept Sci. 2018;19:633–8.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. (2019). Erratum in: Age Ageing. 2018; 48:601.
Fearon K, Evans WJ, Anker SD. Myopenia-a new universal term for muscle wasting. J Cachexia Sarcopenia Muscle. 2011;2:1–3. https://doi.org/10.1007/s13539-011-0025-7.
Bauer J, Morley JE, Schols AMWJ, Ferrucci L, Cruz-Jentoft AJ, Dent E, et al. Sarcopenia: a Time for Action. An SCWD Position Paper. J Cachexia Sarcopenia Muscle. 2019;10:956–61. https://doi.org/10.1002/jcsm.12483.
Triarico S, Rinninella E, Cintoni M, Capozza MA, Mastrangelo S, Mele MC, et al. Impact of malnutrition on survival and infections among pediatric patients with cancer: a retrospective study. Eur Rev Med Pharm Sci. 2019;23:1165–75.
Joffe L, Schadler KL, Shen W, Ladas EJ. Body composition in pediatric solid tumors: state of the science and future directions. J Natl Cancer Inst Monogr. 2019;54:144–8.
Ooi PH, Thompson-Hodgetts S, Pritchard-Wiart L, Gilmour SM, Mager DR. Pediatric Sarcopenia: a Paradigm in the Overall Definition of Malnutrition in Children? JPEN J Parenter Enter Nutr. 2020;44:407–18.
Romero NB, Mezmezian M, Fidziańska A. Main steps of skeletal muscle development in the human: morphological analysis and ultrastructural characteristics of developing human muscle. Handb Clin Neurol. 2013;113:1299–310.
Orsso CE, Tibaes JRB, Oliveira CLP, Rubin DA, Field CJ, Heymsfield SB, et al. Low muscle mass and strength in pediatrics patients: Why should we care? Clin Nutr. 2019;38:2002–15.
Du M, Yan X, Tong JF, Zhao J, Zhu MJ. Maternal obesity, inflammation, and fetal skeletal muscle development. Biol Reprod. 2010;82:4–12.
Cabeço LC, Budri PE, Baroni M, Castan EP, Carani FR, de Souza PA, et al. Maternal protein restriction induce skeletal muscle changes without altering the MRFs MyoD and myogenin expression in offspring. J Mol Histol. 2012;43:461–71.
Verdijk LB, Snijders T, Drost M, Delhaas T, Kadi F, van Loon LJ. Satellite cells in human skeletal muscle; from birth to old age. Age (Dordr). 2014;36:545–7.
Chen Z, Li L, Wu W, Liu Z, Huang Y, Yang L, et al. Exercise protects proliferative muscle satellite cells against exhaustion via the Igfbp7-Akt-mTOR axis. Theranostics. 2020;10:6448–66.
Akhmedov D, Berdeaux R. The effects of obesity on skeletal muscle regeneration. Front Physiol. 2013;4:371.
Thivel D, Ring-Dimitriou S, Weghuber D, Frelut ML, O’Malley G. Muscle Strength and Fitness in Pediatric Obesity: a Systematic Review from the European Childhood Obesity Group. Obes Facts. 2016;9:52–63.
Veldhuis JD, Roemmich JN, Richmond EJ, Rogol AD, Lovejoy JC, Sheffield-Moore M, et al. Endocrine control of body composition in infancy, childhood, and puberty. Endocr Rev. 2005;26:114–46.
Mitchell WK, Wilkinson DJ, Phillips BE, Lund JN, Smith K, Atherton PJ. Human Skeletal Muscle Protein Metabolism Responses to Amino Acid Nutrition. Adv Nutr. 2016;7:828S–38S.
Garlick PJ. Protein requirements of infants and children. Nestle Nutr Workshop Ser Pediatr Program. 2006;58:39–47. https://doi.org/10.1159/000095009.
Arisaka O, Ichikawa G, Koyama S, Sairenchi T. Childhood obesity: rapid weight gain in early childhood and subsequent cardiometabolic risk. Clin Pediatr Endocrinol. 2020;29:135–42.
Berrazaga I, Micard V, Gueugneau M, Walrand S. The Role of the Anabolic Properties of Plant- versus Animal-Based Protein Sources in Supporting Muscle Mass Maintenance: a Critical Review. Nutrients. 2019;11:1825.
Anjanappa M, Corden M, Green A, Roberts D, Hoskin P, McWilliam A. Sarcopenia in cancer: risking more than muscle loss. Tech Innov Patient Support Radiat Oncol. 2020;16:50–7.
Chindapasirt J. Sarcopenia in Cancer Patients. Asian Pac J Cancer Prev. 2015;16:8075–7.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. The malnutrition overlap syndromes of cachexia and sarcopenia: a malnutrition conundrum. Am J Clin Nutr. 2018;6:1157–8.
Vanhoutte G, van de Wiel M, Wouters K, Sels M, Bartolomeeussen L, De Keersmaecker S, et al. Cachexia in cancer: what is in the definition? BMJ Open Gastroenterol. 2016;3:e000097.
Blum D, Stene GB, Solheim TS, Fayers P, Hjermstad MJ, Baracos VE, et al. Euro-Impact. Validation of the Consensus-Definition for Cancer Cachexia and evaluation of a classification model–a study based on data from an international multicentre project (EPCRC-CSA). Ann Oncol. 2014;25:1635–42.
Soeters PB, Jensen GL, Hsiao PY, Allison SP, Sobotka L. Nutritional aspects of chronic inflammatory disease. In: Sobotka L Basics in Clinical Nutrition. 5th edn. Prague:Galen Publishing House; 2019. p. 185–90.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31:1539–47.
Polyzos SA, Margioris AN. Sarcopenic obesity. Hormones (Athens). 2018;17:321–31.
Murphy AJ, White M, Davies PS. Body composition of children with cancer. Am J Clin Nutr. 2010;92:55–60. https://doi.org/10.3945/ajcn.2010.29201.
Murphy AJ, White M, Elliott SA, Lockwood L, Hallahan A, Davies PS. Body composition of children with cancer during treatment and in survivorship. Am J Clin Nutr. 2015; 102891–6. https://doi.org/10.3945/ajcn.114.099697.
Baracos VE, Arribas L. Sarcopenic obesity: hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann Oncol. 2018;29:ii1–ii9.
Marriott CJC, Beaumont LF, Farncombe TH, Cranston AN, Athale UH, Yakemchuk VN, et al. Body composition in long-term survivors of acute lymphoblastic leukemia diagnosed in childhood and adolescence: a focus on sarcopenic obesity. Cancer. 2018;124:1225–31.
Mueske NM, Mittelman SD, Wren TAL, Gilsanz V, Orgel E. Myosteatosis in adolescents and young adults treated for acute lymphoblastic leukemia. Leuk Lymphoma. 2019;60:3146–53.
Levy E, Samoilenko M, Morel S, England J, Amre D, Bertout L, et al. Cardiometabolic Risk Factors in Childhood, Adolescent and Young Adult Survivors of Acute Lymphoblastic Leukemia - A Petale Cohort. Sci Rep. 2017;7:17684.
Zhang Y, Wang JP, Wang XL, Tian H, Gao TT, Tang LM, et al. Computed tomography-quantified body composition predicts short-term outcomes after gastrectomy in gastric cancer. Curr Oncol. 2018;25:e411–e422.
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008;9:629–35.
Prado CM, Lima IS, Baracos VE, Bies RR, McCargar LJ, Reiman T, et al. An exploratory study of body composition as a determinant of epirubicin pharmacokinetics and toxicity. Cancer Chemother Pharm. 2011;67:93–101.
Thompson PA, Rosner GL, Matthay KK, Moore TB, Bomgaars LR, Ellis KJ, et al. Impact of body composition on pharmacokinetics of doxorubicin in children: a Glaser Pediatric Research Network study. Cancer Chemother Pharm. 2009;64:243–51.
Rinninella E, Cintoni M, Raoul P, Pozzo C, Strippoli A, Bria E, et al. Muscle mass, assessed at diagnosis by L3-CT scan as a prognostic marker of clinical outcomes in patients with gastric cancer: a systematic review and meta-analysis. Clin Nutr. 2020;39:2045–54.
Rinninella E, Fagotti A, Cintoni M, Raoul P, Scaletta G, Scambia G, et al. Skeletal muscle mass as a prognostic indicator of outcomes in ovarian cancer: a systematic review and meta-analysis. Int J Gynecol Cancer. 2020;30:654–63.
Rinninella E, Cintoni M, Raoul P, Ponziani FR, Pompili M, Pozzo C, et al. Prognostic value of skeletal muscle mass during tyrosine kinase inhibitor (TKI) therapy in cancer patients: a systematic review and meta-analysis. Intern Emerg Med. 2020;16:1341–56. https://doi.org/10.1007/s11739-020-02589-5.
Rinninella E, Ruggiero A, Maurizi P, Triarico S, Cintoni M, Mele MC. Clinical tools to assess nutritional risk and malnutrition in hospitalized children and adolescents. Eur Rev Med Pharm Sci. 2017;21:2690–701.
Lazzer S, Bedogni G, Agosti F, De Col A, Mornati D, Sartorio A. Comparison of dual-energy X-ray absorptiometry, air displacement plethysmography and bioelectrical impedance analysis for the assessment of body composition in severely obese Caucasian children and adolescents. Br J Nutr. 2008;100:918–24.
Cooper C, Fielding R, Visser M, van Loon LJ, Rolland Y, Orwoll E, et al. Tools in the assessment of sarcopenia. Calcif Tissue Int. 2013;93:201–10.
Amini B, Boyle SP, Boutin RD, Lenchik L. Approaches to assessment of muscle mass and myosteatosis on computed tomography (CT): a systematic review. J Gerontol A Biol Sci Med Sci. 2019;74:1671–8.
Lurz E, Patel H, Frimpong RG, Ricciuto A, Kehar M, Wales PW, et al. Sarcopenia in children with end‐stage liver disease. J Pediatr Gastroenterol Nutr. 2018;66:222–6.
Mangus RS, Bush WJ, Miller C, Kubal CA. Severe sarcopenia and increased fat stores in pediatric patients with liver, kidney, or intestine failure. J Pediatr Gastroenterol Nutr. 2017;65:579–83.
Zhang H, Tao Y, Wang Z, Lu J. Evaluation of nutritional status and prognostic impact assessed by the prognostic nutritional index in children with chronic kidney disease. Med (Baltim). 2019;98:e16713.
Lurz E, Patel H, Lebovic G, Quammie C, Woolfson JP, Perez M, et al. Paediatric reference values for total psoas muscle area. J Cachexia Sarcopenia Muscle. 2020;11:405–14.
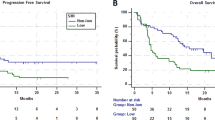
Suzuki D, Kobayashi R, Sano H, Hori D, Kobayashi K. Sarcopenia after induction therapy in childhood acute lymphoblastic leukemia: its clinical significance. Int J Hematol. 2018;107:486–9.
Kawakubo N, Kinoshita Y, Souzaki R, Koga Y, Oba U, Ohga S, et al. The Influence of Sarcopenia on High-Risk Neuroblastoma. J Surg Res. 2019;236:101–5.
Ritz A, Kolorz J, Hubertus J, Ley-Zaporozhan J, von Schweinitz D, Koletzko S, et al. Sarcopenia is a prognostic outcome marker in children with high-risk hepatoblastoma. Pediatr Blood Cancer. 2021;68:e28862. https://doi.org/10.1002/pbc.28862.
Golse N, Bucur PO, Ciacio O, Pittau G, Sa Cunha A, Adam R, et al. A new definition of sarcopenia in patients with cirrhosis undergoing liver transplantation. Liver Transpl. 2016;23:143–54. https://doi.org/10.1002/lt.24671.
Author information
Authors and Affiliations
Contributions
MCM designed the overall study with contributions from MC. ST and GA wrote the paper. AR revised the paper. ER discussed and edited the paper. All authors finally approve the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Triarico, S., Rinninella, E., Mele, M.C. et al. Prognostic impact of sarcopenia in children with cancer: a focus on the psoas muscle area (PMA) imaging in the clinical practice. Eur J Clin Nutr 76, 783–788 (2022). https://doi.org/10.1038/s41430-021-01016-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-01016-y
This article is cited by
-
The impact of sarcopenia and sarcopenic obesity on survival in children with Ewing sarcoma and osteosarcoma
Pediatric Radiology (2023)