Abstract
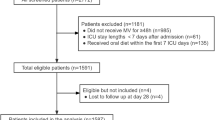
Indirect calorimetry (IC)-guided nutrition might positively affect the clinical outcome of critically ill patients. In this systematic review and meta-analysis, our objective was to assess the benefit of isocaloric nutrition guided by IC, compared to hypocaloric nutrition, for critically ill patients admitted to the intensive care unit (ICU). We performed a systematic review of all randomized controlled trials published through January 2021, assessing the benefit of isocaloric nutrition guided by IC. The primary outcome was 28-day all-cause mortality. Secondary outcomes were ICU and 90-day all-cause mortality, rate of nosocomial infections, and adverse events. Four trials evaluating 1052 patients were included. Patients treated with isocaloric nutrition had a lower 28-day mortality rate (risk ratio (RR) 0.79, 95% confidence interval (CI) 0.63–0.99, P = 0.04). No between-group difference was found in ICU and 90-day mortality (RR 0.92, 95% CI 0.68–1.23, P = 0.56 and RR 0.88, 95% CI 0.72–1.07; P = 0.2, respectively) and in the rate of nosocomial infections (RR 1.15, 95% CI 0.77–1.72, P = 0.51). A pooled analysis of studies that evaluated the benefit of isocaloric nutrition guided by IC, for critically ill patients in the ICU, has shown reduced 28-day mortality. However, there was no difference in 90-day mortality and nosocomial infection rate.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310:1591–600.
Paddon-Jones D, Sheffield-Moore M, Cree MG, Hewlings SJ, Aarsland A, Wolfe RR, et al. Atrophy and impaired muscle protein synthesis during prolonged inactivity and stress. J Clin Endocrinol Metab. 2006;91:4836–41.
Biolo G, Fleming RYD, Maggi SP, Nguyen TT, Herndon DN, Wolfe RR. Inverse regulation of protein turnover and amino acid transport in skeletal muscle of hypercatabolic patients. J Clin Endocrinol Metab. 2002;87:3378–84.
Rennie MJ. Muscle protein turnover and the wasting due to injury and disease. Br Med Bull. 1985;41:257–64.
Ochala J, Gustafson A-M, Diez ML, Renaud G, Li M, Aare S, et al. Preferential skeletal muscle myosin loss in response to mechanical silencing in a novel rat intensive care unit model: underlying mechanisms. J Physiol. 2011;589:2007–26.
Vesali RF, Cibicek N, Jakobsson T, Klaude M, Wernerman J, Rooyackers O. Protein metabolism in leg muscle following an endotoxin injection in healthy volunteers. Clin Sci. 2009;118:421–7.
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38:48–79.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. J Parenter Enter Nutr. 2016;40:159–211.
Achamrah N, Delsoglio M, De Waele E, Berger MM, Pichard C. Indirect calorimetry: the 6 main issues. Clin Nutr. 2021;40:4–14.
Tatucu-Babet OA, Ridley EJ, Tierney AC. Prevalence of underprescription or overprescription of energy needs in critically ill mechanically ventilated adults as determined by indirect calorimetry: a systematic literature review. JPEN J Parenter Enter Nutr. 2016;40:212–25.
Frankenfield DC, Coleman A, Alam S, Cooney RN. Analysis of estimation methods for resting metabolic rate in critically ill adults. JPEN J Parenter Enter Nutr. 2009;33:27–36.
Walker RN, Heuberger RA. Predictive equations for energy needs for the critically ill. Respir Care. 2009;54:509–21.
Reeves MM, Capra S. Predicting energy requirements in the clinical setting: are current methods evidence based?. Nutr Rev. 2003;61:143–51.
Kagan I, Zusman O, Bendavid I, Theilla M, Cohen J, Singer P. Validation of carbon dioxide production (VCO2) as a tool to calculate resting energy expenditure (REE) in mechanically ventilated critically ill patients: a retrospective observational study. Crit Care. 2018;22:186.
Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care. 2016;20:367
Rattanachaiwong S, Singer P. Indirect calorimetry as point of care testing. Clin Nutr. 2019;38:2531–44.
Yeh DD, Fuentes E, Quraishi SA, Cropano C, Kaafarani H, Lee J, et al. Adequate nutrition may get you home: effect of caloric/protein deficits on the discharge destination of critically ill surgical patients. JPEN J Parenter Enter Nutr. 2016;40:37–44.
De Waele E, Honoré PM, Malbrain MLNG. Does the use of indirect calorimetry change outcome in the ICU? Yes it does. Curr Opin Clin Nutr Metab Care. 2018;21:126–9.
Landes S, McClave SA, Frazier TH, Lowen CC, Hurt RT. Indirect calorimetry: is it required to maximize patient outcome from nutrition therapy?. Curr Nutr Rep. 2016;5:233–9.
Lambell KJ, Tatucu-Babet OA, Chapple L-A, Gantner D, Ridley EJ. Nutrition therapy in critical illness: a review of the literature for clinicians. Crit Care. 2020;24:35
Allingstrup MJ, Kondrup J, Wiis J, Claudius C, Pedersen UG, Hein-Rasmussen R, et al. Early goal-directed nutrition versus standard of care in adult intensive care patients: the single-centre, randomised, outcome assessor-blinded EAT-ICU trial. Intensive Care Med. 2017;43:1637–47.
Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Lev S, et al. The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med. 2011;37:601–9.
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013;381:385–93.
Petros S, Horbach M, Seidel F, Weidhase L. Hypocaloric vs normocaloric nutrition in critically ill patients: a prospective randomized pilot trial. JPEN J Parenter Enter Nutr. 2016;40:242–9.
Singer P, De Waele E, Sanchez C, Ruiz Santana S, Montejo JC, Laterre PF, et al. TICACOS international: a multi-center, randomized, prospective controlled study comparing tight calorie control versus Liberal calorie administration study. Clin Nutr. 2021;40:380–7.
Tatucu-Babet OA, Fetterplace K, Lambell K, Miller E, Deane AM, Ridley EJ. Is energy delivery guided by indirect calorimetry associated with improved clinical outcomes in critically ill patients? A systematic review and meta-analysis. Nutr Metab Insights. 2020;13:1178638820903295.
Cochrane Handbook for Systematic Reviews of Interventions. http://www.cochrane-handbook-systematic-reviews-interventions. Accessed 15 Jan 2021.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097
James Thomas JH. Cochrane handbook for systematic reviews of interventions 2019. http://www.handbook/current. Accessed Apr 2020.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Mustafa RA, Santesso N, Brozek J, Akl EA, Walter SD, Norman G, et al. The GRADE approach is reproducible in assessing the quality of evidence of quantitative evidence syntheses. J Clin Epidemiol. 2013;66:736–42.
de Azevedo JRA, Lima HCM, Montenegro WS, de Carvalho Souza SC, Nogueira IROM, Silva MM, et al. Optimized calorie and high protein intake versus recommended caloric-protein intake in critically ill patients: a prospective, randomized, controlled phase II clinical trial. Rev Bras Ter Intensiv. 2019;31:171–9.
Gonzalez-Granda A, Schollenberger A, Haap M, Riessen R, Bischoff SC. Optimization of nutrition therapy with the use of calorimetry to determine and control energy needs in mechanically ventilated critically ill patients: the ONCA study, a randomized, prospective pilot study. JPEN J Parenter Enter Nutr. 2019;43:481–9.
Wernerman J, Christopher KB, Annane D, Casaer MP, Coopersmith CM, Deane AM, et al. Metabolic support in the critically ill: a consensus of 19. Crit Care. 2019;23:318.
Arabi YM, Casaer MP, Chapman M, Heyland DK, Ichai C, Marik PE, et al. The intensive care medicine research agenda in nutrition and metabolism. Intensive Care Med. 2017;43:1239–56.
Weijs PJM, Mogensen KM, Rawn JD, Christopher KB. Protein Intake, Nutritional Status and Outcomes in ICU Survivors: A Single Center Cohort Study. J Clin Med. 2019;8:43 https://doi.org/10.3390/jcm8010043.
Weijs PJM, Looijaard WGPM, Beishuizen A, Girbes ARJ, Oudemans-van Straaten HM. Early high protein intake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients. Crit Care. 2014;18:701
Author information
Authors and Affiliations
Contributions
BP, HB-Y, and JM have conducted the search for relevant articles. BP and HB-Y conducted the double extraction. PS, HB-Y, and BP have written the manuscript. IK, YDG, and IBD have revised the manuscript and assisted in statistical analysis
Corresponding author
Ethics declarations
Conflict of interest
PS is the first author in two trials that were included in this review. There are no other conflicts of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pertzov, B., Bar-Yoseph, H., Menndel, Y. et al. The effect of indirect calorimetry guided isocaloric nutrition on mortality in critically ill patients—a systematic review and meta-analysis. Eur J Clin Nutr 76, 5–15 (2022). https://doi.org/10.1038/s41430-021-00919-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00919-0
This article is cited by
-
Efficacy of permissive underfeeding for critically ill patients: an updated systematic review and trial sequential meta-analysis
Journal of Intensive Care (2024)
-
Personalized nutrition therapy in critical care: 10 expert recommendations
Critical Care (2023)
-
Laborchemisches und kalorimetrisches Monitoring der medizinischen Ernährungstherapie auf der Intensiv- und Intermediate Care Station
Medizinische Klinik - Intensivmedizin und Notfallmedizin (2023)
-
Clinical nutrition issues in 2022: What is missing to trust supplemental parenteral nutrition (SPN) in ICU patients?
Critical Care (2022)
-
Routine use of indirect calorimetry in critically ill patients: pros and cons
Critical Care (2022)