Abstract
Background
Processed foods have been implicated in the pathogenesis of inflammatory bowel diseases (IBD). Our goal was to develop a validated processed foods frequency questionnaire (PFQ) and assess its reliability and validity.
Methods
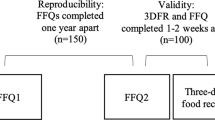
We recruited adult IBD patients to fill-in a PFQ in this prospective single-center study. Food intake was categorized into three groups of processed food levels: unprocessed, processed, and ultra-processed. Reliability was assessed by comparing the PFQ results of each patient at 2 time points. Validity was assessed by comparing the PFQ results to a 3–7 day food diary (FD), and by comparing urine sodium as a biomarker for the high intake of sodium that is mostly present in processed food.
Results
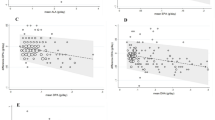
Eighty-six IBD patients were enrolled. Good test–retest reliability was indicated by intraclass correlation of 0.75–0.88 for the different food processing levels. Validity was fair-to-strong as assessed by correlations for different levels of processed food intake between FDs and PFQ, ranging between 0.43 and 0.64 (Pearsonr, P < 0.001), and further supported by higher mean urine sodium levels in patients with high processed foods consumption compared with low consumption (104.57 ± 53.26 vs. 78.62 ± 39.08 mmol/L, respectively, P = 0.022). Agreement between PFQ and the FD in categorizing patients to high and low processed food consumption groups was fair (Kappa 0.23–0.35).
Conclusions
The PFQ is a reliable and valid tool for the assessment of processed foods consumption in IBD patients and can be utilized for studying the association between processed food consumption and IBD etiopathogenesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.e42.
Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017;152:313–21.e2.
Levine A, Sigall Boneh R, Wine E. Evolving role of diet in the pathogenesis and treatment of inflammatory bowel diseases. Gut. 2018;67:1726–38.
Lewis JD, Abreu MT. Diet as a trigger or therapy for inflammatory bowel diseases. Gastroenterology. 2017;152:398–414.e6.
Sarbagili-Shabat C, Sigall-Boneh R, Levine A. Nutritional therapy in inflammatory bowel disease. Curr Opin Gastroenterol. 2015;31:303–8.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9.
Monteiro CA, Moubarac J-C, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev.2013;14(Suppl 2):21–8.
Rashvand S, Behrooz M, Samsamikor M, Jacobson K, Hekmatdoost A. Dietary patterns and risk of ulcerative colitis: a case-control study. J Hum Nutr Diet. 2018;31:408–12.
D’Souza S, Levy E, Mack D, Israel D, Lambrette P, Ghadirian P, et al. Dietary patterns and risk for Crohn’s disease in children. Inflamm Bowel Dis. 2008;14:367–73.
Chassaing B, Van De Wiele T, De Bodt J, Marzorati M, Gewirtz AT. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut. 2017;66:1414–27.
Jowett SL, Seal CJ, Pearce MS, Phillips E, Gregory W, Barton JR, et al. Influence of dietary factors on the clinical course of ulcerative colitis: a prospective cohort study. Gut. 2004;53:1479–84.
Zinöcker MK, Lindseth IA. The western diet-microbiome-host interaction and its role in metabolic disease. Nutrients. 2018;10:365.
Albenberg L, Brensinger CM, Wu Q, Gilroy E, Kappelman MD, Sandler RS, et al. A diet low in red and processed meat does not reduce rate of crohn’s disease flares. Gastroenterology. 2019;157:128–136.e5.
Santos Costa C, Del-Ponte B, Cecília M, Assunção F, Santos IS. Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review. Public Health Nutr. 2018;21:148–59.
Nelson MC, Lytle LA. Development and evaluation of a brief screener to estimate fast-food and beverage consumption among adolescents. J Am Diet Assoc. 2009;109:730–4.
Cantwell M, Mittl B, Curtin J, Carroll R, Potischman N, Caporaso N, et al. Relative validity of a food frequency questionnaire with a meat-cooking and heterocyclic amine module. Cancer Epidemiol Biomark Prev. 2004;13:293–8.
De Cock N, Van Camp J, Kolsteren P, Lachat C, Huybregts L, Maes L, et al. Development and validation of a quantitative snack and beverage food frequency questionnaire for adolescents. J Hum Nutr Diet. 2017;30:141–50.
Neuhouser ML, Lilley S, Lund A, Johnson DB. Development and validation of a beverage and snack questionnaire for use in evaluation of school nutrition policies. J Am Diet Assoc. 2009;109:1587–92.
Laura Da Costa Louzada M, Galastri Baraldi L, Martinez Steele E, Paula A, Martins B, Canella DS, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15.
Schnabel L, Buscail C, Sabate JM, Bouchoucha M, Kesse-Guyot E, Allès B, et al. Association between ultra-processed food consumption and functional gastrointestinal disorders: results from the french NutriNet-Santé cohort. Am J Gastroenterol. 2018;113:1217–28.
Fiolet T, Srour B, Sellem L, Kesse-Guyot E, Allès B, Méjean C, et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:322.
Miele E, Shami R, Aloi M, Assa A, Braegger C, Bronsky J, et al. Nutrition in pediatric inflammatory bowel disease: a position paper on behalf of the porto inflammatory bowel disease group of the european society of pediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr. 2018;66:687–708.
Forbes A, Escher J, Hébuterne X, Kłęk S, Krznaric Z, Schneider S, et al. ESPEN guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr. 2017;36:321–47.
Monteiro CA, Cannon G, Moubarac J-C, Levy RB, Louzada MLC, Jaime PC. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21:5–17.
Eicher-Miller HA, Fulgoni VL III, Keast DR. Contributions of processed foods to dietary intake in the us from 2003–2008: a report of the food and nutrition science solutions joint task force of the academy of nutrition and dietetics, american society for nutrition, institute of food technologists, and international food information council. J Nutr. 2012;142:2065S.
Moubarac J-C, Parra DC, Cannon G, Monteiro CA. Food classification systems based on food processing: significance and implications for policies and actions: a systematic literature review and assessment. Curr Obes Rep. 2014;3:256–72.
Monteiro CA, Cannon G, Levy RB, Moubarac J-C, Louzada ML, Rauber F, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22:936–41.
Monteiro CA, Levy RB, Claro RM, Castro IRR, de, Cannon G. A new classification of foods based on the extent and purpose of their processing. Cad Saude Publica. 2010;26:2039–49.
Lam MCL, Adams J. Association between home food preparation skills and behaviour, and consumption of ultra-processed foods: cross-sectional analysis of the UK National Diet and nutrition survey (2008-2009). Int J Behav Nutr Phys Act. 2017;14:68.
MABAT. First Israeli national health and nutrition survey 1999–2001 part 2: what Israelis eat. Food and nutrition services, Ministry of Health and Israel Center for Disease Control. Publication no. 228. 2004. https://www.health.gov.il/PublicationsFiles/Mabat_1999-2001-b.pdf.
Mercado CI, Cogswell ME, Valderrama AL, Wang C-Y, Loria CM, Moshfegh AJ, et al. Difference between 24-h diet recall and urine excretion for assessing population sodium and potassium intake in adults aged 18–39 y. Am J Clin Nutr. 2015;101:376–86.
Umesawa M, Yamagishi K, Noda H, Ikeda A, Sawachi S, Muraki I, et al. The relationship between sodium concentrations in spot urine and blood pressure increases: a prospective study of Japanese general population: the Circulatory Risk in Communities Study (CIRCS). BMC Cardiovasc Disord. 2016;16:55.
Lee S-G, Lee W, Kwon OH, Kim J-H. Association of urinary sodium/creatinine ratio and urinary sodium/specific gravity unit ratio with blood pressure and hypertension: KNHANES 2009–2010. Clin Chim Acta. 2013;424:168–73.
Joosten MM, Gansevoort RT, Mukamal KJ, Lambers Heerspink HJ, Geleijnse JM, Feskens EJM, et al. Sodium excretion and risk of developing coronary heart disease. Circulation. 2014;129:1121–28.
Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38:791–813.
Ni Mhurchu C, Capelin C, Dunford EK, Webster JL, Neal BC, Jebb SA. Sodium content of processed foods in the United Kingdom: analysis of 44,000 foods purchased by 21,000 households. Am J Clin Nutr. 2011;93:594–600.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Charlton KE, Steyn K, Levitt NS, Jonathan D, Zulu JV, Nel JH. Development and validation of a short questionnaire to assess sodium intake. Public Health Nutr. 2007;11:83–94.
Lemogoum D, Ngatchou W, Lele CB, Okalla C, Leeman M, Degaute J-P, et al. Association of urinary sodium excretion with blood pressure and risk factors associated with hypertension among Cameroonian pygmies and bantus: a cross-sectional study. BMC Cardiovasc Disord. 2018;18:49.
Jian L, Binns CW, Lee AH. Validity of a food-frequency questionnaire for elderly men in southeast China. Public Health Nutr. 2006;9:928–33.
Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes. 2000;24:1119–30.
Mente A, O’Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392:496–506.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows—CSS: conceived and designed the study, did the data collection, performed the statistical analysis, and wrote the paper; SZS: conceived and designed the study, provided statistical input, helped with interpretation of the results, and reviewed the paper for important intellectual content; NFI, YR, and AH: contributed to data collection; NM: conceived and designed the study, supervised on data collection, helped with interpretation of the results, and reviewed the paper for important intellectual content; all the authors read and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sarbagili-Shabat, C., Zelber-Sagi, S., Fliss Isakov, N. et al. Development and validation of processed foods questionnaire (PFQ) in adult inflammatory bowel diseases patients. Eur J Clin Nutr 74, 1653–1660 (2020). https://doi.org/10.1038/s41430-020-0632-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0632-5
This article is cited by
-
Best practices for applying the Nova food classification system
Nature Food (2023)
-
Integrative development of a short screening questionnaire of highly processed food consumption (sQ-HPF)
International Journal of Behavioral Nutrition and Physical Activity (2022)