Abstract
Background/Objectives
The effect of dietary folate intake or folic acid (FA) supplementation during pregnancy on neonatal congenital heart defects (CHDs) remains inconclusive. There are limited data about non-folate-B-vitamin intake and the risk of CHDs. Furthermore, few studies have investigated dietary B-vitamin intake and B-vitamin supplement use simultaneously in relation to the risk of CHDs. This study aimed to explore the associations between maternal folate, vitamin B6, and vitamin B12 intake (dietary intake, total intake from diet and supplements); B-vitamin supplement use during pregnancy; and the risk of CHDs using the propensity score matching (PSM) method.
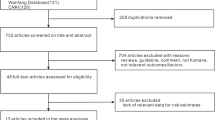
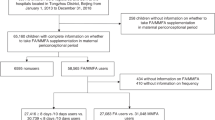
Methods
We conducted a case-control study and included 760 cases and 1600 controls in Shaanxi Province, China. Diet, supplement use and other information were collected through a questionnaire interview. By using the 1:2 ratio PSM method, 396 cases were matched with 792 controls. Conditional logistic regression was used to investigate the associations between maternal B-vitamin intake and supplement use during pregnancy and CHDs.
Results
Higher maternal dietary and total intake of folate and vitamin B12 were associated with reduced risk of CHDs, and the tests for linear trend were significant. Compared with non-users, maternal FA + VB6 + VB12 containing supplement use during pregnancy (OR 0.61, 95%CI 0.40–0.94), FA supplement use during pregnancy (OR 0.70, 95%CI 0.50–0.98) and in the first trimester (OR 0.62, 95%CI 0.46–0.85) were associated with a lower risk of CHDs.
Conclusions
The findings of this study suggest that a higher intake of folate and vitamin B12 during pregnancy reduces the risk of CHDs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
U.S. Department of Health & Human Services, National Heart, Lung, and Blood Institute. Congenital Heart Defects. [https://www.nhlbi.nih.gov/health-topics/congenital-heart-defects]
Dolk H, Loane M, Garne E. Congenital heart defects in Europe: prevalence and perinatal mortality, 2000 to 2005. Circulation. 2011;123:841–9.
Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800.
Jortveit J, Øyen N, Leirgul E, Fomina T, Tell GS, Vollset SE, et al. Trends in mortality of congenital heart defects. Congenit heart Dis. 2016;11:160–8.
Smedts HP, van Uitert EM, Valkenburg O, Laven JS, Eijkemans MJ, Lindemans J, et al. A derangement of the maternal lipid profile is associated with an elevated risk of congenital heart disease in the offspring. Nutr, Metab Cardiovascul Dis. 2012;22:477–85.
McNulty B, McNulty H, Marshall B, Ward M, Molloy AM, Scott JM, et al. Impact of continuing folic acid after the first trimester of pregnancy: findings of a randomized trial of folic acid supplementation in the second and third trimesters. Am J Clin Nutr. 2013;98:92–8.
Konstantinova SV, Vollset SE, Berstad P, Ueland PM, Drevon CA, Refsum H, et al. Dietary predictors of plasma total homocysteine in the Hordaland Homocysteine Study. Br J Nutr. 2007;98:201–10.
Smedts HP, Rakhshandehroo M, Verkleij-Hagoort AC, de Vries JH, Ottenkamp J, Steegers EA, et al. Maternal intake of fat, riboflavin and nicotinamide and the risk of having offspring with congenital heart defects. Eur J Nutr. 2008;47:357–65.
Verkleij-Hagoort AC, de Vries JH, Ursem NT, de Jonge R, Hop WC, Steegers-Theunissen RP. Dietary intake of B-vitamins in mothers born a child with a congenital heart defect. Eur J Nutr. 2006;45:478–86.
Bower C, Miller M, Payne J, Serna P. Folate intake and the primary prevention of non-neural birth defects. Aust N Z J Public Health. 2006;30:258–61.
Mao B, Qiu J, Zhao N, Shao Y, Dai W, He X, et al. Maternal folic acid supplementation and dietary folate intake and congenital heart defects. PLoS ONE. 2017;12:e0187996.
van Beynum IM, Kapusta L, Bakker MK, den Heijer M, Blom HJ, de Walle HEK. Protective effect of periconceptional folic acid supplements on the risk of congenital heart defects: a registry-based case-control study in the northern Netherlands. Eur Heart J. 2010;31:464–71.
Øyen N, Olsen SF, Basit S, Leirgul E, Strøm M, Carstensen L, et al. Association between maternal folic acid supplementation and congenital heart defects in offspring in birth cohorts From Denmark and Norway. J Am Heart Assoc. 2019;8:e011615.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424.
Chau CA, Pan WH, Chen HJ. Employment status and temporal patterns of energy intake: Nutrition and Health Survey in Taiwan, 2005–2008. Public Health Nutr. 2017;20:3295–303.
Cheng Y, Yan H, Dibley MJ, Shen Y, Li Q, Zeng L. Validity and reproducibility of a semi-quantitative food frequency questionnaire for use among pregnant women in rural China. Asia Pac J Clin Nutr. 2008;17:166–77.
Global Fortification Data Exchange. Dashboard: Country Fortification. [Available from: http://www.fortificationdata.org.] (accessed on 1 May 2020).
Institute of Nutrition and Food Safety, China Center for Disease Control. China Food Composition Book 1. 2nd ed. Beijing: Peking University Medical Press; 2009.
Institute of Nutrition and Food Safety, China Center for Disease Control. China Food Composition Book 1. 2nd ed. Beijing: Peking University Medical Press; 2005.
Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–31S.
Li S, Liu D, Zhang R, Lei F, Liu X, Cheng Y, et al. The association of maternal dietary folate intake and folic acid supplementation with small-for-gestational-age births: a cross-sectional study in Northwest China. Br J Nutr. 2019;122:459–67.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Pei L, Kang Y, Zhao Y, Yan H. Prevalence and risk factors of congenital heart defects among live births: a population-based cross-sectional survey in Shaanxi province, Northwestern China. BMC Pediatrics. 2017;17:18.
Feng Y, Cai J, Tong X, Chen R, Zhu Y, Xu B, et al. Non-inheritable risk factors during pregnancy for congenital heart defects in offspring: A matched case-control study. Int J Cardiol. 2018;264:45–52.
Most J, Dervis S, Haman F, Adamo KB, Redman LM. Energy intake requirements in pregnancy. Nutrients. 2019;11:1812.
Caffrey A, McNulty H, Irwin RE, Walsh CP, Pentieva K. Maternal folate nutrition and offspring health: evidence and current controversies. Proc Nutr Soc. 2018;78:208–20.
Pufulete M, Emery PW, Sanders TA. Folate, DNA methylation and colo-rectal cancer. Proc Nutr Soc. 2003;62:437–45.
Chowdhury S, Cleves MA, MacLeod SL, James SJ, Zhao W, Hobbs CA. Maternal DNA hypomethylation and congenital heart defects. Birth Defects Res Part A Clin Mol Teratol. 2011;91:69–76.
Obeid R, Holzgreve W, Pietrzik K. Folate supplementation for prevention of congenital heart defects and low birth weight: an update. Cardiovasc Diagn Ther. 2019;9:S424–S33.
Boot MJ, Steegers-Theunissen RP, Poelmann RE, Van Iperen L, Lindemans J, Gittenberger-De Groot AC. Folic acid and homocysteine affect neural crest and neuroepithelial cell outgrowth and differentiation in vitro. Developmental Dyn. 2003;227:301–8.
Tierney BJ, Ho T, Reedy MV, Brauer PR. Homocysteine inhibits cardiac neural crest cell formation and morphogenesis in vivo. Developmental Dyn. 2004;229:63–73.
Bean LJH, Allen EG, Tinker SW, Hollis ND, Locke AE, Druschel C, et al. Lack of maternal folic acid supplementation is associated with heart defects in down syndrome: a report from the National Down Syndrome Project. Birth Defects Res Part A Clin Mol Teratol. 2011;91:885–93.
Li X, Li S, Mu D, Liu Z, Li Y, Lin Y, et al. The association between periconceptional folic acid supplementation and congenital heart defects: a case-control study in China. Prev Med. 2013;56:385–9.
Vereczkey A, Kosa Z, Csaky-Szunyogh M, Czeizel AE. Isolated atrioventricular canal defects: birth outcomes and risk factors: a population-based Hungarian case-control study, 1980-1996. Birth Defects Res Part A Clin Mol Teratol. 2013;97:217–24.
Scanlon KS, Ferencz C, Loffredo CA, Wilson PD, Correa-Villaseñor A, Khoury MJ, et al. Preconceptional folate intake and malformations of the cardiac outflow tract. Baltimore-Washington Infant Study Group. Epidemiol. 1998;9:95–8.
Tuokkola J, Luukkainen P, Kaila M, Takkinen HM, Niinistö S, Veijola R, et al. Maternal dietary folate, folic acid and vitamin D intakes during pregnancy and lactation and the risk of cows’ milk allergy in the offspring. Br J Nutr. 2016;116:710–8.
Barchitta M, Maugeri A, Magnano San Lio R, Favara G, La Mastra C, et al. Dietary Folate Intake and Folic Acid Supplements among Pregnant Women from Southern Italy: Evidence from the “Mamma & Bambino” Cohort. Int J Environ Res Public Health. 2020;17:638.
Czeizel AE, Dudás I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992;327:1832–5.
Czeizel AE. Reduction of urinary tract and cardiovascular defects by periconceptional multivitamin supplementation. Am J Med Genet. 1996;62:179–83.
Bosco JL, Tseng M, Spector LG, Olshan AF, Bunin GR. Reproducibility of reported nutrient intake and supplement use during a past pregnancy: a report from the Children’s Oncology Group. Paediatr Perinat Epidemiol. 2010;24:93–101.
Bunin GR, Gyllstrom ME, Brown JE, Kahn EB, Kushi LH. Recall of diet during a past pregnancy. Am J Epidemiol. 2001;154:1136–42.
Crozier SR, Robinson SM, Godfrey KM, Cooper C, Inskip HM. Women’s dietary patterns change little from before to during pregnancy. J Nutr. 2009;139:1956–63.
Rifas-Shiman SL, Rich-Edwards JW, Willett WC, Kleinman KP, Oken E, Gillman MW. Changes in dietary intake from the first to the second trimester of pregnancy. Paediatr Perinat Epidemiol. 2006;20:35–42.
Acknowledgements
We are grateful to all researchers and all participants in the 2014–2017 survey for their contribution to data collection.
Funding
This research was funded by the National Natural Science Foundation of China (81230016, 81202218, the Shaanxi Health and Family Planning Commission (Sxwsjswzfcght2016-013), and the National Key Research and Development Program of China (2017YF0907200, 2017YF0907201).
Author information
Authors and Affiliations
Contributions
RZ, LG, SD, and HY conceived and designed the study; RZ, LG, DZ, and PQ collected and cleared the data; RZ, LG and DZ analyzed and interpreted the data; RZ wrote the paper; LG, DZ, PQ, SD, and HY drafted and revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All subjects gave their written informed consent for inclusion before they participated in the study. The study was in accordance with the Helsinki Declaration, and the protocol was approved by the Ethics Committee of Xi’an Jiaotong University Health Science Center (Approval NO. 20120008).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, R., Guo, L., Zhao, D. et al. Maternal B-vitamin intake and B-vitamin supplementation during pregnancy in relation to neonatal congenital heart defects: a case-control study with propensity score matching. Eur J Clin Nutr 75, 782–791 (2021). https://doi.org/10.1038/s41430-020-00804-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00804-2