Abstract
Background
Taking folic acid supplementation could reduce the risk of neural tube defects for offspring in the maternal periconceptional period, but the relationship between folic acid use and other birth defects remains unclear, such as genitourinary system birth defects.
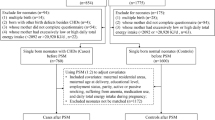
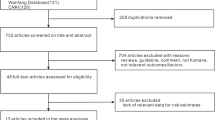
Methods
The data from a Prenatal Health Care System and Birth Defects Surveillance System in Tongzhou, Beijing, China, were collected from 2013 to 2018. We adjusted for differences in characteristics between comparison groups using propensity score inverse probability weighting and assessed associations with Poisson regression modeling.
Results
A total of 65,418 live births and stillbirths were included, and there were 194 cases with congenital genitourinary defects among them. The prevalence of genitourinary system birth defects was 29.2 (34.9) per 10,000 for FA/MMFA users (nonusers). Compared to nonusers, FA/MMFA users had a lower risk for genitourinary system birth defects (adjusted risk ratio [aRR] 0.81, 95% confidence interval [CI] 0.67, 0.98), and for hypospadias (aRR 0.55, 95% CI 0.40, 0.76).
Conclusions
FA or MMFA supplementation during the maternal periconceptional period could reduce the risk for genitourinary system birth defects in offspring. More mechanisms should be explored for the protective effect.
Impact
-
Folic acid (FA) or multiple micronutrients containing folic acid (MMFA) supplementation during the maternal periconceptional period could reduce the risk for genitourinary system birth defects in offspring.
-
Maternal FA/MMFA supplementation during the periconceptional period may reduce the risk for hypospadias.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Punjani, N. & Lamb, D. J. Male infertility and genitourinary birth defects: there is more than meets the eye. Fertil. Steril. 114, 209–218. (2020).
Ristoska-Bojkovska, N. Congenital anomalies of the kidney and urinary tract (CAKUT). Pril. (Makedon. Akad. Nauk Umet. Odd. Med Nauk.) 38, 59–62 (2017).
Mieusset, R. & Soulié, M. Hypospadias: psychosocial, sexual, and reproductive consequences in adult life. J. Androl. 26, 163–168 (2005).
Isert, S., Müller, D. & Thumfart, J. Factors associated with the development of chronic kidney disease in children with congenital anomalies of the kidney and urinary tract. Front. Pediatr. 8, 298 (2020).
Atala, A. Bioengineered tissues for urogenital repair in children. Pediatr. Res. 63, 569–575 (2008).
Gildestad, T. et al. Maternal use of folic acid and multivitamin supplements and infant risk of birth defects in Norway, 1999-2013. Br. J. Nutr. 124, 316–329. (2020).
Lamichhane, D. K. et al. Increased prevalence of some birth defects in Korea, 2009-2010. BMC Pregnancy Childbirth 16, 61 (2016).
Li, W. J. & Du, Z. W. Current status of birth defect monitoring system. Zhong Guo Fu You Wei Sheng Za Zhi 7, 63-66+83 (2016).
System CBDS. National Maternal and Child Health Surveillance and Annual Report Newsletter 3 (2021).
Zhang, W. et al. Analysis of the incidence of congenital renal malformations in Beijing from 2008 to 2014. Zhong Guo You Sheng Yu Yi Chuan Za Zhi 23, 74–77 (2015).
Xiao, W. X., Luan, Y. Q., Liu, Y. L., Song, C. H. & Chen, Y. J. Analysis of perinatal infants birth defects surveillance from 2011 to 2010 in Dongcheng District, Beijing. Zhong Guo You Sheng Yu Yi Chuan 24, 86–87 (2016).
Jia, B. L. Analysis of perinatal birth defects surveillance in Pinggu District, Beijing from 2013 to 2016. Zhong Guo Shi Yong Yi Yao. 12, 189–190 (2017).
van der Horst, H. J. & de Wall, L. L. Hypospadias, all there is to know. Eur. J. Pediatr. 176, 435–441. (2017).
Nicolaou, N., Renkema, K. Y., Bongers, E. M., Giles, R. H. & Knoers, N. V. Genetic, environmental, and epigenetic factors involved in CAKUT. Nat. Rev. Nephrol. 11, 720–731 (2015).
Glassberg, K. I. et al. Renal dysgenesis and cystic disease of the kidney: a report of the Committee on Terminology, Nomenclature and Classification, Section on Urology, American Academy of Pediatrics. J. Urol. 138, 1085–1092 (1987).
Chen, C. H. et al. Variants in ALX4 and their association with genitourinary defects. Andrology 8, 1243–1255. (2020).
Madariaga, L. et al. Severe prenatal renal anomalies associated with mutations in HNF1B or PAX2 genes. Clin. J. Am. Soc. Nephrol. 8, 1179–1187 (2013).
Ormond, G. et al. Endocrine disruptors in the workplace, hair spray, folate supplementation, and risk of hypospadias: case-control study. Environ. Health Perspect. 117, 303–307 (2009).
Rosenblum, S., Pal, A. & Reidy, K. Renal development in the fetus and premature infant. Semin. Fetal Neonatal Med. 22, 58–66 (2017).
Qin, X. Y. et al. Individual variation of the genetic response to bisphenol A in human foreskin fibroblast cells derived from cryptorchidism and hypospadias patients. PLoS One 7, e52756 (2012).
Tank, K. C. S. S., Pandya, A. M., Akbari, V. J. & Dangar, K. P. A study of histogenesis of human fetal kidney. Int. J. Biol. Med. Res. 3, 6 (2012).
Awazu, M. Structural and functional changes in the kidney caused by adverse fetal and neonatal environments. Mol. Biol. Rep. 49, 2335–2344. (2022).
Awazu, M. & Hida, M. Folic acid supplementation alleviates reduced ureteric branching, nephrogenesis, and global DNA methylation induced by maternal nutrient restriction in rat embryonic kidney. PLoS One 15, e0230289 (2020).
Blom, F., Bergman, J. E. & de Walle, H. E. Are congenital urinary tract and genital organ anomalies related to folic acid? Eur. Urol. 69, 544–546 (2016).
Pierik, F. H., Burdorf, A., Deddens, J. A., Juttmann, R. E. & Weber, R. F. Maternal and paternal risk factors for cryptorchidism and hypospadias: a case-control study in newborn boys. Environ. Health Perspect. 112, 1570–1576 (2004).
Groen In ‘t Woud, S. et al. Maternal risk factors involved in specific congenital anomalies of the kidney and urinary tract: a case-control study. Birth Defects Res. A Clin. Mol. Teratol. 106, 596–603 (2016).
Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. MRC Vitamin Study Research Group. Lancet 338, 131–137 (1991).
Ren, A. G. Prevention of neural tube defects with folic acid: The Chinese experience. World J. Clin. Pediatr. 4, 41–44 (2015).
Jin, L. et al. Maternal periconceptional folic acid supplementation and its effects on the prevalence of fetal neural tube defects. Bei Jing Da Xue Xue Bao Yi Xue Ban 52, 719–725 (2020).
Wang, C. et al. Prevalence of gestational diabetes mellitus and its determinants among pregnant women in Beijing. J. Matern. Fetal Neonatal Med. 35, 1337–1343. (2020).
Group TFASW. China Maternal and Child Health Association Guideline for the prevention of neural tube defects by periconceptional folic acid supplementation (2017). Zhong Guo Sheng Yu Jian Kang Za Zhi 28, 401–410 (2017).
Cong, J. et al. Evaluation of effect of different folic acid supplementation preparations on preventing birth defects: a cross-sectional study in Jiangsu province. Evid Based Complement Alternat Med. 2022, 7255331 (2022).
Newman, R. D., Parise, M. & Nahlen, B. Folic acid antagonists during pregnancy and risk of birth defects. N. Engl. J. Med. 344, 934–935 (2001).
Qu, P. F. et al. A propensity-matched study of the association between optimal folic acid supplementation and birth defects in Shaanxi province, Northwestern China. Sci. Rep. 9, 5271 (2019).
de Kort, C. A., Nieuwenhuijsen, M. J. & Mendez, M. A. Relationship between maternal dietary patterns and hypospadias. Paediatr. Perinat. Epidemiol. 25, 255–264 (2011).
Mavrogenis, S., Urban, R., Czeizel, A. E. & Ács, N. Possible preventive effect of high doses of folic acid for isolated hypospadias: a national population-based case-control study. Am. J. Med Genet A 164a, 3108–3114 (2014).
Arpino, C. et al. Teratogenic effects of antiepileptic drugs: use of an International Database on Malformations and Drug Exposure (MADRE). Epilepsia 41, 1436–1443 (2000).
Lindhout, D., Meinardi, H., Meijer, J. W. & Nau, H. Antiepileptic drugs and teratogenesis in two consecutive cohorts: changes in prescription policy paralleled by changes in pattern of malformations. Neurology 42, 94–110 (1992).
Carmichael, S. L., Yang, W., Correa, A., Olney, R. S. & Shaw, G. M. Hypospadias and intake of nutrients related to one-carbon metabolism. J. Urol. 181, 315–321 (2009).
Schreuder, M. F. Life with one kidney. Pediatr. Nephrol. 33, 595–604 (2018).
Sajjad, Y. Development of the genital ducts and external genitalia in the early human embryo. J. Obstet. Gynaecol. Res. 36, 929–937 (2010).
Baskin, L. S. & Ebbers, M. B. Hypospadias: anatomy, etiology, and technique. J. Pediatr. Surg. 41, 463–472 (2006).
Society for Maternal-Fetal Medicine (SMFM), Sparks, T. N. Hypospadias. Am. J. Obstet. Gynecol. 225, B18–B20 (2021).
Richard, M. A. et al. Altered mechanisms of genital development identified through integration of DNA methylation and genomic measures in hypospadias. Sci. Rep. 10, 12715 (2020).
Liew, S. C. Folic acid and diseases – supplement it or not? Rev. Assoc. Med. Bras. (1992). 62, 90–100 (2016).
Rampersaud, G. C., Kauwell, G. P., Hutson, A. D., Cerda, J. J. & Bailey, L. B. Genomic DNA methylation decreases in response to moderate folate depletion in elderly women. Am. J. Clin. Nutr. 72, 998–1003 (2000).
Källen, K. Maternal smoking and urinary organ malformations. Int. J. Epidemiol. 26, 571–574 (1997).
Funding
This study was supported by the National Key R&D Program of China, 2021YFC2701000 and 2021YFC2701001.
Author information
Authors and Affiliations
Contributions
L.J. and Z.P. conceptualized and designed the study, drafted the manuscript, performed the analysis and revised the manuscript critically for important intellectual content. L.J., J.Z. and W.M. contributed to the acquisition and interpretation of data and revised it critically for important intellectual content. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the biomedical ethics committee of Peking University (no. IRB00001052-18010). Informed consent of all participants is exempted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pang, Z., Jin, L., Zhang, J. et al. Maternal periconceptional folic acid supplementation and risk for fetal congenital genitourinary system defects. Pediatr Res 95, 1132–1138 (2024). https://doi.org/10.1038/s41390-023-02808-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02808-7