Abstract
Background/objectives
Evidence is lacking on how variation in vitamin D concentrations during gestation affects perinatal outcomes. Therefore, we evaluated the association between vitamin D serum concentrations during pregnancy and neonatal outcomes.
Methods
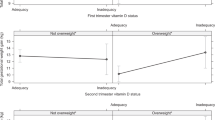
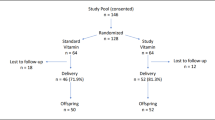
A prospective cohort of 180 healthy Brazilian pregnant women was followed and plasma 25-hydroxyvitamin [25(OH)D, nmol/L] was measured at 5–13 (baseline), 20–26 and 30–36 gestational weeks. Birth weight (BW), birth length (BL), BW z-scores, BL z-scores, first minute Apgar, small for gestational age (SGA), large for gestational age (LGA) and preterm birth were the outcomes. Multiple linear and Poisson regression models were estimated. Best linear unbiased prediction of random coefficients model was used to determine the association between the mean rate of change in vitamin D during pregnancy concentrations and neonatal outcomes.
Results
Mean (SD) BW was 3300 (600) g, BW z-score 0.34 (1.11), BL 49.3 (3.3) cm, BL z-score 0.44 (1.5), and first minute Apgar score 8.2 (1.4). Prevalence of SGA, LGA and preterm birth were 6%, 18% and 13%, respectively. 25(OH)D was directly associated with the risk of preterm birth at all trimesters. Incidence-rate ratios were 1.02, 1.05 and 1.04 for the 1st, 2nd and 3rd trimester, respectively. Mean rate of change during pregnancy in 25(OH)D was directly associated with BW z-score (β: 0.36, 95% CI 0.07; 0.65), LGA risk (IRR: 1.97, 95% CI 1.07; 3.63) and preterm birth (IRR: 7.35, 95% CI 2.99; 18.07).
Conclusions
Mean 25(OH)D rate of change during pregnancy was directly associated with BW z-scores, and increased LGA and preterm birth risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Barker DJ. The origins of the developmental origins theory. J Intern Med. 2007;261:412–7.
Savchev S, Sanz-Cortes M, Cruz-Martinez R, Arranz A, Botet F, Gratacos E, et al. Neurodevelopmental outcome of full-term small-for-gestational-age infants with normal placental function. Ultrasound Obstet Gynecol. 2013;42:201–6.
Platt MJ. Outcomes in preterm infants. Public Health. 2014;128:399–403.
Kleiser C, Schaffrath Rosario A, Mensink GB, Prinz-Langenohl R, Kurth BM. Potential determinants of obesity among children and adolescents in Germany: results from the cross-sectional KiGGS Study. BMC Public Health. 2009;9:46.
de Jong F, Monuteaux MC, van Elburg RM, Gillman MW, Belfort MB. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension. 2012;59:226–34.
Nam HK, Lee KH. Small for gestational age and obesity: epidemiology and general risks. Ann Pediatr Endocrinol Metab. 2018;23:9–13.
Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7:e37–46.
Blencowe H, Krasevec J, de Onis M, Black RE, An X, Stevens GA, et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2019;7:e849–60.
Lee AC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1:e26–36.
Frey HA, Klebanoff MA. The epidemiology, etiology, and costs of preterm birth. Semin Fetal Neonatal Med. 2016;21:68–73.
McCowan L, Horgan RP. Risk factors for small for gestational age infants. Best Pr Res Clin Obstet Gynaecol. 2009;23:779–93.
Triunfo S, Lanzone A, Lindqvist PG. Low maternal circulating levels of vitamin D as potential determinant in the development of gestational diabetes mellitus. J Endocrinol Investig. 2017;40:1049–59.
Mannion CA, Gray-Donald K, Koski KG. Association of low intake of milk and vitamin D during pregnancy with decreased birth weight. CMAJ. 2006;174:1273–7.
Francis EC, Hinkle SN, Song Y, Rawal S, Donnelly SR, Zhu Y, et al. Longitudinal maternal vitamin D status during pregnancy is associated with neonatal anthropometric measures. Nutrients. 2018;10:1631.
Bilic M, Qamar H, Onoyovwi A, Korsiak J, Papp E, Al Mahmud A, et al. Prenatal vitamin D and cord blood insulin-like growth factors in Dhaka, Bangladesh. Endocr Connect. 2019;8:745–53.
Wagner CL, Taylor SN, Johnson DD, Hollis BW. The role of vitamin D in pregnancy and lactation: emerging concepts. Women’s Health. 2012;8:323–40.
Agudelo-Zapata Y, Maldonado-Acosta LM, Sandoval-Alzate HF, Poveda NE, Garcés MF, Cortés-Vásquez JA, et al. Serum 25-hydroxyvitamin D levels throughout pregnancy: a longitudinal study in healthy and preeclamptic pregnant women. Endocr Connect. 2018;7:698–707.
Figueiredo AC, Cocate PG, Adegboye AR, Franco-Sena AB, Farias DR, de Castro MB, et al. Changes in plasma concentrations of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D during pregnancy: a Brazilian cohort. Eur J Nutr. 2017;57:1059–72.
Brannon PM, Picciano MF. Vitamin D in pregnancy and lactation in humans. Annu Rev Nutr. 2011;31:89–115.
Tous M, Villalobos M, Iglesias L, Fernández-Barrés S, Arija V. Vitamin D status during pregnancy and offspring outcomes: a systematic review and meta-analysis of observational studies. Eur J Clin Nutr. 2019;74:36–53.
Amegah AK, Klevor MK, Wagner CL. Maternal vitamin D insufficiency and risk of adverse pregnancy and birth outcomes: a systematic review and meta-analysis of longitudinal studies. PLoS ONE. 2017;12:e0173605.
van der Pligt P, Willcox J, Szymlek-Gay EA, Murray E, Worsley A, Daly RM. Associations of maternal vitamin D deficiency with pregnancy and neonatal complications in developing countries: a systematic review. Nutrients. 2018;10:640.
Kelishadi R, Sharifi-Ghazvini F, Poursafa P, Mehrabian F, Farajian S, Yousefy H, et al. Determinants of hypovitaminosis D in pregnant women and their newborns in a sunny region. Int J Endocrinol. 2013;2013:460970.
Pereira-Santos M, Carvalho GQ, Couto RD, Dos Santos DB, Oliveira AM. Vitamin D deficiency and associated factors among pregnant women of a sunny city in Northeast of Brazil. Clin Nutr Espen. 2018;23:240–4.
Bouillon R. Comparative analysis of nutritional guidelines for vitamin D. Nat Rev Endocrinol. 2017;13:466–79.
Karras SN, Fakhoury H, Muscogiuri G, Grant WB, van den Ouweland JM, Colao AM, et al. Maternal vitamin D levels during pregnancy and neonatal health: evidence to date and clinical implications. Ther Adv Musculoskelet Dis. 2016;8:124–35.
Wagner CL, Hollis BW. The implications of vitamin D dtatus during pregnancy on mother and her developing child. Front Endocrinol. 2018;9:500.
Chan SY, Susarla R, Canovas D, Vasilopoulou E, Ohizua O, McCabe CJ, et al. Vitamin D promotes human extravillous trophoblast invasion in vitro. Placenta. 2015;36:403–9.
Liu NQ, Larner DP, Yao Q, Chun RF, Ouyang Y, Zhou R, et al. Vitamin D-deficiency and sex-specific dysregulation of placental inflammation. J Steroid Biochem Mol Biol. 2018;177:223–30.
El-Khoury JM, Reineks EZ, Wang S. Progress of liquid chromatography-mass spectrometry in measurement of vitamin D metabolites and analogues. Clin Biochem. 2011;44:66–76.
Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, et al. Prevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90:3215–24.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Gordon CC, Chumlea WC, Roche AF. Stature, recumbent length, and weight. Anthropometric standardization reference manual. Champaign: Human kinetics Books; 1988. pp. 3–8.
Giacomello A, Schmidt MI, Nunes MAA, Duncan BB, Soares RM, Manzolli P, et al. Validation of a food frequency questionnaire conducted among pregnant women attended by the Brazilian National Health Service, in two municipalities of the State of Rio Grande do Sul, Brazil. Rev Brasileira de Saúde Matern Infant. 2008;8:445–54.
Sichieri R, Everhart J. Validity of a Brazilian food frequency questionnaire against dietary recalls and estimated energy intake. Nutr Res. 1998;18:1649–59.
(US) IoM. Committee to review dietary reference intakes for vitamin D and calcium: dietary reference intakes for calcium and vitamin D. In: Ross ACTC, Yaktine AL, Del Valle HB, editors. Washington (DC) US: National Academies Press; 2011.
Chen YH, Ferguson KK, Meeker JD, McElrath TF, Mukherjee B. Statistical methods for modeling repeated measures of maternal environmental exposure biomarkers during pregnancy in association with preterm birth. Environ Health. 2015;14:9.
Glymor MM, Greenland S. Causal diagrams. In: TL RKGSL, editor. Modern epidemiology. Philadelphia: Lippincott Williams & Wilkins; 2008. pp. 183–209.
Textor J, Hardt J, Knüppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745.
StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017.
Kale PL, Lordelo CVM, Fonseca SC, Silva KS, Lobato JCP, Costa AJL, et al. Adequação do peso ao nascer para idade gestacional de acordo com a curva INTERGROWTH-21 st e fatores associados ao pequeno para idade gestacional. Cad Saúde Coletiva. 2018;26:391–9.
Francis A, Hugh O, Gardosi J. Customized vs INTERGROWTH-21. Am J Obstet Gynecol. 2018;218:S692–9.
Pereira-Santos M, Carvalho GQ, Dos Santos DB, Oliveira AM. Influence of vitamin D serum concentration, prenatal care and social determinants on birth weight: a northeastern Brazilian cohort study. Br J Nutr. 2019;122:284–92.
Nobles CJ, Markenson G, Chasan-Taber L. Early pregnancy vitamin D status and risk for adverse maternal and infant outcomes in a bi-ethnic cohort: the Behaviors Affecting Baby and You (B.A.B.Y.) Study. Br J Nut.r 2015;114:2116–28.
Lapillonne A. Vitamin D deficiency during pregnancy may impair maternal and fetal outcomes. Med Hypotheses. 2010;74:71–5.
Shin JS, Choi MY, Longtine MS, Nelson DM. Vitamin D effects on pregnancy and the placenta. Placenta. 2010;31:1027–34.
Møller UK, Streym S, Heickendorff L, Mosekilde L, Rejnmark L. Effects of 25OHD concentrations on chances of pregnancy and pregnancy outcomes: a cohort study in healthy Danish women. Eur J Clin Nutr. 2012;66:862–8.
Zhou J, Su L, Liu M, Liu Y, Cao X, Wang Z, et al. Associations between 25-hydroxyvitamin D levels and pregnancy outcomes: a prospective observational study in southern China. Eur J Clin Nutr. 2014;68:925–30.
Fernández-Alonso AM, Dionis-Sánchez EC, Chedraui P, González-Salmerón MD, Pérez-López FR. Group SVDaWsHR. First-trimester maternal serum 25-hydroxyvitamin D3 status and pregnancy outcome. Int J Gynaecol Obstet. 2012;116:6–9.
Bärebring L, Bullarbo M, Glantz A, Leu Agelii M, Jagner Å, Ellis J, et al. Preeclampsia and blood pressure trajectory during pregnancy in relation to vitamin D status. PLoS ONE. 2016;11:e0152198.
Kassai MS, Cafeo FR, Affonso-Kaufman FA, Suano-Souza FI, Sarni ROS. Vitamin D plasma concentrations in pregnant women and their preterm newborns. BMC Pregnancy Childbirth. 2018;18:412.
Qin LL, Lu FG, Yang SH, Xu HL, Luo BA. Does maternal vitamin D deficiency increase the risk of preterm birth: a meta-analysis of observational studies. Nutrients. 2016;8:301.
McDonnell SL, Baggerly KA, Baggerly CA, Aliano JL, French CB, Baggerly LL, et al. Maternal 25(OH)D concentrations ≥40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PLoS ONE. 2017;12:e0180483.
Romero R, Espinoza J, Gonçalves LF, Kusanovic JP, Friel L, Hassan S. The role of inflammation and infection in preterm birth. Semin Reprod Med 2007;25:21–39.
Hewison M. Antibacterial effects of vitamin D. Nat Rev Endocrinol. 2011;7:337–45.
Liu NQ, Hewison M. Vitamin D, the placenta and pregnancy. Arch Biochem Biophys. 2012;523:37–47.
Al-Shaikh GK, Ibrahim GH, Fayed AA, Al-Mandeel H. Impact of vitamin D deficiency on maternal and birth outcomes in the Saudi population: a cross-sectional study. BMC Pregnancy Childbirth. 2016;16:119.
Viellas EF, Domingues RMSM, Dias MAB, et al. Assistência pré-natal no Brasil. Cad de Saúde Pública. 2014;30:S85–100.
Moon RJ, Harvey NC, Cooper C, D’Angelo S, Curtis EM, Crozier SR, et al. Response to antenatal cholecalciferol supplementation is associated with common vitamin D-related genetic variants. J Clin Endocrinol Metab. 2017;102:2941–9.
Acknowledgements
The authors are grateful to all the women who volunteered to participate in this cohort study, to the managers and professionals of the Municipal Health Centre Heitor Beltrão for providing us with the space and opportunities for the data collection and to the Quest Diagnostics Nichols Institute laboratory (San Juan Capistrano, CA, USA) for performing the vitamin D concentration analyses. Moreover, we thank the National Council for Scientific and Technological Development (CNPq in the Portuguese acronym; grant number: 471196/2010-0) and the Carlos Chagas Filho Foundation for Research Support of Rio de Janeiro State (FAPERJ for the Portuguese acronym, grant number E-26/111.400/2010, E_14/2010) for the financial support. National Council for Scientific and Technological Development (CNPq in the Portuguese acronym; grant number: 471196/2010-0) and the Carlos Chagas Filho Foundation for Research Support of Rio de Janeiro State (FAPERJ in the Portuguese acronym, grant number E-26/111.400/2010, E_14/2010).
Author information
Authors and Affiliations
Contributions
CB and GK developed the research question and designed the study. CB and TRBC conducted the statistical analyses. GK, TRBC and DF provided support for the statistical analyses. TRBC assisted with the literature review and with writing the manuscript. All of the authors have made substantial contributions to the manuscript and approved this final revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The current study was performed in accordance with the guidelines of the Declaration of Helsinki. An informed consent for participation was thoroughly explained and signed by all participants. This study was approved by the Rio de Janeiro Federal University Maternity Teaching Hospital Ethics Committee (protocol number: 0023.0.361.000-08) and the Municipal Secretary of Rio de Janeiro Ethics Committee (protocol number: 0139.0.314.000-09).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benaim, C., Carrilho, T.R.B., Farias, D.R. et al. Vitamin D during pregnancy and its association with birth outcomes: a Brazilian cohort study. Eur J Clin Nutr 75, 489–500 (2021). https://doi.org/10.1038/s41430-020-00733-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00733-0