Abstract
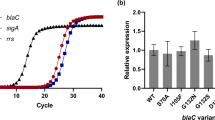
Tunicamycins (TUN) are well-defined, Streptomyces-derived natural products that inhibit protein N-glycosylation in eukaryotes, and by a conserved mechanism also block bacterial cell wall biosynthesis. TUN inhibits the polyprenylphosphate-N-acetyl-hexosamine-1-phospho-transferases (PNPT), an essential family of enzymes found in both bacteria and eukaryotes. We have previously published the development of chemically modified TUN, called TunR1 and TunR2, that have considerably reduced activity on eukaryotes but that retain the potent antibacterial properties. A mechanism for this reduced toxicity has also been reported. TunR1 and TunR2 have been tested against mammalian cell lines in culture and against live insect cells but, until now, no in vivo evaluation has been undertaken for vertebrates. In the current work, TUN, TunR1, and TunR2 are investigated for their relative toxicity and antimycobacterial activity in zebrafish using a well-established Mycobacterium marinum (M. marinum) infection system, a model for studying human Mycobacterium tuberculosis infections. We also report the relative ability to activate the unfolded protein response (UPR), the known mechanism for the eukaryotic toxicity observed with TUN treatment. Importantly, TunR1 and TunR2 retained their antimicrobial properties, as evidenced by a reduction in M. marinum bacterial burden, compared to DMSO-treated zebrafish. In summary, findings from this study highlight the characteristics of recently developed TUN derivatives, mainly TunR2, and its potential for use as a novel anti-bacterial agent for veterinary and potential medical purposes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
CDC. Centers for Disease Control and Prevention. 2022 [cited 2022 Sep 5]. The biggest antibiotic-resistant threats in the U.S. Available from: https://www.cdc.gov/drugresistance/biggest-threats.html
Sekhri L, Kadri ML, Samira C, Senigra M. Synthesis of penicillin derivatives and study of their biological antibacterial activities. Biomed Pharm J. 2015;1:257–64.
Pan X, He Y, Chen T, Chan KF, Zhao Y. Modified Penicillin Molecule with Carbapenem-Like Stereochemistry Specifically Inhibits Class C β-Lactamases. Antimicrob Agents Chemother. 2017;61:e01288–17.
Zhu X, Liu D, Singh AK, Drolia R, Bai X, Tenguria S, et al. Tunicamycin Mediated Inhibition of Wall Teichoic Acid Affects Staphylococcus aureus and Listeria monocytogenes Cell Morphology, Biofilm Formation and Virulence. Front Microbiol. 2018;9:1352.
Huszár S, Singh V, Polčicová A, Baráth P, Barrio MB, Lagrange S, et al. N-Acetylglucosamine-1-Phosphate Transferase, WecA, as a Validated Drug Target in Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2017;61:e01310–17.
Cundell DR, Tuomanen EI. Receptor specificity of adherence of Streptococcus pneumoniae to human type-II pneumocytes and vascular endothelial cells in vitro. Micro Pathog. 1994;17:361–74.
Cantagrel V, Lefeber DJ. From glycosylation disorders to dolichol biosynthesis defects: a new class of metabolic diseases. J Inherit Metab Dis. 2011;34:859–67.
Eichler J, Imperiali B. Biogenesis of Asparagine-Linked Glycoproteins Across Domains of Life—Similarities and Differences. ACS Chem Biol. 2018;13:833–7. https://pubs.acs.org/doi/pdf/10.1021/acschembio.8b00163
Lehle L, Strahl S, Tanner W. Protein Glycosylation, Conserved from Yeast to Man: A Model Organism Helps Elucidate Congenital Human Diseases. Angew Chem Int Ed. 2006;45:6802–18.
Bugg TDH, Kerr RV. Mechanism of action of nucleoside antibacterial natural product antibiotics. J Antibiot (Tokyo). 2019;72:865–76.
Shan L, Wenling Q, Mauro P, Stefano B. Antibacterial Agents Targeting the Bacterial Cell Wall. Curr Med Chem. 2020;27:2902–26.
Schröder M, Kaufman RJ. ER stress and the unfolded protein response. Mutat Res Mol Mech Mutagen. 2005;569:29–63.
Abdullahi A, Stanojcic M, Parousis A, Patsouris D, Jeschke MG. Modeling Acute ER stress in vivo and in vitro. Shock Augusta Ga. 2017;47:506–13.
Tkacz JS, Lampen O. Tunicamycin inhibition of polyisoprenyl N-acetylglucosaminyl pyrophosphate formation in calf-liver microsomes. Biochem Biophys Res Commun. 1975;65:248–57.
Price NPJ, Jackson MA, Singh V, Hartman TM, Blackburn JA, Dowd PF. Synergistic enhancement of beta-lactam antibiotics by modified tunicamycin analogs TunR1 and TunR2. J Antibiot (Tokyo). 2019;72:807–15.
Price NP, Hartman TM, Li J, Velpula KK, Naumann TA, Guda MR, et al. Modified tunicamycins with reduced eukaryotic toxicity that enhance the antibacterial activity of β-lactams. J Antibiot (Tokyo). 2017;70:1070–7.
Dong YY, Wang H, Pike ACW, Cochrane SA, Hamedzadeh S, Wyszyński FJ, et al. Structures of DPAGT1 Explain Glycosylation Disease Mechanisms and Advance TB Antibiotic Design. Cell. 2018;175:1045–e16.
Mitachi K, Mingle D, Effah W, Sánchez-Ruiz A, Hevener KE, Narayanan R, et al. Concise Synthesis of Tunicamycin V and Discovery of a Cytostatic DPAGT1 Inhibitor. Angew Chem Int Ed. 2022;61:e202203225.
Hakulinen JK, Hering J, Brändén G, Chen H, Snijder A, Ek M, et al. MraY-antibiotic complex reveals details of tunicamycin mode of action. Nat Chem Biol. 2017;13:265–7.
Yoo J, Mashalidis EH, Kuk ACY, Yamamoto K, Kaeser B, Ichikawa S, et al. GlcNAc-1-P-transferase–tunicamycin complex structure reveals basis for inhibition of N-glycosylation. Nat Struct Mol Biol. 2018;25:217–24.
Mashalidis EH, Lee SY. Structures of bacterial MraY and human GPT provide insights into rational antibiotic design. J Mol Biol. 2020;432:4946–63.
Hering J, Dunevall E, Snijder A, Eriksson PO, Jackson MA, Hartman TM, et al. Exploring the Active Site of the Antibacterial Target MraY by Modified Tunicamycins. ACS Chem Biol. 2020;15:2885–95.
Takaki K, Davis JM, Winglee K, Ramakrishnan L. Evaluation of the pathogenesis and treatment of Mycobacterium marinum infection in zebrafish. Nat Protoc. 2013;8:1114–24.
Tobin DM, Ramakrishnan L. Comparative pathogenesis of Mycobacterium marinum and Mycobacterium tuberculosis. Cell Microbiol. 2008;10:1027–39.
Sridevi JP, Anantaraju HS, Kulkarni P, Yogeeswari P, Sriram D. Optimization and validation of Mycobacterium marinum-induced adult zebrafish model for evaluation of oral anti-tuberculosis drugs. Int J Mycobacteriol. 2014;3:259–67.
Davis JM, Clay H, Lewis JL, Ghori N, Herbomel P, Ramakrishnan L. Real-Time Visualization of Mycobacterium-Macrophage Interactions Leading to Initiation of Granuloma Formation in Zebrafish Embryos. Immunity. 2002;17:693–702.
Clark EM, Nonarath HJT, Bostrom JR, Link BA. Establishment and validation of an endoplasmic reticulum stress reporter to monitor zebrafish ATF6 activity in development and disease. Dis Model Mech. 2020;13:dmm041426.
Ellett F, Pase L, Hayman JW, Andrianopoulos A, Lieschke GJ. mpeg1 promoter transgenes direct macrophage-lineage expression in zebrafish. Blood. 2011;117:e49.
Matty MA, Knudsen DR, Walton EM, Beerman RW, Cronan MR, Pyle CJ, et al. Potentiation of P2RX7 as a host-directed strategy for control of mycobacterial infection. Garrett WS, Kana BD, Barczak A, editors. eLife. 2019;8:e39123.
Price NP, Labeda DP, Naumann TA, Vermillion KE, Bowman MJ, Berhow MA, et al. Quinovosamycins: new tunicamycin-type antibiotics in which the α, β-1″,11′-linked N-acetylglucosamine residue is replaced by N-acetylquinovosamine. J Antibiot (Tokyo). 2016;69:637–46.
Bookstaver PB, Bland CM, Griffin B, Stover KR, Eiland LS, McLaughlin M. A Review of Antibiotic Use in Pregnancy. Pharmacotherapy. 2015;35:1052–62.
Nakanishi K, Sudo T, Morishima N. Endoplasmic reticulum stress signaling transmitted by ATF6 mediates apoptosis during muscle development. J Cell Biol. 2005;169:555–60.
Wang X, Karamariti E, Simpson R, Wang W, Xu Q. Dickkopf Homolog 3 Induces Stem Cell Differentiation into Smooth Muscle Lineage via ATF6 Signalling. J Biol Chem. 2015;290:19844–52.
Habjan E, Ho VQT, Gallant J, van Stempvoort G, Jim KK, Kuijl C, et al. An anti-tuberculosis compound screen using a zebrafish infection model identifies an aspartyl-tRNA synthetase inhibitor. Dis Model Mech. 2021;14:dmm049145.
Dalton JP, Uy B, Okuda KS, Hall CJ, Denny WA, Crosier PS, et al. Screening of anti-mycobacterial compounds in a naturally infected zebrafish larvae model. J Antimicrob Chemother. 2017;72:421–7.
Demain AL. Antibiotics: Natural products essential to human health. Med Res Rev. 2009;29:821–42.
Cinaroglu A, Gao C, Imrie D, Sadler KC. Atf6 plays protective and pathologic roles in fatty liver disease due to endoplasmic reticulum stress. Hepatol Balt Md. 2011;54:495–508.
Li J, Chen Z, Gao LY, Colorni A, Ucko M, Fang S, et al. A transgenic zebrafish model for monitoring xbp1 splicing and endoplasmic reticulum stress in vivo. Mech Dev. 2015;137:33–44.
Yeh KY, Lai CY, Lin CY, Hsu CC, Lo CP, Her GM. ATF4 overexpression induces early onset of hyperlipidaemia and hepatic steatosis and enhances adipogenesis in zebrafish. Sci Rep. 2017;7:16362.
Kenyon S, Pike K, Jones DR, Brocklehurst P, Marlow N, Salt A, et al. Childhood outcomes after prescription of antibiotics to pregnant women with spontaneous preterm labour: 7-year follow-up of the ORACLE II trial. Lancet Lond Engl. 2008;372:1319–27.
Qiu W, Fang M, Magnuson JT, Greer JB, Chen Q, Zheng Y, et al. Maternal exposure to environmental antibiotic mixture during gravid period predicts gastrointestinal effects in zebrafish offspring. J Hazard Mater. 2020;399:123009.
Bengmark S, Göransson G, Zoucas E. Defects in hemostasis produced by antibiotics. An in vivo study in the rat. Eur Surg Res Eur Chir Forsch Rech Chir Eur. 1981;13:290–8.
Ailes EC, Gilboa SM, Gill SK, Broussard CS, Crider KS, Berry RJ, et al. Association between antibiotic use among pregnant women with urinary tract infections in the first trimester and birth defects, National Birth Defects Prevention Study 1997 to 2011. Birth Defects Res A Clin Mol Teratol. 2016;106:940–9.
Hoyberghs J, Bars C, Ayuso M, Van Ginneken C, Foubert K, Van Cruchten S. DMSO Concentrations up to 1% are Safe to be Used in the Zebrafish Embryo Developmental Toxicity Assay. Front Toxicol. 2021;3:804033.
Maes J, Verlooy L, Buenafe OE, Witte PAM, de, Esguerra CV, Crawford AD. Evaluation of 14 Organic Solvents and Carriers for Screening Applications in Zebrafish Embryos and Larvae. PLOS ONE. 2012;7:e43850.
Thuning CA, Fanshaw MS, Warren J. Mechanisms of the synergistic effect of oral dimethyl sulfoxide on antineoplastic therapy. Ann N. Y Acad Sci. 1983;411:150–60.
Christou M, Kavaliauskis A, Ropstad E, Fraser TWK. DMSO effects larval zebrafish (Danio rerio) behavior, with additive and interaction effects when combined with positive controls. Sci Total Environ. 2020;709:134490.
Kim K, Lee SE. Combined toxicity of dimethyl sulfoxide (DMSO) and vanadium towards zebrafish embryos (Danio rerio): Unexpected synergistic effect by DMSO. Chemosphere. 2021;270:129405.
Uribe PM, Mueller MA, Gleichman JS, Kramer MD, Wang Q, Sibrian-Vazquez M, et al. Dimethyl Sulfoxide (DMSO) Exacerbates Cisplatin-induced Sensory Hair Cell Death in Zebrafish (Danio rerio). PLoS. 2013;8:e55359. https://dspace.mit.edu/handle/1721.1/78920
Acknowledgements
This work was supported in part by the U.S. Department of Agriculture, Agricultural Research Service (N.P.J.P. and M.A.J.), and by Eminent Scholar funds from the Medical College of Wisconsin (B.A.L). T.C.Z. was supported by the National Institute of Allergy and Infectious Diseases (5R21AI144225-02). We acknowledge C. Skory (NCAUR-ARS, Peoria, IL) and J. Bannantine (NADC-ARS, Ames, IA) for helpful discussion and suggestions on the preparation of this manuscript. We thank T. Hartman for expert technical support and David M. Tobin (Duke University) for sharing reagents. Finally we acknowledge the use of BioRender for the generation of diagrams used in this manuscript. Mention of trade names or commercial products in this article is solely for the purpose of providing scientific information and does not imply recommendation or endorsement by the U.S. Department of Agriculture. USDA is an equal opportunity provider and employer.
Author information
Authors and Affiliations
Contributions
The manuscript was written through the contributions of all authors. All authors have given approval to the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nonarath, H.J.T., Jackson, M.A., Penoske, R.M. et al. The tunicamycin derivative TunR2 exhibits potent antibiotic properties with low toxicity in an in vivo Mycobacterium marinum-zebrafish TB infection model. J Antibiot 77, 245–256 (2024). https://doi.org/10.1038/s41429-023-00694-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-023-00694-z