Abstract
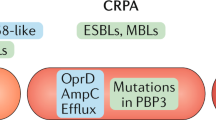
Although the development of resistance by microorganisms to antimicrobial drugs has been recognized as a global public health concern, the contribution of various non-antibiotic antimicrobial agents to the development of antimicrobial resistance (AMR) remains largely neglected. The present review discusses various chemical substances and factors other than typical antibiotics, such as preservatives, disinfectants, biocides, heavy metals and improper chemical sterilization that contribute to the development of AMR. Furthermore, it encompasses the mechanisms like co-resistance and co-selection, horizontal gene transfer, changes in the composition and permeability of cell membrane, efflux pumps, transposons, biofilm formation and enzymatic degradation of antimicrobial chemicals which underlie the development of resistance to various non-antibiotic antimicrobial agents. In addition, the review addresses the resistance-associated changes that develops in microorganisms due to these agents, which ultimately contribute to the development of resistance to antibiotics. In order to prevent the indiscriminate use of chemical substances and create novel therapeutic agents to halt resistance development, a more holistic scientific approach might provide diversified views on crucial factors contributing to the persistence and spread of AMR. The review illustrates the common and less explored mechanisms contributing directly or indirectly to the development of AMR by non-antimicrobial agents that are commonly used.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Davies J. Origins and evolution of antibiotic resistance. Microbiolía. 1996;12:9–16. https://doi.org/10.1128/mmbr.00016-10.
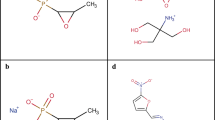
Cen T, Zhang X, Xie S, Li D. Preservatives accelerate the horizontal transfer of plasmid-mediated antimicrobial resistance genes via differential mechanisms. Environ Int. 2020;138:1–9.
Rehman K, Fatima F, Waheed I, Akash MSH. Prevalence of exposure of heavy metals and their impact on health consequences. J Cell Biochem. 2018;119:157–84.
Wales AD, Davies RH. Co-selection of resistance to antibiotics, biocides and heavy metals, and its relevance to foodborne pathogens. Antibiotics. 2015;4:567–604. https://doi.org/10.3390/antibiotics4040567.
Alderton I, et al. The role of emerging organic contaminants in the development of antimicrobial resistance. Emerg Contam. 2021;7:160–71. https://doi.org/10.1016/j.emcon.2021.07.001.
Maillard J-Y. Resistance of bacteria to biocides. Microbiol Spectr. 2018;6:1–17.
Tekleab AM, Asfaw Y, Weldetsadik A, Amaru GM. Antibiotic prescribing practice in the management of cough or diarrhea among children attending hospitals in Addis Ababa: a cross-sectional study. Pediatr Health Med Ther. 2017;8:93–98.
Andersson DI, Hughes D. Selection and transmission of antibiotic-resistant bacteria. Microbiol Spectr. 2017;5:1–17.
Fernández L, Hancock REW. Adaptive and mutational resistance: role of porins and efflux pumps in drug resistance. Clin Microbiol Rev. 2012;25:661–81.
Huemer M, Mairpady Shambat S, Brugger SD, Zinkernagel AS. Antibiotic resistance and persistence—implications for human health and treatment perspectives. EMBO Rep. 2020;21:e51034.
Chen J, et al. Lack of antibiotic knowledge and misuse of antibiotics by medical students in Mali: a cross-sectional study. Expert Rev Anti Infect Ther. 2021;19:797–804.
Maillard J. Impact of benzalkonium chloride, benzethonium chloride and chloroxylenol on bacterial antimicrobial resistance. J Appl Microbiol. 2022. https://doi.org/10.1111/jam.15739.
Dhama K, et al. The role of disinfectants and sanitizers during COVID-19 pandemic: advantages and deleterious effects on humans and the environment. Environ Sci Pollut Res. 2021;28:34211–28.
Pereira BMP, Tagkopoulos I. Benzalkonium chlorides: uses, regulatory status, and microbial resistance. Appl Environ Microbiol. 2019;85. https://doi.org/10.1128/AEM.00377-19.
Kim M, et al. Widely used benzalkonium chloride disinfectants can promote antibiotic resistance. Appl Environ Microbiol. 2018;84:e01201–18. https://journals.asm.org/journal/aem.
Adair FW, Liauw H-L, Geftic SG, Gelzer J. Reduced virulence of pseudomonas aeruginosa grown in the presence of benzalkonium chloride. J Clin Microbiol. 1975;1:175–9.
Qian Y, et al. Biological synergy and antimicrobial mechanism of hydroxypropyltrimethyl ammonium chloride chitosan with benzalkonium chloride. Chem Pharm Bull. 2021;69:612–9.
Xu D, et al. Benzalkonium chloride and heavy-metal tolerance in Listeria monocytogenes from retail foods. Int J Food Microbiol. 2014;190:24–30.
Hoffmann H-P, Geftic SG, Gelzer J, Heymann H, Adair FW. Ultrastructural alterations associated with the growth of resistant Pseudomonas aeruginosa in the presence of benzalkonium chloride. J Bacteriol. 1973;113:409–16.
Kampf G. Adaptive microbial response to low-level benzalkonium chloride exposure. J Hospital Infect. 2018;100:e1–e22. https://doi.org/10.1016/j.jhin.2018.05.019.
Adair FW, Geftic SG, Gelzer J. Resistance of pseudomonas to quaternary ammonium compounds I. Growth in benzalkonium chloride solution. Appl Microbiol. 1969;18:299–302.
Kim M, et al. Genomic and transcriptomic insights into how bacteria withstand high concentrations of benzalkonium chloride biocides. Appl Environ Microbiol. 2018;84:e00197–18.
El-Banna T, Abd El-Aziz A, Sonbol F, El-Ekhnawy E. Adaptation of Pseudomonas aeruginosa clinical isolates to benzalkonium chloride retards its growth and enhances biofilm production. Mol Biol Rep. 2019;46:3437–43.
Nordholt N, Kanaris O, Schmidt SBI, Schreiber F. Persistence against benzalkonium chloride promotes rapid evolution of tolerance during periodic disinfection. Nat Commun. 2021;12:1–13.
Short FL, et al. Benzalkonium chloride antagonises aminoglycoside antibiotics and promotes evolution of resistance. EBioMedicine. 2021;73:103653.
Tabata A, et al. Correlation between resistance of Pseudomonas aeruginosa to quaternary ammonium compounds and expression of outer membrane protein OprR. Antimicrob Agents Chemother. 2003;47:2093–9.
Bore E, et al. Adapted tolerance to benzalkonium chloride in Escherichia coli K-12 studied by transcriptome and proteome analyses. Microbiology. 2007;153:935–46.
Cookson B. A review: Clinical significance of emergence of bacterial antimicrobial resistance in the hospital environment. J Appl Microbiol. 2005;99:989–96. https://doi.org/10.1111/j.1365-2672.2005.02693.x.
Gaze WH, Abdouslam N, Hawkey PM, Wellington EMH. Incidence of class 1 integrons in a quaternary ammonium compound-polluted environment. Antimicrob Agents Chemother. 2005;49:1802–7.
Moënne-Loccoz Y, Mavingui P, Combes C, Normand P, Steinberg C. Microorganisms and biotic interactions. In: Environmental microbiology: fundamentals and applications. Netherlands: Springer; 2015. pp. 395–444. https://doi.org/10.1007/978-94-017-9118-2_11.
Ryu O, et al. Effects of several cosmetic preservatives on ROS-dependent apoptosis of rat neural progenitor cells. Biomol Ther. 2018;26:608–15.
Noguchi N, et al. Antiseptic susceptibility and distribution of antiseptic-resistance genes in methicillin-resistant Staphylococcus aureus. FEMS Microbiol Lett. 1999;172:247–53.
Akimitsu N, et al. Increase in resistance of methicillin-resistant Staphylococcus aureus to beta-lactams caused by mutations conferring resistance to benzalkonium chloride, a disinfectant widely used in hospitals. Antimicrob Agents Chemother. 1999;43:3042–3.
Sasatsu M. High-level resistance to ethidium bromide and antiseptics in Staphylococcus aureus. FEMS Microbiol Lett. 1992;93:109–13.
Mettler E, Carpentier B. Variations over time of microbial load and physicochemical properties of floor materials after cleaning in food industry premises. J Food Prot. 1998;61:57–65.
Brightwell G, Boerema J, Mills J, Mowat E, Pulford D. Identifying the bacterial community on the surface of IntraloxTM belting in a meat boning room by culture-dependent and culture-independent 16S rDNA sequence analysis. Int J Food Microbiol. 2006;109:47–53.
Singh Sidhu M, Heir E, Sørum H, Holck A. Genetic linkage between resistance to quaternary ammonium compounds and b-lactam antibiotics in food-related Staphylococcus spp. Micro Drug Resist. 2001;7:363–71.
Langsrud S, Sidhu MS, Heir E, Holck AL. Bacterial disinfectant resistance - a challenge for the food industry. in. Int Biodeterior Biodegrad. 2003;51:283–90.
Sidhu MS, Heir E, Leegaard T, Wiger K, Holck A. Frequency of disinfectant resistance genes and genetic linkage with β-lactamase transposon Tn552 among clinical staphylococci. Antimicrob Agents Chemother. 2002;46:2797–803.
Hegstad K, et al. Does the wide use of quaternary ammonium compounds enhance the selection and spread of antimicrobial resistance and thus threaten our health? Microb Drug Resist. 2010;16:91–104.
Ciric L, Mullany P, Roberts AP. Antibiotic and antiseptic resistance genes are linked on a novel mobile genetic element: Tn6087. J Antimicrobial Chemother. 2011;66:2235–9.
Jomova K, Valko M. Advances in metal-induced oxidative stress and human disease. Toxicology. 2011;283:65–87.
Amadi CN, Offor SJ, Frazzoli C, Orisakwe OE. Natural antidotes and management of metal toxicity. Environ Sci Pollut Res. 2019;26:18032–52.
Shi LD, et al. Will a non-antibiotic metalloid enhance the spread of antibiotic resistance genes: the selenate story. Environ Sci Technol. 2021;55:1004–14.
van Dijk HFG, et al. Resisting disinfectants. Commun Med. 2022;2:6–17.
Azeh Engwa G, Udoka Ferdinand P, Nweke Nwalo F, Unachukwu MN. Mechanism and health effects of heavy metal toxicity in humans. In Poisoning in the modern world - new tricks for an old dog? IntechOpen; 2019. https://doi.org/10.5772/intechopen.82511.
Balali-Mood M, Naseri K, Tahergorabi Z, Khazdair MR, Sadeghi M. Toxic mechanisms of five heavy metals: mercury, lead, chromium, cadmium, and arsenic. Front Pharmacol. 2021;12. https://doi.org/10.3389/fphar.2021.643972.
Shahid M, et al. Heavy-metal-induced reactive oxygen species: phytotoxicity and physicochemical changes in plants. Rev Environ Contam Toxicol. 2014;232:1–44.
Wu J, Tisa LS, Rosen BP. Membrane topology of the ArsB protein, the membrane subunit of an anion-translocating ATPase. J Biol Chem. 1992;267:12570–6.
Chen CM, Misra TK, Silver S, Rosen BP. Nucleotide sequence of the structural genes for an anion pump. The plasmid-encoded arsenical resistance operon. J Biol Chem. 1986;261:15030–8.
Chen J, Bhattacharjee H, Rosen BP. ArsH is an organoarsenical oxidase that confers resistance to trivalent forms of the herbicide monosodium methylarsenate and the poultry growth promoter roxarsone. Mol Microbiol. 2015;96:1042–52.
Wu J, Rosen BP. The arsD gene encodes a second trans-acting regulatory protein of the plasmid-encoded arsenical resistance operon. Mol Microbiol. 1993;8:615–23.
Ji G, Silver S. Reduction of arsenate to arsenite by the ArsC protein of the arsenic resistance operon of Staphylococcus aureus plasmid pI258. Proc Natl Acad Sci. 1992;89:9474–8.
Chen J, Yoshinaga M, Garbinski LD, Rosen BP. Synergistic interaction of glyceraldehydes-3-phosphate dehydrogenase and ArsJ, a novel organoarsenical efflux permease, confers arsenate resistance. Mol Microbiol. 2016;100:945–53.
Szymański P, Frączek T, Markowicz M, Mikiciuk-Olasik E. Development of copper based drugs, radiopharmaceuticals and medical materials. BioMetals. 2012;25:1089–112.
Peipert LJ, Collins KE, Zhao Q, Peipert JF. Copper intrauterine device and incident sexually transmitted infections. Am J Obstet Gynecol. 2021;225:579–80.
Qian F, Huang X, Su X, Bao Y. Responses of microbial communities and metabolic profiles to the rhizosphere of Tamarix ramosissima in soils contaminated by multiple heavy metals. J Hazard Mater. 2022;438:129469.
Zubair M, et al. Rhizobacteria and phytoremediation of heavy metals. Environ Technol Rev. 2016;5:112–9.
Barra Caracciolo A, et al. Characterization of the belowground microbial community in a poplar-phytoremediation strategy of a multi-contaminated soil. Front Microbiol. 2020;11:2073.
Besaury L, Pawlak B, Quillet L. Expression of copper-resistance genes in microbial communities under copper stress and oxic/anoxic conditions. Environ Sci Pollut Res. 2016;23:4013–23.
Martínez-Bussenius C, Navarro CA, Jerez CA. Microbial copper resistance: importance in biohydrometallurgy. Micro Biotechnol. 2017;10:279–95.
Zhang S, et al. Copper nanoparticles and copper ions promote horizontal transfer of plasmid-mediated multi-antibiotic resistance genes across bacterial genera. Environ Int. 2019;129:478–87.
Xavier JC, et al. Evaluation of the microbial diversity and heavy metal resistance genes of a microbial community on contaminated environment. Appl Geochem. 2019;105:1–6.
Li J, Phulpoto IA, Zhang G, Yu Z. Acceleration of emergence of E. coli antibiotic resistance in a simulated sublethal concentration of copper and tetracycline co-contaminated environment. AMB Express. 2021;11:1–11.
Lund PA, Brown NL. Role of the merT and merP gene products of transposon Tn501 in the induction and expression of resistance to mercuric ions. Gene. 1987;52:207–14.
Schiering N, et al. Structure of the detoxification catalyst mercuric ion reductase from Bacillus sp. strain RC607. Nature. 1991;352:168–72.
Moore MJ, Distefano MD, Walsh CT, Schiering N, Pai EF. Purification, crystallization, and preliminary X-ray diffraction studies of the flavoenzyme mercuric ion reductase from Bacillus sp. Strain RC607. J Biol Chem. 1989;264:14386–8.
Nucifora G, Chu L, Silver S, Misra TK. Mercury operon regulation by the merR gene of the organomercurial resistance system of plasmid pDU1358. J Bacteriol. 1989;171:4241–7.
Foster TJ, Brown NL. Identification of the merR gene of R100 by using mer-lac gene and operon fusions. J Bacteriol. 1985;163:1153–7.
Parks JM, et al. The genetic basis for bacterial mercury methylation. Science. 2013;339:1332–5.
Edlund C, Bjorkman L, Ekstrand J, Englund GS, Nord CE. Resistance of the normal human microflora to mercury and antimicrobials after exposure to mercury from dental amalgam fillings. Clin Infect Dis. 1996;22:944–50.
Rupp ME, et al. Effect of silver-coated urinary catheters: efficacy, cost-effectiveness, and antimicrobial resistance. Am J Infect Control. 2004;32:445–50.
Lansdown ABG. Silver in health care: antimicrobial effects and safety in use. in Biofunctional Text Ski. 2006;33:17–34.
Jin M, et al. Chlorine disinfection promotes the exchange of antibiotic resistance genes across bacterial genera by natural transformation. ISME J. 2020;14:1847–56.
Liao C, Li Y, Tjong S. Bactericidal and cytotoxic properties of silver nanoparticles. Int J Mol Sci. 2019;20:449.
Prabhu S, Poulose EK. Silver nanoparticles: mechanism of antimicrobial action, synthesis, medical applications, and toxicity effects. Int Nano Lett. 2012;2:32.
Matsumura Y, Yoshikata K, Kunisaki S, Tsuchido T. Mode of bactericidal action of silver zeolite and its comparison with that of silver nitrate. Appl Environ Microbiol. 2003;69:4278–81.
Morones JR, et al. The bactericidal effect of silver nanoparticles. Nanotechnology. 2005;16:2346–53.
Feng QL, et al. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J Biomed Mater Res. 2000;52:662–8.
Slawson RM, van Dyke MI, Lee H, Trevors JT. Germanium and silver resistance, accumulation, and toxicity in microorganisms. PLASMID. 1992;27:72–79.
Robinson JB, Tuovinen OH. Mechanisms of microbial resistance and detoxification of mercury and organomercury compounds: physiological, biochemical, and genetic analyses. Microbiol Rev. 1984;48:95–124.
Trevors JT. Silver resistance and accumulation in bacteria. Enzym Micro Technol. 1987;9:331–3.
Bennett PM. Plasmid encoded antibiotic resistance: acquisition and transfer of antibiotic resistance genes in bacteria. Br J Pharm. 2008;153:S347–S357.
Silver S. Bacterial silver resistance: molecular biology and uses and misuses of silver compounds. FEMS Microbiol Rev. 2003;27:341–53.
Hendry AT, Stewart IO. Silver-resistant Enterobacteriaceae from hospital patients. Can J Microbiol. 1979;25:915–21.
Mchugh GL, Moellering RC, Hopkins CC, Swartz MN. Salmonella typhimurium resistant to silver nitrate, chloramphenicol, and ampicillin. Lancet. 1975;305:235–40.
Gordienko MG, et al. Antimicrobial activity of silver salt and silver nanoparticles in different forms against microorganisms of different taxonomic groups. J Hazard Mater. 2019;378:1–11.
Muller M, Merrett ND. Pyocyanin production by Pseudomonas aeruginosa confers resistance to ionic silver. Antimicrob Agents Chemother. 2014;58:5492–9.
Berni Canani R, Buccigrossi V, Passariello A. Mechanisms of action of zinc in acute diarrhea. Curr Opin Gastroenterol. 2011;27:8–12.
Hernick M, Fierke CA. Zinc hydrolases: the mechanisms of zinc-dependent deacetylases. Arch Biochem Biophys. 2005;433:71–84.
Gupta M, Mahajan VK, Mehta KS, Chauhan PS. Zinc therapy in dermatology: a review. Dermatol Res Pr. 2014;2014:1–11.
Prasad AS. Zinc in human health: an update. J Trace Elem Exp Med. 1998;11:63–87.
Saper RB, Rash R. Zinc: an essential micronutrient. Am Fam Physician. 2009;79:768–72.
David R. Why zinc is bad for bacteria. Nat Rev Microbiol. 2012;10:4.
McDevitt CA, et al. A molecular mechanism for bacterial susceptibility to zinc. PLoS Pathog. 2011;7:e1002357.
Shoeb E, et al. Horizontal gene transfer of stress resistance genes through plasmid transport. World J Microbiol Biotechnol. 2012;28:1021–5.
Spain A, Alm E. Implications of microbial heavy metal tolerance in the environment. Rev Undergraduate Res. 2003;2 http://www.epa.gov/ogwdw000/ars/ars9.html.
Wang Y, Xiao M, Geng X, Liu J, Chen J. Horizontal transfer of genetic determinants for degradation of phenol between the bacteria living in plant and its rhizosphere. Appl Microbiol Biotechnol. 2007;77:733–9.
Nies DH, Nies A, Chu L, Silver S. Expression and nucleotide sequence of a plasmid-determined divalent cation efflux system from Alcaligenes eutrophus (heavy metal plasmid resistance/cation transport system). Proc Nati Acad Sci USA. 1989;86:7351–5.
Adekanmbi AO, Adeleke OJ, Aremu OO, Olaposi AV. Molecular characterization, antibiogram and distribution of zntA gene in zinc-resistant Escherichia coli population recovered from anthropogenically-influenced surface water sources in Nigeria. Meta Gene. 2020;26:100789.
Højberg O, Canibe N, Poulsen HD, Hedemann MS, Jensen BB. Influence of dietary zinc oxide and copper sulfate on the gastrointestinal ecosystem in newly weaned piglets. Appl Environ Microbiol. 2005;71:2267–77.
Shi J, Su Y, Zhang Z, Wei H, Xie B. How do zinc oxide and zero valent iron nanoparticles impact the occurrence of antibiotic resistance genes in landfill leachate? Environ Sci Nano. 2019;6:2141–51.
Cavaco LM, et al. Cloning and occurrence of czrC, a gene conferring cadmium and zinc resistance in methicillin-resistant Staphylococcus aureus CC398 isolates. Antimicrob Agents Chemother. 2010;54:3605–8.
da Costa P, Loureiro L, Matos A. Transfer of multidrug-resistant bacteria between intermingled ecological niches: the interface between humans, animals and the environment. Int J Environ Res Public Health. 2013;10:278–94.
Argudín MA, et al. Bacteria from animals as a pool of antimicrobial resistance genes. Antibiotics. 2017;6. https://doi.org/10.3390/antibiotics6020012.
Andremont A, et al. Fighting bacterial resistance at the root: need for adapted EMEA guidelines. Lancet Infect Dis. 2011;11:6–8.
Jones IA, Joshi LT. Biocide use in the antimicrobial era: a review. Molecules. 2021;26:2276.
Lowbury EJ. Chlorhexidine. Practitioner. 1957;179:489–93.
Chlorhexidine - an overview, ScienceDirect Topics. 2018. https://www.sciencedirect.com/topics/medicine-and-dentistry/chlorhexidine.
Brookes ZLS, Bescos R, Belfield LA, Ali K, Roberts A. Current uses of chlorhexidine for management of oral disease: a narrative review. J Dent. 2020;103:103497.
Kampf G. Antibiotic resistance can be enhanced in gram-positive species by some biocidal agents used for disinfection. Antibiotics. 2019;8:13.
Cook HA, Cimiotti JP, Della-Latta P, Saiman L, Larson EL. Antimicriobial resistance patterns of colonizing flora on nurses’ hands in the neonatal intensive care unit. Am J Infect Control. 2007;35:231–6.
Bhardwaj P, Ziegler E, Palmer KL. Chlorhexidine induces VanA-type vancomycin resistance genes in Enterococci. Antimicrob Agents Chemother. 2016;60:2209–21.
Bock LJ, Wand ME, Sutton JM. Varying activity of chlorhexidine-based disinfectants against Klebsiella pneumoniae clinical isolates and adapted strains. J Hospital Infect. 2016;93:42–48.
Wand ME, Bock LJ, Bonney LC, Sutton JM. Mechanisms of increased resistance to chlorhexidine and cross-resistance to colistin following exposure of klebsiella pneumoniae clinical isolates to chlorhexidine. Antimicrob Agents Chemother. 2017;61:1–12.
Conceição T, de Lencastre H, Aires-de-Sousa M. Prevalence of biocide resistance genes and chlorhexidine and mupirocin non-susceptibility in Portuguese hospitals during a 31-year period (1985–2016). J Glob Antimicrob Resist. 2021;24:169–74.
Horner C, Mawer D, Wilcox M. Reduced susceptibility to chlorhexidine in staphylococci: Is it increasing and does it matter? J Antimicrobial Chemother. 2012;67:2547–59.
Sekavec JG, Moore WT, Gillock ET. Chlorhexidine resistance in a Gram-negative bacterium isolated from an aquatic source. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2013;48:1829.
Dance DAB, Pearson AD, Seal DV, Lowes JA. A hospital outbreak caused by a chlorhexidine and antibiotic-resistant Proteus mirabilis. J Hosp Infect. 1987;10:10–16.
Pumbwe L, Skilbeck CA, Wexler HM. Induction of multiple antibiotic resistance in Bacteroides fragilis by benzene and benzene-derived active compounds of commonly used analgesics, antiseptics and cleaning agents. J Antimicrobial Chemother. 2007;60:1288–97.
Fraud S, Campigotto AJ, Chen Z, Poole K. MexCD-OprJ multidrug efflux system of pseudomonas aeruginosa: involvement in chlorhexidine resistance and induction by membrane-damaging agents dependent upon the AlgU stress response sigma factor. Antimicrob Agents Chemother. 2008;52:4478.
Tag ElDein MA, Yassin AS, El-Tayeb O, Kashef MT. Chlorhexidine leads to the evolution of antibiotic-resistant Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis. 2021;40:2349–61.
Heckman JR. Chlorine. In Handbook of Plant Nutrition. Florida: CRC Press; 2016. pp. 295–308. https://doi.org/10.1201/9781420014877-12.
Anand SS, Philip BK, Mehendale HM. Chlorination byproducts. In: Encyclopedia of toxicology. 3rd ed. 2014. pp. 855–9 https://doi.org/10.1016/B978-0-12-386454-3.00276-1.
Luo L-W, et al. Evaluating method and potential risks of chlorine-resistant bacteria (CRB): a review. Water Res. 2021;188:116474.
Wang L, et al. Assessment of the UV/chlorine process in the disinfection of Pseudomonas aeruginosa: efficiency and mechanism. Environ Sci Technol. 2021;55:9221–30.
Muller JF, Ghosh S, Ikuma K, Stevens AM, Love NG. Chlorinated phenol-induced physiological antibiotic resistance in Pseudomonas aeruginosa. FEMS Microbiol Lett. 2015;362:172.
Tong C, et al. Chlorine disinfectants promote microbial resistance in Pseudomonas sp. Environ Res. 2021;199:111296.
Huang JJ, Hu HY, Wu YH, Wei B, Lu Y. Effect of chlorination and ultraviolet disinfection on tetA-mediated tetracycline resistance of Escherichia coli. Chemosphere. 2013;90:2247–53.
Zhang Z, et al. Residual chlorine disrupts the microbial communities and spreads antibiotic resistance in freshwater. J Hazard Mater. 2022;423:127152.
Liu SS, et al. Chlorine disinfection increases both intracellular and extracellular antibiotic resistance genes in a full-scale wastewater treatment plant. Water Res. 2018;136:131–6.
Shrivastava R, et al. Suboptimal chlorine treatment of drinking water leads to selection of multidrug-resistant Pseudomonas aeruginosa. Ecotoxicol Environ Saf. 2004;58:277–83.
5 Things to Know About Triclosan, FDA. https://www.fda.gov/consumers/consumer-updates/5-things-know-about-triclosan.
Olaniyan LWB, Mkwetshana N, Okoh AI. Triclosan in water, implications for human and environmental health. Springerplus. 2016;5:1639.
Heath RJ, et al. Mechanism of triclosan inhibition of bacterial fatty acid synthesis. J Biol Chem. 1999;274:11110–4.
Drury B, Scott J, Rosi-Marshall EJ, Kelly JJ. Triclosan exposure increases triclosan resistance and influences taxonomic composition of benthic bacterial communities. Environ Sci Technol. 2013;47:8923–30.
Zeng W, et al. The prevalence and mechanism of triclosan resistance in Escherichia coli isolated from urine samples in Wenzhou, China. Antimicrob Resist Infect Control. 2020;9:161.
Mcmurry LM, Oethinger M, Levy SB. Overexpression of marA, soxS, or acrAB produces resistance to triclosan in laboratory and clinical strains of Escherichia coli. FEMS Microbiol Lett. 1998;166:305–9.
Westfall C, et al. The widely used antimicrobial triclosan induces high levels of antibiotic tolerance in vitro and reduces antibiotic efficacy up to 100-fold in vivo. Antimicrob Agents Chemother. 2019;63:1–28.
Chuanchuen R, et al. Cross-resistance between triclosan and antibiotics in Pseudomonas aeruginosa is mediated by multidrug efflux pumps: exposure of a susceptible mutant strain to triclosan selects nfxB mutants overexpressing MexCD-OprJ. Antimicrob Agents Chemother. 2001;45:428.
Parikh SL, Xiao G, Tonge PJ. Inhibition of InhA, the enoyl reductase from Mycobacterium tuberculosis, by triclosan and isoniazid. Biochemistry. 2000;39:7645–50.
Elekhnawy E, Sonbol F, Abdelaziz A, Elbanna T. An investigation of the impact of triclosan adaptation on Proteus mirabilis clinical isolates from an Egyptian university hospital. Braz J Microbiol. 2021;52:927–37.
Cetrimide | C17H38BrN - PubChem. https://pubchem.ncbi.nlm.nih.gov/compound/Cetrimide.
Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine in endodontics. Int Endod J. 2009;42:288–302.
Ruiz-Linares M, et al. Antimicrobial activity of alexidine, chlorhexidine and cetrimide against Streptococcus mutans biofilm. Ann Clin Microbiol Antimicrob. 2014;13:1–6.
Gilbert P, Moore LE. Cationic antiseptics: diversity of action under a common epithet. J Appl Microbiol. 2005;99:703–15.
Cetrimonium bromide and cetrimide. Meyler’s side effects of drugs. vol. 224, 2016. https://doi.org/10.1016/B978-0-444-53717-1.00469-8.
Gadea R, Glibota N, Pérez Pulido R, Gálvez A, Ortega E. Adaptation to biocides cetrimide and chlorhexidine in bacteria from organic foods: association with tolerance to other antimicrobials and physical stresses. J Agric Food Chem. 2017;65:1758–70.
Rossouw FT, Rowbury RJ. Effects of the resistance plasmid R124 on the level of the OmpF outer membrane protein and on the response of Escherichia coli to environmental agents. J Appl Bacteriol. 1984;56:63–79.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baig, M.I.R., Kadu, P., Bawane, P. et al. Mechanisms of emerging resistance associated with non-antibiotic antimicrobial agents: a state-of-the-art review. J Antibiot 76, 629–641 (2023). https://doi.org/10.1038/s41429-023-00649-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-023-00649-4
This article is cited by
-
Operando investigation of the synergistic effect of electric field treatment and copper for bacteria inactivation
Nature Communications (2024)
-
Antibiotic stewardship programs should include disinfectants and biocides
The Journal of Antibiotics (2023)