Abstract
Background
Acute lymphocytic leukaemia (ALL) and non-Hodgkin lymphoma (NHL) are among the commonest types of childhood cancer. Some previous studies suggested that elevated ultraviolet radiation (UVR) exposures increase ALL risk; many more indicate NHL risk is reduced.
Methods
We assessed age<20 ALL/NHL incidence in Surveillance, Epidemiology and End Results data using AVGLO-derived UVR irradiance/cumulative radiant exposure measures, using quasi-likelihood models accounting for underdispersion, adjusted for age, sex, racial/ethnic group and other county-level socioeconomic variables.
Results
There were 30,349 cases of ALL and 8062 of NHL, with significant increasing trends of ALL with UVR irradiance (relative risk (RR) = 1.200/mW/cm2 (95% CI 1.060, 1.359, p = 0.0040)), but significant decreasing trends for NHL (RR = 0.646/mW/cm2 (95% CI 0.512, 0.816, p = 0.0002)). There was a borderline-significant increasing trend of ALL with UVR cumulative radiant exposure (RR = 1.444/MJ/cm2 (95% CI 0.949, 2.197, p = 0.0865)), and significant decreasing trends for NHL (RR = 0.284/MJ/cm2 (95% CI 0.166, 0.485, p < 0.0001)). ALL and NHL trend RR is substantially increased among those aged 0–3. All-age trend RRs are most extreme (increasing for ALL, decreasing for NHL) for Hispanics for both UVR measures.
Conclusions
Our more novel finding, of excess UVR-related ALL risk, is consistent with some previous studies, but is not clear-cut, and in need of replication.
Similar content being viewed by others
Introduction
Acute lymphocytic leukaemia (ALL) and non-Hodgkin lymphoma (NHL) are among the most common cancers in childhood in developed countries, in that order [1, 2]. The reported increasing incidence rates seen in the US and in other developed countries in pediatric lymphoid leukaemia rates [3], in particular for B-cell precursor ALL (but not for T-ALL nor acute myeloid leukaemia (AML)) [4], and NHL [3, 5] point towards a role for the modern lifestyle. To date there are relatively few well-established environmental risk factors for such paediatic cancers. For ALL these include ionising radiation [6, 7], heavy birth weight [8,9,10,11] and male sex [10]. NHL is not generally thought to be associated with ionising radiation exposure [6, 7]. There is a modest but significant socio-economic gradient for ALL, at least in the UK and USA, with increasing rates of ALL in higher socioeconomic classes [12,13,14]. There is also a substantial body of data suggesting a role for infections in childhood ALL [15,16,17]. The aetiology of NHL in childhood is poorly understood, the only well-established risk factors being those associated with dysregulation of the immune system [18]. There are known difference in rates of most common types of childhood cancer between racial/ethnic groups [19].
A Finnish cancer incidence study suggested that rates of childhood ALL slightly increased during the lighter part of the year, the increase being most pronounced for children aged 2-4 [20]. A study of childhood haematological malignancies in France demonstrated increasing rates of precursor B-cell ALL with increasing levels of solar ultraviolet radiation (UVR), but no significant variation of NHL [21]. A Greek case/control study reported significant reduction in rates of childhood NHL associated with more than 15 days annual sunbathing [22]. A meta-analysis of population-level cancer incidence data from 57 countries suggested decreased risk of ALL and increased risk of NHL in childhood associated with increased solar exposure, although only the former trend was significant (p < 0.01) [23].
In the current study we analyse childhood ALL and NHL risk in relation to solar exposure in the current Surveillance, Epidemiology and End Results (SEER) data [2] aggregated at the county level. We shall consider a number of different metrics of ambient solar exposure, and assess variations in solar-associated risk of ALL and NHL by sex and major racial/ethnic group.
Materials and methods
Study population
County level SEER22 data for cases diagnosed in 2000–2020 was used [2] in population-based SEER cancer registries, restricting to ALL and NHL cases under the age of 20 (not inclusive). We included registries pertaining to parts of the states of California, Connecticut, Georgia, Idaho, Illinois, Iowa, Kentucky, Louisiana, Massachusetts, New Jersey, New Mexico, New York, Texas, Utah and Washington; as detailed in the Supplement A (Methods) certain other states in SEER22 were omitted for various reasons. In the analytical cohort, there were a total of 1078 counties, with total populations (under age 20) ranging from 25 to 2.68 ×106, with mean 3.67 ×104.
ALL was defined by the lymphoid neoplasm recode 2021 Revision of ‘2(a)1 Precursor Non-Hodgkin lymphoma, B-cell’, and ‘2(b)1 Precursor Non-Hodgkin lymphoma, T-cell’ [24]. For cases diagnosed in 2000–2012, we additionally included ALL cases that had a histology code of the international classification of disease for oncology (ICD-O-3) ‘9727’ [25].
NHL was defined using ‘2(a)2 Mature Non-Hodgkin lymphoma, B-cell’, ‘2(a)3 Non-Hodgkin lymphoma, B-cell, NOS ‘, and ‘2(b)2 Mature Non-Hodgkin lymphoma, T-cell’, or with a ICD-O-3 histology code of ‘9832’ [24]. For cases diagnosed in 2013–2020, we additionally included NHL cases with a histology code of ‘9727’ [25].
We restricted analysis to the four main racial/ethnic groups, namely white non-Hispanic, black non-Hispanic, Hispanic (all races), and non-Hispanic Asian or Pacific Islanders. Further details of groups excluded are detailed in the Supplement A (Methods). The county population-year counts used in the calculation of population-years (somewhat analogous to person–years) at risk were based on the 2000 U.S. standard population (single ages to 84 – Census P25-1130). Given the known difference in childhood cancer rates between these racial/ethnic groups [19], and the geographical heterogeneity of distribution of the various racial/ethnic groups, analysis of exposure response could be potentially confounded. We therefore adjusted for racial/ethnic group in all analyses.
Solar radiation exposure assessment
The AVerage daily total GLObal solar radiation (AVGLO) estimates that are employed are derived used the National Solar Radiation Database (NSRAD) produced by the National Renewable Energy Laboratory (NREL) under the US Department of Energy’s Resource Assessment Program. This is the largest ground-based solar measurement network in the US, containing statistical summaries computed from hourly measurement data (with some infilling for missing data) for 239 US radiation stations for the period 1961–1990, including monthly, yearly, and 30-year average global solar radiation measures, and gives estimates of ambient solar exposure cumulated over a day, measured in W hour/m2. We employ county-level interpolations developed by Tatalovich et al. [26] which deliver estimates of potential solar ambient irradiance (~100–3000 nm) at 1 km² resolution in the mainland US. Linkage of SEER data to this interpolated AVGLO exposure database was via the county-level Federal Information Processing System (FIPS) code. Further details, in particular details of data mislinkage (because of incompleteness in either the SEER or AVGLO data), are given in the Supplement A (Methods).
Two candidate exposure metrics are suggested a priori, namely UVR irradiance (in units of mW/cm2), which is proportional to UVR power density on a surface, or UVR cumulative radiant exposure (in units of MJ/cm2), which is proportional to cumulative solar UVR energy deposition on a surface. These are measures of UVR exposure recommended by the Commission Internationale de l’Eclairage (CIE) [27]. As noted in the Supplement A (Methods) AVGLO is approximately proportional to the average total solar irradiance (in units of mW/cm2). We shall also use the measure of cumulative radiant exposure (in units of MJ/cm2). The derivation of both measures is explained in more detail in the Supplement A (Methods), and is as previously employed [28,29,30].
Statistical analysis
Because of marked under-dispersion, with variance generally reduced by about 10% over the Poisson-expected rates in certain race-sex subgroups for both disease endpoints, a quasi-likelihood model was used for all model fits and tests of significance [31]. The model assumes that the expected number of cases in the stratum with population-years \(P{Y}_{i}\), after UVR exposure, \({H}_{i}\) (using either irradiance or cumulative radiant exposure), with various other explanatory covariates, \({X}_{i}=({X}_{ij})\), is given by:
The population in each year and subgroup defined by the stratification is summed over each separate calendar year to give the population-year total \(P{Y}_{i}\) for that subgroup. Model fitting is performed in R [32] using the glm function. Other variables used for adjustment were taken from a set of demographic/socioeconomic variables measured at county level. The variables measured are described in Supplement A Table A1. To avoid variables that could potentially soak up the effect of UVR exposure, we exclude any which had absolute value of the (Pearson) correlation with UVR irradiance of 0.1 or greater. In order to avoid over-parameterised models, the Akaike Information Criterion (AIC) [33, 34] was employed to select the optimal subset of descriptive variables from this set. A mixed forward-backward stepwise algorithm was used to select the set of variables minimising AIC, using R [32]. In order to test the effect of excluding those baseline variables with correlation >0.1, this restriction was relaxed, and AIC used to select the optimal subset of descriptive variables again. We also performed sensitivity analysis via model fits in which the demographic/socioeconomic variables were omitted. Profile-likelihood confidence intervals (CI) were estimated from the quasi-likelihood [31]. All statistical tests were two-sided.
Results
Among the four main racial/ethnic groups analysed here there are 30,349 ALL cases and 8062 cases of NHL among a population with 831,424,805 population-years of follow-up (Tables 1 and 2).
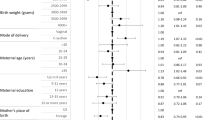
For ALL there are highly significant effects of age (with risk varying in a U-shaped manner, peaking at ages 2-3 years), sex (risk for males ~1.29× females), racial/ethnic group (risks for black non-Hispanics ~0.57× white non-Hispanics, risks of Hispanics ~1.33× white non-Hispanics, risks of Asian/Pacific Islanders ~0.94× white non-Hispanics), median rent (with risk decreasing with cheaper rent), heterogeneity by SNAP and increasing trends over time (Table 2). For NHL there are highly significant effects of age (with risk increasing with age), sex (risk for males ~1.87× females), racial/ethnic group (risks for black non-Hispanics ~0.88× white non-Hispanics, risks of Hispanics ~0.82× white non-Hispanics, risks of Asian/Pacific Islanders ~1.04× white non-Hispanics), median rent (risk decreasing in lower rental-cost accommodation), heterogeneity by SNAP and increasing trends over time (Table 2). All heterogeneity p-values are highly significant (p < 0.0001).
The stepAIC algorithm suggests that the optimal background model for ALL includes age, racial/ethnic group, sex, median rent, calendar year, age × racial/ethnic group, age × sex, age × calendar year, racial/ethnic group × calendar year in that order; for NHL the optimal set of explanatory variables are age, sex, racial/ethnic group, median rent, calendar year, SNAP, age × sex, and racial/ethnic group × sex, in that order.
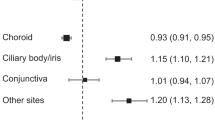
Table 3 and Fig. 1 demonstrate that using this model (and obvious simplifications [omitting the interaction terms in racial/ethnic group and sex] in the racial/ethnic group x sex subgroups) there is a highly significant trend of ALL with UVR irradiance, with relative risk (RR) = 1.200/mW/cm2 (95% CI 1.060, 1.359, p = 0.0040). There are increasing trends of ALL with solar exposure in various racial/ethnic group/sex subgroups, in particular in Hispanic boys (p = 0.0007) and girls (p = 0.0020) (Table 3). However, there is only a borderline significant increasing trend of ALL incidence with UVR cumulative radiant exposure, with RR = 1.444/MJ/cm2 (95% CI 0.949, 2.197, p = 0.0865), although there are significant increasing trends of ALL with UVR cumulative radiant exposure among Hispanic boys (p = 0.0337) and girls (p = 0.0133) (Table 3). Very similar results are obtained if demographic/socioeconomic variables are not used for adjustment (Table 3). Supplement A Table A2 demonstrates that there is evidence of modification of trend RR by race, for ALL (all but one p-value < 0.05), although very little evidence of such modification for sex (all p-values > 0.5). The largest UVR irradiance trend RR for ALL is for Hispanics with RR = 1.517 /mW/cm2 (95% CI 1.254, 1.837), compared with RR = 1.079 /mW/cm2 (95% CI 0.896, 1.300) for White non-Hispanics, RR = 0.903 /mW/cm2 (95% CI 0.537, 1.516) for Black non-Hispanics and RR = 0.708 /mW/cm2 (95% CI 0.442, 1.136) for Asian or Pacific Islanders (Supplement A Table A3). Likewise the largest UVR cumulative radiant exposure trend RR for ALL is for Hispanics with RR = 2.593 /MJ/cm2 (95% CI 1.387, 4.859), compared with RR = 0.999 /MJ/cm2 (95% CI 0.521, 1.913) for White non-Hispanics, RR = 1.504 /MJ/cm2 (95% CI 0.288, 7.772) for Black non-Hispanics and RR = 0.245 /MJ/cm2 (95% CI 0.047, 1.283) for Asian or Pacific Islanders (Supplement A Table A3).
a acute lymphocytic leukaemia (ALL) in relation to UVR irradiance, (b) acute lymphocytic leukaemia (ALL) in relation to UVR cumulative radiant exposure (c) non-Hodgkin lymphoma in relation to UVR irradiance, (d) non-Hodgkin lymphoma in relation to UVR cumulative radiant exposure. Fitted models are the most complete (all racial/ethnic group, both sexes) AIC-optimal models given in Tables 3 and 4.
By contrast, Table 4 and Fig. 1 demonstrate that solar exposure appears protective for NHL, with decreases in incidence for increasing UVR irradiance with RR = 0.646 /mW/cm2 (95% CI 0.512, 0.816, p = 0.0002). This is also observed, if sometimes only at borderline levels of statistical significance, in a number of racial/ethnic/sex subgroups, in particular in white non-Hispanic boys and girls (p = 0.0348, p = 0.0282, respectively), and Hispanic boys (p = 0.0024) (Table 4), although not in Asian or Pacific Islander children, among whom there are indications of increased NHL risk with increasing irradiance, borderline significant for males (p = 0.1074) and significant (p = 0.0282) for females. There is also a highly significant decreasing trend of NHL with UVR cumulative radiant exposure, with RR = 0.284/MJ/cm2 (95% CI 0.166, 0.485, p < 0.0001), with again significant or borderline significant decreasing trends in white non-Hispanic boys (p = 0.0033) and girls (p = 0.0666) and in Hispanic boys (p = 0.0008) (Table 4). By contrast, there are indications of increased NHL incidence with increasing UVR cumulative radiant exposure among Asian or Pacific Islander children, which for girls is significant (p = 0.0074). Very similar results are obtained if demographic/socioeconomic variables are not used for adjustment (Table 4). Supplement A Table A2 demonstrates that there is evidence of modification of RR by race for NHL (all p-values < 0.05), although little evidence of such modification for sex (all p-values > 0.05). The lowest UVR irradiance trend RR for NHL is for Hispanics with RR = 0.545/mW/cm2 (95% CI 0.359, 0.829), compared with RR = 0.602 /mW/cm2 (95% CI 0.434, 0.833) for White non-Hispanics, RR = 0.578/mW/cm2 (95% CI 0.277, 1.200) for Black non-Hispanics and RR = 2.059/mW/cm2 (95% CI 0.933, 4.574) for Asian or Pacific Islanders (Supplement A Table A3). Likewise the lowest UVR cumulative radiant exposure trend RR for NHL is for Hispanics with RR = 0.218/MJ/cm2 (95% CI 0.123, 0.386), compared with RR = 0.336/MJ/cm2 (95% CI 0.188, 0.600) for White non-Hispanics, RR = 0.511/MJ/cm2 (95% CI 0.250, 1.041) for Black non-Hispanics and RR = 0.331/MJ/cm2 (95% CI 0.155, 0.708) for Asian or Pacific Islanders (Supplement A Table A3).
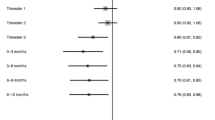
Table 5 demonstrates that there is no significant variation in risk of ALL in different age groups whether in relation to irradiance (p = 0.9087) or cumulative radiant exposure (p = 0.3174). Nevertheless, there is reduction in trend RR with increasing age, both in relation to irradiance or cumulative radiant exposure, with large (and significant) risks for the age group 0–3, particularly in relation to cumulative radiant exposure; so that for example for ages 0–3 RR = 1.269 /mW/cm2 (95% CI 1.024, 1.573) and RR = 20.58 /MJ/cm2 (95% CI 1.559, 272.0), both measures generally decreasing with increasing age, with in some cases trend RR < 1 for older ages. Table 5 also shows that the evidence for such heterogeneity for NHL is stronger, at least for irradiance (p = 0.0113), although less so for cumulative radiant exposure (p = 0.1844). As for ALL, it is notable that there are large (and significant) risks for NHL for the age group 0–3, in relation to both UVR metrics and particularly for cumulative radiant exposure; so that for example for ages 0–3 RR = 2.483/mW/cm2 (95% CI 1.129, 5.463) and RR = 21,881/MJ/cm2 (95% CI 1.960, >106), both measures generally decreasing with increasing age, with in most cases trend RR < 1 for older ages. Very similar results are obtained if the analyses omit adjustment for the various demographic/socioeconomic variables.
Supplement A Table A4 illustrates the effect of relaxing the restriction on baseline variables having correlation with UVR < 0.1. As can be seen, comparing also with the results in Tables 3 and 4, the effect of allowing these extra variables to be used is to generally weaken the UVR-associated trends, whether the generally positive trends for ALL, or the generally negative trends for NHL. Supplement A Table A5 demonstrates that there is no significant variation in risk of ALL in different median rent groups whether in relation to irradiance (p = 0.8023) or cumulative radiant exposure (p = 0.8974); Supplement A Table A6 shows that the evidence for such heterogeneity for NHL is scarcely stronger, whether in relation to irradiance (p = 0.1628) or cumulative radiant exposure (p = 0.1646). There is high negative correlation between solar exposure and latitude, with \(\rho =-0.729\) (data not shown).
Discussion
The present study has demonstrated a highly significant increase in risk of ALL for age <20 with increasing levels of solar UVR exposure (Table 3). However, the significance of the increasing trend is only seen in the Hispanic group. Although there is some overlap of RR and CI for irradiance and cumulative radiant exposure for the four ethnic groups, nevertheless there is significant heterogeneity by ethnic group using both UVR metrics (most p < 0.05), with trend RR highest for Hispanics (Supplement A Tables A2, A3). The increase is seen using UVR irradiance, and much less strongly using UVR cumulative radiant exposure. By contrast, there are highly significant decreases in risk of NHL, using either measure of UVR exposure (Table 4). Although there is some overlap of RR for irradiance and cumulative radiant exposure for the four ethnic groups, nevertheless there is significant heterogeneity by ethnic group using both UVR metrics (all p < 0.05), with trend RR lowest for Hispanics, and for most other racial/ethnic groups trend RR < 1 (Supplement A Tables A2 and A3). Both for ALL and NHL the risk appears to be concentrated in the youngest age group (0–3 years), and in both endpoints and all UVR metrics, but particularly for cumulative radiant exposure, the trend RR is increased in this age group (Table 5).
Our findings of increased risk of ALL with increasing solar exposure parallel those found in a large recent French ecological study of childhood cases, based on high quality ground-based UV measurements, somewhat similar to the AVGLO measurements used in the present study, and which demonstrated increasing risk of precursor B-cell ALL with elevated UVR, with RR = 1.41 (95% CI 1.13, 1.69) per 100 J/cm2 /day [21]. This is similar to the figure we derive of 1.235 per 100 J/cm2 /day (95% CI 1.070, 1.426) (Table 3). A Finnish study suggested that rates of childhood ALL slightly (but non-significantly) increased during the lighter part of the year (April-September), the increase being most pronounced, about 18% (and borderline significant) for children aged 2–4 [20]. However, it is the studies of long-term solar exposure which are more comparable with the structure of our data. A Californian study using AVGLO UVR data suggested a mild and borderline significant (p = 0.042) protective effect of increased UVR on early childhood (under age 5 year) ALL rates [35]. This study also showed a protective effect of UVR in children of Hispanic and Black mothers [35], again in contrast to our findings (Table 3, Supplement A Table A3). A meta-analysis of population-level cancer incidence data by registry suggested that rates of childhood ALL significantly increased (p < 0.01) with increasing degrees of registry latitude [23], again suggestive of a protective effect. A study of all-age leukaemia mortality data in Spain observed decreases with increasing latitude, suggestive of elevated UVR-associated risk [36].
Our findings of a protective effect of solar exposure on NHL (albeit not for ages 0–3) should be compared with those found in a French ecological study which reported a non-significant increased risk of NHL of RR = 1.26 (95% CI 0.89, 1.87) per 100 J/cm2 /day [21]. This is very much higher, and inconsistent with the significant negative trend we derive of RR = 0.603 per 100 J/cm2 /day (95% CI 0.461, 0.790) (Table 4). A meta analysis, conducted at the level of cancer registry (including 75 registries among 57 countries at all levels of economic development) reported weak and non-significant decreasing trends of childhood NHL with increasing registry latitude [23], suggesting a weak positive trend with UVR. Kim et al. [37] conducted a systematic review and meta-analysis of 17 case-control and 9 cohort studies, all but two covering the full age range, and all relating to developed countries (Australia, Denmark, Europe, France, Germany, Greece, Italy, Norway, Singapore, Sweden, UK, USA) mostly in the northern hemisphere, suggested that NHL risk decreased with increasing personal sunlight exposure in relation to a number of metrics, relating both to solar exposure in childhood and in adulthood. On the other hand, Lu et al. [38] conducted a systematic review and meta-analysis of 10 case-control and 1 cohort studies of occupational exposure, again of developed countries (Australia, Denmark, Europe, Germany, Singapore, Sweden, USA) mostly in the northern hemisphere, which suggested a weak positive association of NHL with solar exposure. Petridou et al. [22] studied 87 cases of NHL at ages 0–14 from a Greek national network of oncology units together with 164 age/sex-matched controls. Average time spent sunbathing per year was determined by interviewing guardians. There was a significant (p = 0.002) reduction in rate of childhood NHL incidence associated with more than 15 days annual sunbathing. The Interlymph Consortium case-control study, analysed by combining trends for each centre, each one in a developed country (Australia, Canada, Denmark, France, Germany, Ireland, Italy, Spain, Sweden, UK, USA) mostly in the northern hemisphere, using meta-analytic tools, suggested weak protective effects of UVR for NHL at ages 10–17 in relation to daily hours of UVR exposure, which were borderline significant (p = 0.06) in relation to total sun exposure [39]. A small Californian study using the same AVGLO assessments of UVR as employed here suggested a modest and non-statistically significant (p > 0.1) protective effect of increased solar UVR on childhood NHL, in particular in relation to children of Hispanic and White mothers [35]. There are also a number of all-age studies, in particular Grant [36] who documented increasing trends of all-age NHL mortality with increasing latitude in Spain, suggesting a protective effect of solar exposure. Analysis of all-age NHL incidence in the US at the level of cancer registry, with UVR assessed via data from the satellite-based Total Ozone Mapping Spectrometer (TOMS) database, documented lower incidence among those registries with higher UVR quintile for many subtypes of NHL [40]. A defect of certain of these studies [21, 23, 35] is their ecological design. In all save the French [21] and Californian [35] studies the measures of solar exposure are crude or non-existent, and many studies [36,37,38] are not confined to cancer in childhood. Latitude, which is used in many, is only a proxy for UVR exposure, in particular will not take account of local climatic factors such as cloud cover or height above sea level, which are also known to be important, and so these apparently conflicting findings are perhaps unsurprising.
The EUROSUN UVR data used by Coste et al. [21] is probably the strongest UVR measure apart from the AVGLO data employed here and in the study of Lombardi et al. [35]. The EUROSUN UVR data is satellite based, although with validating ground-based data, so contrasting with the purely ground-based AVGLO data used here. France spans approximately 41.6–51.0 degrees North in latitude, whereas the 15 states in our study cover the range of 25.8–49.0 degrees North, thereby providing us with a much wider variation in UVR irradiance.
Our finding of concentration of UVR risk for ALL among those aged 0–3 (Table 5) is not without precedent. The study of Coste et al. [21] also reported a significant interaction (p = 0.007) between UVR-associated ALL risk and age, so that only for age under 5 years was the trend significant. However, the concentration of UVR risk for NHL among those aged 0–3 (Table 5) is more novel. These findings suggest powerful factors operating soon after (or before) birth. However, like all novel findings, they require replication.
A major strength of our study is the large size, using prospectively gathered cancer status data, which is linked with an independent set of county-level solar exposure measures. The availability of a rich set of lifestyle and environmental measures, albeit ecological (measured at the level of county) is also a strength. However, we were not able to examine the UVR effect in relation to different histological subtypes of ALL/NHL with varying aetiologies. The solar exposure measurements used in our study are based on interpolated solar exposure measurements derived from a 30-year series of measurements at 215 measurement stations distributed across the contiguous 48 US states [26]. What is used here is therefore a climatic average for a region and does not take account of year-to-year variations in solar exposure. The spatial resolution, to the level of US counties is a potential limitation, although the evidence is that UVR does not vary much over even relatively large (100 km square) geographical units [41]. Solar exposure of an individual living at a specific location will exhibit much greater fluctuations than ambient variation because of differences in time spent outdoors and proximity to shade on different days throughout the year. Furthermore, the solar UVR dose absorbed by the skin (assuming that to be the relevant factor) will be further modified by the use of photoprotective agents such as hats, clothing and sunscreens. There is evidence that people tend to cover up more at lower latitudes [42], which implies that personal level exposures might be less than indicated by the ambient exposure data, suggesting a likely underestimation of the slope of the cancer-solar irradiance response. We also note that there is evidence for different use of sun protective measures amongst different racial/ethnic groups [43,44,45]. Our analyses (Supplement A Tables A5 and A6) demonstrate no evidence of socioeconomic modifiers of UVR risk. However, the variation of solar exposure from year to year in this measurement set is relatively slight [46] and climatic norms will give far more representative sunlight values for the region of interest. Given that disease counts and underlying estimates of populations in our database are available only for complete calendar years, this may not matter too much, but inevitably there will be inaccuracies in assessing exposure, even assuming it was known which solar exposure metric, UVR irradiance vs UVR cumulative radiant exposure, was the more relevant, about which information is lacking. The use of these two methods of measuring solar exposure is a novelty of our study, which has not been attempted hitherto.
It is not known what the relevant exposure period for solar exposure is likely to be for the paediatric cancers considered here. It is suspected that the relevant exposure for such cancers is very early in life, as our analysis of interaction of UVR-associated risk with age might suggest (Table 5). As such correlating with solar exposure at diagnosis, an inescapable feature of the SEER registry data is likely to be not altogether the correct thing to do. However, with paediatric cancers, and particularly ALL, most of which occur under the age of 5, one can be much more confident that the solar exposure being measured relates to the entire duration of life up to the point of development of cancer. There are some mechanistic grounds for supposing that our findings with respect to ALL can be interpreted causally. Brady et al. [47] found Signature 7 UV-related mutations were enriched among a group of aneuploid pediatric ALL cases, specifically in cases with gross chromosomal alterations, including hyperdiploid (detected in 17% of samples), near haploid (35% of samples) and iAMP21 B-ALL (46% of samples). Another possible mechanism is UV-associated immunosuppression, for which there is some evidence [48]. The interaction of ALL with the immune system is complex and many autoimmune diseases exhibit elevated risk of ALL [49]. It is also clear that ALL can inhibit the immune system [50]. The protective effects of circulating vitamin D levels on many types of cancer are reasonably well known, possibly mediated via cellular gap-junctional mechanisms [51, 52], reinforced by findings of reductions in cancer mortality following vitamin D supplementation [53] although there no effects of supplementation on cancer incidence [54, 55].
As with all other studies of solar radiation our study does not take account of population migration. In our data, solar exposure is linked to the SEER county of residence at diagnosis. The effect of this is that a proportion of the population in each area, which would be larger with increasing age, will have expected solar exposure which in the worst case, of in-migration from anywhere within the US, will correspond to the US average, so that the variation in true solar exposure (of the underlying population) between areas will be to some extent over-estimated. There will also be Berkson errors resulting from applying the group means to the individual exposures, but at least to first order the effect of these on trend estimates will again be minimal [56], although uncertainties could be underestimated [57]. That said, the great advantage of studying childhood cancers is that they occur early in life, so that the effects of population migration should not be too serious [58,59,60]. Indeed Bell and Belanger [59] reviewing the literature on residential mobility about the time of birth in various developed countries, noted explicitly that most mothers, when they move, stayed within the same county; there was little variation between countries in this respect. Another source of error is the determination of Hispanic origin in SEER. This employs an algorithm using the patient’s surname, so that misclassification of certain cases is possible. However, as such misclassification is unlikely to vary with degree of UVR exposure it will probably not introduce bias in assessments of cancer risk in relation to UVR exposure.
In summary, our findings of a protective effect of solar exposure on NHL (albeit not for ages 0–3) are generally supported by those of a number of previous, but generally lower quality, ecological studies. Our more novel finding, of an adverse effect of solar exposure on childhood ALL, is consistent with those of a large population-based study in France, but to some extent inconsistent with findings in a case-control study in California with little UVR variation [35] and lower quality ecological studies. However, the evidence is not entirely clear-cut and all findings are in need of replication, perhaps by using individual-level data, where solar exposures can be assigned more accurately.
Data availability
All data and R code used for the analysis is available via online Supplement B.
References
Office for National Statistics. Cancer Statistics Registrations, England (Series MB1), no. 41, 2010. London: Office for National Statistics; 2012.
Surveillance Epidemiology and End Results (SEER) Program (www.seer.cancer.gov). Surveillance, Epidemiology, and End Results (SEER) Program SEER*Stat Database: Incidence – SEER Research Plus Limited-Field Data, 22 Registries, Nov 2022 Sub (2000-2020) - Linked To County Attributes - Total U.S., 1969-2020 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2023, based on the November 2022 submission., Accessed 9/2023, 2023.
Linet MS, Brown LM, Mbulaiteye SM, Check D, Ostroumova E, Landgren A, et al. International long-term trends and recent patterns in the incidence of leukemias and lymphomas among children and adolescents ages 0-19 years. Int J Cancer. 2016;138:1862–74.
Kaatsch P, Steliarover-Foucher E, Crocetti E, Magnani C, Spix C, Zambon P. Time trends of cancer incidence in European children (1978-1997): report from the Automated Childhood Cancer Information System project. Eur J Cancer. 2006;42;1961–71.
Zhang Y, Dai Y, Zheng T, Ma S. Risk factors of non-Hodgkin lymphoma. Expert Opin Med Diagn. 2011;5:539–50.
United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR). UNSCEAR 2006 Report. Annex A. Epidemiological Studies of Radiation and Cancer. 13–322, United Nations: New York: UNSCEAR; 2008.
Armstrong B, Brenner DJ, Baverstock K, Cardis E, Gilmette RA, Hall J, et al. Radiation. Volume 100D. A review of human carcinogens. 1–341, Lyon, France: International Agency for Research on Cancer; 2012.
Hjalgrim LL, Westergaard T, Rostgaard K, Schmiegelow K, Melbye M, Hjalgrim H, et al. Birth weight as a risk factor for childhood leukemia: a meta-analysis of 18 epidemiologic studies. Am J Epidemiol. 2003;158:724–35.
Caughey RW, Michels KB. Birth weight and childhood leukemia: a meta-analysis and review of the current evidence. Int J Cancer. 2009;124:2658–70.
Smith A, Lightfoot T, Simpson J, Roman E. Birth weight, sex and childhood cancer: A report from the United Kingdom Childhood Cancer Study. Cancer Epidemiol. 2009;33:363–7.
O’Neill KA, Murphy MFG, Bunch KJ, Puumula SE, Carozza SE, Chow EJ, et al. Infant birthweight and risk of childhood cancer: international population-based case control studies of 40 000 cases. Int J Epidemiol. 2015;44:153–68.
Kroll ME, Stiller CA, Murphy MFG, Carpenter LM. Childhood leukaemia and socioeconomic status in England and Wales 1976-2005: evidence of higher incidence in relatively affluent communities persists over time. Br J Cancer. 2011;105:1783–7.
Wang L, Gomez SL, Yasui Y. Racial and ethnic differences in socioeconomic position and risk of childhood acute lymphoblastic leukemia. Am J Epidemiol. 2017;185:1263–71.
Kehm RD, Spector LG, Poynter JN, Vock DM, Osypuk TL. Socioeconomic status and childhood cancer incidence: a population-based multilevel analysis. Am J Epidemiol. 2018;187:982–91.
Kinlen LJ. An examination, with a meta-analysis, of studies of childhood leukaemia in relation to population mixing. Br J Cancer. 2012;107:1163–8.
Crouch S, Lightfoot T, Simpson J, Smith A, Ansell P, Roman E. Infectious illness in children subsequently diagnosed with acute lymphoblastic leukemia: modeling the trends from birth to diagnosis. Am J Epidemiol. 2012;176:402–8.
He J-R, Ramakrishnan R, Hirst JE, Bonaventure A, Francis SS, Paltiel O, et al. Maternal infection in pregnancy and childhood leukemia: a systematic review and meta-analysis. J Pediatr. 2020;217:98–109.
Cerhan JR, Vajdic CM, Spinelli JJ. The non-Hodgkin lymphomas. In: Thun MJ, Linet MS, Cerhan JR, Haiman C, Schottenfeld D & Landgren AM, editors. Cancer epidemiology and prevention. 4th edn. Ch. 40, 767–96, New York, NY: Oxford University Press: 2018.
Chow EJ, Puumula SE, Mueller BA, Carozza SE, Fox EE, Horel S, et al. Childhood cancer in relation to parental race and ethnicity: a 5-state pooled analysis. Cancer. 2010;116:3045–53.
Timonen T, Nayha S, Koskela T, Pukkala E. Are sunlight deprivation and influenza epidemics associated with the onset of acute leukemia? Haematologica. 2007;92:1553–6.
Coste A, Goujon S, Boniol M, Marquant F, Faure L, Doré J-F, et al. Residential exposure to solar ultraviolet radiation and incidence of childhood hematological malignancies in France. Cancer Causes Control. 2015;26:1339–49.
Petridou ET, Dikalioti SK, Skalkidou A, Andrie E, Dessypris N, Trichopoulos D, et al. Sun exposure, birth weight, and childhood lymphomas: a case control study in Greece. Cancer Causes Control. 2007;18:1031–7.
Musselman JR, Spector LG. Childhood cancer incidence in relation to sunlight exposure. Br J Cancer. 2011;104:214–20.
Morton LM, Turner JJ, Cerhan JR, Linet MS, Treseler PA, Clarke CA, et al. Proposed classification of lymphoid neoplasms for epidemiologic research from the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph). Blood. 2007;110:695–708.
Dores GM, Devesa SS, Curtis RE, Linet MS, Morton LM. Acute leukemia incidence and patient survival among children and adults in the United States, 2001-2007. Blood. 2012;119:34–43.
Tatalovich Z, Wilson JP, Cockburn M. A comparison of Thiessen polygon, kriging, and spline models of potential UV exposure. Cartogr Geogr Inf Sci. 2006;33:217–31.
Sliney DH, International Commission on Illumination (CIE). Radiometric quantities and units used in photobiology and photochemistry: recommendations of the Commission Internationale de L’Eclairage (International Commission on Illumination). Photochem Photobiol. 2007;83:425–32.
Little MP, Linet MS, Kimlin MG, Lee T, Tatalovich Z, Sigurdson AJ, et al. Cumulative solar ultraviolet radiation exposure and basal cell carcinoma of the skin in a nationwide US cohort using satellite and ground-based measures. Environ Health. 2019;18:114.
Little MP, Linet MS, Kimlin MG, Lee T, Tatalovich Z, Sigurdson AJ. Improving assessment of lifetime solar ultraviolet radiation exposure in epidemiologic studies: comparison of ultraviolet exposure assessment methods in a nationwide U.S. occupational cohort. Photochem Photobiol. 2018;94:1297–307.
Little MP, Lee T, Kimlin MG, Kitahara CM, Zhang R, Alexander BH, et al. Lifetime ambient UV radiation exposure and risk of basal cell carcinoma by anatomic site in a nationwide U.S. cohort, 1983-2005. Cancer Epidemiol Biomark Prev. 2021;30:1932–46.
McCullagh P, Nelder JA. Generalized linear models. 2nd ed. 1–526, Boca Raton, FL: Chapman and Hall/CRC; 1989.
R: a language and environment for statistical computing. version 3.6.1 https://www.r-project.org. Vienna, Austria: R Foundation for Statistical Computing; 2019.
Akaike H. Information theory and an extension of the maximum likelihood principle. In: Petrov BN & Czáki F, editors. 2nd International Symposium on Information Theory. 267–81. Budapest: Akadémiai Kiadó; 1973.
Akaike H. Likelihood of a model and information criteria. J Econ. 1981;16:3–14.
Lombardi C, Heck JE, Cockburn M, Ritz B, Solar UV. radiation and cancer in young children. Cancer Epidemiol Biomark Prev. 2013;22:1118–28.
Grant WB. An ecologic study of cancer mortality rates in Spain with respect to indices of solar UVB irradiance and smoking. Int J Cancer. 2007;120:1123–8.
Kim H-B, Kim J-H. Sunlight exposure in association with risk of lymphoid malignancy: a meta-analysis of observational studies. Cancer Causes Control. 2021;32:441–57.
Lu D, Xu F, Hu K, Yin L, Duan H, Zhang J, et al. Occupational ultraviolet exposure and risk of non-Hodgkin’s lymphomas: a meta-analysis. Oncotarget. 2017;8:62358–70.
Kricker A, Armstrong BK, Hughes AM, Goumas C, Smedby KE, Zheng T, et al. Personal sun exposure and risk of non Hodgkin lymphoma: a pooled analysis from the Interlymph Consortium. Int J Cancer. 2008;122:144–54.
Cahoon EK, Pfeiffer RM, Wheeler DC, Arhancet J, Lin S-W, Alexander BH, et al. Relationship between ambient ultraviolet radiation and non-Hodgkin lymphoma subtypes: a U.S. population-based study of racial and ethnic groups. Int J Cancer. 2015;136:E432–E441.
Grant RH, Slusser JR. Spatial variability in UV radiation during the growing season across the continental USA. Theor Appl Climatol. 2003;74:167–77.
Sun J, Lucas RM, Harrison S, van der Mei I, Armstrong BK, Nowak M, et al. The relationship between ambient ultraviolet radiation (UVR) and objectively measured personal UVR exposure dose is modified by season and latitude. Photochem Photobiol Sci. 2014;13:1711–8.
Andreeva VA, Unger JB, Yaroch AL, Cockburn MG, Baezconde-Garbanati L, Reynolds KD. Acculturation and sun-safe behaviors among US Latinos: findings from the 2005 Health Information National Trends Survey. Am J Public Health. 2009;99:734–41.
Andreeva VA, Cockburn MG, Yaroch AL, Unger JB, Rueda R, Reynolds KD. Preliminary evidence for mediation of the association between acculturation and sun-safe behaviors. Arch Dermatol. 2011;147:814–9.
Linos E, Keiser E, Kanzler M, Sainani KL, Lee W, Vittinghoff E, et al. Sun protective behaviors and vitamin D levels in the US population: NHANES 2003-2006. Cancer Causes Control. 2012;23:133–40.
Tatalovich Z. Personal communication to MP Little 8/2017. 2017.
Brady SW, Roberts KG, Gu Z, Shi L, Pounds S, Pei D, et al. The genomic landscape of pediatric acute lymphoblastic leukemia. Nat Genet. 2022;54:1376–89.
González Maglio DH, Paz ML, Leoni J. Sunlight effects on immune system: is there something else in addition to UV-induced immunosuppression? BioMed Res Int. 2016;1934518:1-10.
Linet MS, Morton LM, Devesa SS, Dores GM. Leukemias. In Thun MJ, Linet MS, Cerhan JR, Haiman C, Schottenfeld D & Landgren AM, editors. Cancer epidemiology and prevention. 4th ed. Ch. 38, 715–44. New York, NY: Oxford University Press; 2018.
Pastorczak A, Domka K, Fidyt K, Poprzeczko M, Firczuk M. Mechanisms of immune evasion in acute lymphoblastic leukemia. Cancers. 2021;13:1536.
Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, et al. The role of vitamin D in cancer prevention. Am J Public Health. 2006;96:252–61.
McCullough ML, Zoltick ES, Weinstein SJ, Fedirko V, Wang M, Cook NR, et al. Circulating vitamin D and colorectal cancer risk: an international pooling project of 17 cohorts. J Natl Cancer Inst. 2019;111:158–69.
Manson JE, Bassuk SS, Buring JE, VITAL Research Group. Principal results of the VITamin D and OmegA-3 TriaL (VITAL) and updated meta-analyses of relevant vitamin D trials. J Steroid Biochem Molec Biol. 2020;198:105522.
Manson JE, Cook NR, Lee I-M, Christen W, Bassuk SS, Mora S, et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med. 2019;380:33–44.
Scragg RKR. Overview of results from the Vitamin D Assessment (ViDA) study. J Endocrinol Invest. 2019;42:1391–9.
Carroll RJ, Ruppert D, Stefanski LA, Crainiceanu CM. Measurement error in nonlinear models. A modern perspective. 1–488, Boca Raton, FL: Chapman and Hall/CRC; 2006.
Zhang Z, Preston DL, Sokolnikov M, Napier BA, Degteva M, Moroz B, et al. Correction of confidence intervals in excess relative risk models using Monte Carlo dosimetry systems with shared errors. PloS One. 2017;12:e0174641.
Kendall GM, Wakeford R, Bunch KJ, Vincent TJ, Little MP. Residential mobility and associated factors in relation to the assessment of exposure to naturally occurring radiation in studies of childhood cancer. J Radiol Prot. 2015;35:835–68.
Bell ML, Belanger K. Review of research on residential mobility during pregnancy: consequences for assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol. 2012;22:429–38.
Nikkilä A, Kendall G, Raitanen J, Spycher B, Lohi O, Auvinen A. Effects of incomplete residential histories on studies of environmental exposure with application to childhood leukaemia and background radiation. Environ Res. 2018;166:466–72.
Acknowledgements
The authors are grateful for the detailed and helpful comments of Drs Sara Schonfeld, Lindsay Morton, Zaria Tatalovich, Professor Brian Diffey and the two referees. This work was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Division of Cancer Epidemiology and Genetics. MGK was supported through a Cancer Council Queensland (Australia) Chair in Cancer Prevention position.
Author information
Authors and Affiliations
Contributions
MPL was responsible for designing the study protocol, performing the main statistical analysis and writing the first MS draft. JZM was responsible for preparing the preliminary primary SEER analysis dataset. VK was responsible for preparation of the AVGLO and other county-level variable dataset. All authors contributed to and approved successive drafts of the MS.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The data used is taken from the SEER registry, which has no personal identifying information, and therefore ethical approval and informed consent is not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Little, M.P., Mai, J.Z., Fang, M. et al. Solar ultraviolet radiation exposure, and incidence of childhood acute lymphocytic leukaemia and non-Hodgkin lymphoma in a US population-based dataset. Br J Cancer (2024). https://doi.org/10.1038/s41416-024-02629-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41416-024-02629-3