Abstract
Background
Insulin resistance is a hypothesised biological mechanism linking obesity with prostate cancer (PCa) death. Data in support of this hypothesis is limited.
Methods
We included 259,884 men from eight European cohorts, with 11,760 incident PCa’s and 1784 PCa deaths during follow-up. We used the triglyceride-glucose (TyG) index as indicator of insulin resistance. We analysed PCa cases with follow-up from PCa diagnosis, and the full cohort with follow-up from the baseline cancer-free state, thus incorporating both PCa incidence and death. We calculated hazard ratios (HR) and the proportion of the total effect of body mass index (BMI) on PCa death mediated through TyG index.
Results
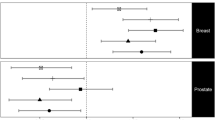
In the PCa-case-only analysis, baseline TyG index was positively associated with PCa death (HR per 1-standard deviation: 1.11, 95% confidence interval (CI); 1.01–1.22), and mediated a substantial proportion of the baseline BMI effect on PCa death (HRtotal effect per 5-kg/m2 BMI: 1.24; 1.14–1.35, of which 28%; 4%–52%, mediated). In contrast, in the full cohort, the TyG index was not associated with PCa death (HR: 1.03; 0.94-1.13), hence did not substantially mediate the effect of BMI on PCa death.
Conclusions
Insulin resistance could be an important pathway through which obesity accelerates PCa progression to death.
Similar content being viewed by others
Introduction
The association of obesity with prostate cancer (PCa) incidence and death is double-edged. Obesity is associated with lower risk of diagnosis of low-risk, commonly screen-detected PCa, but is not associated with the risk of more advanced PCa [1,2,3,4,5,6,7]. In contrast, obesity has consistently been associated with worse PCa prognosis and PCa-specific death [1, 3,4,5, 8,9,10,11,12,13,14,15,16,17], but the mechanisms underlying these associations remain unclear. One possible mechanism is that less effective PCa treatment of obese men results in a higher risk of disease recurrence [1, 18, 19], but biological mechanisms may also be in action [1, 8, 20,21,22]. In support of biological mechanisms is the fact that obesity is associated with an increased risk of PCa progression and death also when studying only low-risk PCa’s [3, 23]; findings which are less likely to be affected by curative and palliative treatment.
Insulin resistance and the resulting hyperinsulinemia is one potential biological pathway connecting obesity with progression and death from PCa [1]. Whilst hyperinsulinemia has not been associated with the diagnosis of PCa in prospective cohort studies [24, 25], there is evidence for its involvement in PCa progression and death [26, 27]. For example, in the Physicians’ Health Study, plasma concentrations of prediagnostic C-peptide – a robust marker of plasma insulin levels - were positively associated with higher PCa-specific mortality [26].
The product of fasting triglyceride and glucose levels (triglyceride-glucose [TyG] index) is a simple measure of insulin resistance [28]. It correlates well with the euglycemic-hyperinsulinemic clamp test, the gold standard for determining insulin resistance, and has validity similar to the frequently used homoeostatic model assessment insulin resistance index [29]. Both lipotoxicity and glucotoxicity play crucial roles in insulin resistance modulation, and both are reflected in the TyG index [30, 31].
Prospective epidemiological studies quantifying (i) the association of insulin resistance and death from PCa, and (ii) how much of the effect of obesity on higher risk of PCa death is mediated through insulin resistance are lacking. This study aimed at estimating these quantities using body mass index (BMI) and TyG index measurements in pooled data of eight European population-based cohorts.
Materials and methods
Study population
This study pooled data from four Swedish, three Norwegian, and one Austrian population-based cohorts. Information was obtained from health examinations, performed between 1972 and 2016, including height and weight as measured by medical staff, glucose and triglyceride values from blood draws, and questionnaire-assessed smoking status. The study was approved by research ethics committees in the respective countries. Further details on the cohorts can be found in the Supplementary Information, Supplementary Materials and Methods.
Follow-up and endpoint assessment
To obtain information on cancer diagnoses, date and cause of death, and date of emigration (not available for the Austrian cohort), each cohort was linked to the respective national Cancer Register, Cause of Death Register, and Population Register. Study participants were followed until emigration, death, or end of study (2012 for the Norwegian, 2014 for the Austrian, and 2016 for the Swedish cohorts). PCa cases were identified in the cancer registers using International Classification of Diseases, version 7 code 177 and/or ICD-10 code C61. For the Swedish cohorts, additional linkages of the data with the Longitudinal Integration Database for Health Insurance and Labour Market Studies (LISA), the Patient Register, and the National Prostate Cancer Register (NPCR) were performed (see also Supplementary Information, Supplementary Materials and Methods).
Exclusions
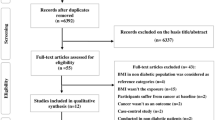
From the original dataset, observations were excluded for a variety of reasons, including men with inconsistencies in cancer and death dates and/or a cancer diagnosis occurring before the baseline visit (except non-melanoma skin cancer), visits with incomplete, inconsistent, or implausible reporting, and visits occurring before the age of 21. After exclusions, 259,884 out of originally 431,525 men were left for our final analysis population (Figure S1). The vast majority of these exclusions were due to missing information on glucose levels in the Norwegian cohorts during years when it had not been routinely measured. Additional details are provided in the Supplementary Information, Supplementary Materials and Methods.
Statistical analysis
Exposure (BMI) and mediator (TyG index) values were taken from each man’s baseline visit. BMI was calculated as [weight (kg)/height (m)2], and the TyG index as ln[triglycerides (mg/dl) × blood glucose (mg/dl)/2] [28]. TyG index values were standardised (z-transformed) separately for cohort and fasting status (<8 h vs. ≥8 h) to account for effects of fasting state and cohort-specific differences, such as analytical methods. Tests of interaction between BMI and cohort, and TyG index and cohort, did not indicate differential associations with PCa death across cohorts, supporting the pooling of data from all cohorts.
The association between the TyG index (both as a linear term and in quartiles) and PCa incidence and death was modelled using Cox proportional hazards regression. To assess mediation of the effect of BMI on PCa death through the TyG index, we applied the two-stage regression method for survival data by VanderWeele [32]. In brief, two regression models were fit to the data, one modelling the mediator and the other modelling the outcome; parameter estimates of these two separate models were combined to obtain effect estimates of mediation. We modelled the outcome (PCa death) using Cox proportional hazards regression models, and the mediator (TyG index) using linear regression models. All these analyses were performed both on the full, initially cancer-free population, using attained age (left-truncated at the baseline examination) as the underlying time variable, and on PCa cases only, using time from PCa diagnosis to PCa-specific death as the time variable. Analogous mediation analyses using BMI categories instead of continuous BMI were performed. All models were stratified on cohort and birth decade (≤1929/1930-1939/1940-1949/1950-1959/1960-1969/ ≥ 1970), and adjusted for age at baseline (full cohort analysis), age at diagnosis (PCa-case only analysis), smoking status, and fasting status. In analyses of men included in the Swedish NPCR, further adjustments were made for country of birth, educational level, income, source of income, civil status, and Charlson comorbidity index [33] closest to the time of diagnosis, primary treatment for prostate cancer, and prostate cancer risk category. We found no interaction between BMI and TyG index on risk of PCa death; thus, no such interaction terms were added to the models.
Assuming causal relationships between variables as shown in the directed acyclic graph in Fig. 1, and under the assumption that we accounted for the majority of confounding, VanderWeele’s method [32] decomposes the total effect of BMI on PCa death (expressed as the hazard ratio (HR) per 5-kg/m2 increase in BMI, or as the HR vs. the reference <25 kg/m2 for BMI categories) into two components: the natural indirect effect (i.e. the effect of BMI that is due to mediation through the TyG index), and the natural direct effect (i.e. the effect of BMI not explained through the mediator) [32]. Since the question of mediation is of an intrinsically causal nature, we used the term “effect” in this context [34], even though our analysis is based on observational data. The proportion of the total effect of BMI on PCa death mediated through the TyG index (in %) was calculated on the log-transformed HR scale as log(indirect effect HR)/log(total effect HR) × 100, since HRs are additive on this scale. 95% confidence intervals (CIs) for estimates of the total, natural indirect, and natural direct effects and the proportion mediated were calculated based on standard errors (SEs) derived from the delta method.
Dotted arrows represent confounding pathways, whereas the other arrows (solid [direct effect of body mass index] and dashed [indirect effect via mediator TyG index]), due to their unidirectionality, can convey exposure effects to the outcome, and are thus causal pathways. 1Only available for Swedish men. 2The case-only analysis of time from PCa diagnosis to PCa-specific death is sensitive to when the tumour was diagnosed (“PCa detection time”). Delayed detection of PCa is more likely in obese compared to normal weight men [1, 3, 40]. Therefore, for the case-only analysis, PCa detection time can be seen as a subcomponent of the direct effect. However, delayed detection of PCa in obese men can also be interpreted as an instance of detection bias. Assuming that clinical tumour characteristics are an indicator of the detection time of the PCa, the influence of this bias can be mitigated by adjusting for clinical tumour characteristics, as has been done in secondary analyses in Swedish NPCR cases, for whom this information was available. PCa – prostate cancer.
As parameter (β) estimates from regression models might be diluted by random measurement error and long-term intra-individual fluctuations, we calculated regression dilution ratios (RDRs) for BMI and the TyG index, and corrected β estimates of all regression models (including those from the mediation models) by dividing the original values by the RDR. Consequently, for HRs from Cox regression models, the correction formula was \({{HR}}_{{corrected}}=\exp (\log \left({{HR}}_{{original}}\right)/{RDR})\). RDRs were calculated using linear mixed effects models as described by Wood et al. using all available repeated measurements in our cohorts [35, 36]. Details about the obtained RDRs and a comparison of characteristics of men with vs. without repeated measurements are shown in Figure S2 and Table S1, respectively.
RDRs were calculated using the user-written function “rdrcalc” (see https://www.phpc.cam.ac.uk/ceu/erfc/programmes/) using Stata SE, version 17.0. All other analyses were conducted in R, version 4.0.5 (R Foundation).
Results
Study population
Out of 259,884 study participants, 111,168 (42.8%) men originated from Norway, 80,098 (30.8%) from Austria, and 68,618 (26.4%) from Sweden. The mean age at baseline was 43.3 [standard deviation (SD) 10.1] years. More than half of the population was either overweight (43.6%) or obese (10.9%). Mean (SD) values of glucose (mmol/l), triglycerides (mmol/l) and the TyG index {ln[mg2/(2*dl2)]} were 5.3 (1.3), 1.8 (1.3), and 8.8 (0.6), respectively. Over a median follow-up time of 17.5 years, equalling a total of 5,150,512 person-years, 11,760 men were diagnosed with PCa, of whom 1784 died from the disease (Table 1; Table S2 for stratification by country). Among the 4101 Swedish PCa cases, 3820 (93.1%) were identified in the NPCR. Clinical characteristics for men in the NPCR are presented in Table S3.
Associations of TyG index with baseline characteristics and death from PCa
Mean baseline BMI and age, and the prevalence of smoking, increased across TyG index quartiles, while the number of PCa diagnoses was similar across quartiles (Table 1). The correlation of BMI with the TyG index remained after adjusting for cohort, birth decade, age, smoking, and fasting status (partial Pearson correlation ρ = 0.35).
In case-only analyses, the TyG index was positively associated with time from PCa diagnosis to PCa-specific death (HR1-SD increase in TyG index = 1.11, 95% CI: 1.01–1.22) (Table 2). Analysing the TyG index categorised into quartiles confirmed a roughly linear relationship. The association became more pronounced when restricting the analysis to PCa cases with blood drawn in the fasting state (HR = 1.27, 95% CI: 1.12–1.44). The results did not change substantially when assessing only TyG index values measured at most 10 years prior to PCa diagnosis (HR = 1.15, 95% CI: 0.99–1.33), and when additionally adjusting for PCa risk category and other clinical characteristics in the NPCR cases.
In contrast, in the full cohort analysis the association between TyG index and PCa-specific death was much weaker (HR1-SD increase in TyG index = 1.03, 95% CI: 0.94–1.13), although exclusion of non-fasting samples made the association stronger (HR = 1.13, 95% CI: 1.00–1.29) (Table 2). Notably, the TyG index was slightly negatively associated with PCa incidence (0.96, 95% CI: 0.93–1.00).
Effect of BMI on death from PCa mediated through the TyG index
Analysing time since PCa diagnosis in PCa cases only, BMI was positively associated with the risk of PCa death (HRtotal effect = 1.24 per 5-kg/m2 increase in BMI, 95% CI: 1.14–1.35). Of this total effect, 28% (95% CI: 4%–52%) were mediated through the TyG index (HRindirect effect = 1.06, 95% CI: 1.01–1.12) (Table 3; Table S4 for RDR-uncorrected results). The proportion increased to 54% (95% CI: 22%–85%) when analysing fasting blood samples only. Analysis by BMI categories yielded a total effect HR of 1.13 (95% CI: 1.02–1.25) for overweight vs. normal weight, and a total effect HR of 1.59 (95% CI: 1.34–1.89) for obese men. Proportions mediated through the TyG index were 42% for overweight (HRindirect effect = 1.05; 95% CI: 1.01–1.10), and 22% for obesity (HRindirect effect = 1.11; 95% CI: 1.02–1.21). Assessing only BMI and TyG index values measured at most 10 years prior to PCa diagnosis, and further adjustment by PCa risk category and other clinical characteristics for Swedish men in the NPCR did not materially change the effects (Table 3).
Analysing age at PCa death in the full cohort, associations of BMI with PCa death were slightly weaker than in the case-only analyses (HRtotal effect = 1.17, 95% CI: 1.08–1.27). Only 11% (95% CI: −21%–42%) of this total effect [38% (95% CI: −1%–77%) for fasting samples only], and thus a markedly smaller proportion than for the PCa-case only analysis, were mediated through the TyG index (HRindirect effect, total = 1.02, 95% CI: 0.97–1.07; HRindirect effect, fasting samples only = 1.07; 95% CI: 1.00–1.14) (Table 4).
Discussion
In this large, pooled analysis of eight population-based European cohorts, higher TyG index was associated with a shorter time from PCa diagnosis to PCa-specific death, and more than a quarter of the total effect of BMI on PCa-specific death was mediated through the TyG index. In the full cohort followed from a cancer-free state through PCa diagnosis and death, there was neither an association of the TyG index with PCa-specific death, nor did the TyG index substantially mediate the effect of BMI on PCa death. These results suggest that insulin resistance, as reflected by the TyG index, may substantially mediate the effect of BMI on PCa progression to death, but not a diagnosis of PCa.
The different findings in the analysis of PCa cases who were followed from time of diagnosis as compared to the analysis of the full cohort followed from baseline throughout the follow-up period, both commonly applied approaches, warrant further discussion. The results from the full cohort analysis reflect the association of obesity with a mix of time until PCa diagnosis and PCa-specific death. The second component is of primary interest in the study of PCa progression and survival, and was directly studied in our case-only analysis. Importantly, obesity and insulin resistance are hypothesised to be more involved during the progression of PCa [1, 17, 20]. Our finding that the proportion of the effect of baseline BMI on PCa death mediated through the TyG index is more pronounced in the case-only analysis compared to the full cohort analysis supports this hypothesis. This interpretation was further corroborated by the analysis of data measured up to ten years prior to PCa diagnosis. However, the relationship of BMI and TyG index measured at the time of PCa diagnosis, together with changes from baseline, with PCa-specific death should be investigated in future studies.
While time from diagnosis to PCa-specific death was studied directly in the case-only analysis, this analysis might be affected by collider stratification bias inherent to the analysis of cases only [37,38,39]. However, for collider bias to influence our findings, an association between TyG index and incident PCa would be required and this association was weak in our data. The case-only analysis might also be affected by detection bias resulting in a differential exposure association with indolent and advanced PCa at diagnosis, which has been observed for BMI [1, 3, 40]. Delayed diagnosis of PCa is more likely in obese compared to normal weight men because of hemodiluted prostate-specific antigen (PSA) levels and enlarged prostate glands, and possibly lower frequency of asymptomatic PSA testing in obese men [1, 3, 40]. In analyses of cases in the NPCR of Sweden, we were able to mitigate the potential influence of differential detection time by adjusting the statistical models for PCa risk category and other clinical characteristics. However, these additional adjustments did not materially change the results, which validates the unadjusted results of our extended pooling.
In addition to epidemiological studies, which have shown that insulin resistance is associated with PCa progression and PCa-specific death [26, 27], there is also evidence from preclinical and mechanistic studies of the importance of insulin resistance in PCa progression. For example, increased numbers of insulin receptors on the cell membranes of high grade compared to low grade prostate tumours have been observed [41]. Another study reported an increased expression of the insulin receptor A isoform in high grade PCa cells in vitro and in vivo [42]. Diet-induced hyperinsulinemia was associated with PCa tumour growth in a xenograft model [43]. Finally, a relatively recent study reported that insulin made PCa cells in vitro more invasive and mobile [44]. However, a large proportion of the BMI effect was not mediated through the TyG index in our study. Although unaccounted measurement error and confounding might have led to an underestimation of the indirect effect, other important mechanisms are likely to be in action. Other mechanisms for which the presence of mediation should be studied as well include (i) alterations in sex hormone metabolism, in particular androgen deficiency [1, 45, 46], (ii) chronic inflammation characterised by altered levels of adipokines in obese men [17, 47, 48], and (iii) less successful treatment in obese men with associated higher rates of disease recurrence [1, 18, 19]. In general, proportions mediated through the TyG index appeared to be larger for overweight than for obesity in our analyses. This observation might be explained by the sometimes expressed claim that overweight per se is not as intrinsically bad as obesity, and exerts its detrimental effects to a higher extent via metabolic pathways, compared to obesity, where other pathways, such as neurohumoral or hemodynamic dysregulations, are additional relevant contributors [49, 50].
One limitation of our study was that we only had measures of BMI and TyG index. Those are only surrogate measures of excess body fatness and insulin resistance, the conditions that are believed to be the biological link to PCa death. Furthermore, the precision of the TyG index may be reduced when measured in the non-fasting state. This would dilute the association and explain why the proportion of the effect of BMI on PCa death risk mediated through the TyG index was markedly smaller when analysing all men compared to analysing only samples from fasting men. However, systematic differences across cohorts might be another reason, since men with non-fasting samples originated primarily from the Norwegian cohorts. Furthermore, BMI and the TyG index were measured at the same time in point, while ideally the exposure BMI should be measured prior to the mediator TyG index. However, BMI is a very stable measure over the observation period of our study population (RDR = 0.924), so the simultaneous measurement of BMI and TyG index probably does not substantially affect our findings, in particular because we corrected our analyses for the RDR. Another direct limitation of observational research is that we cannot rule out the possibility of unmeasured and/or residual confounding.
Strengths of our study include the large sample size and long follow-up, the use of high-quality national cancer registers ensuring a virtually complete capture of cancer cases [51,52,53], detailed and validated cancer characteristics for a large proportion of the Swedish PCa cases [54], and the availability of repeated measurements to account for random measurement error and intra-individual fluctuations in BMI and TyG index values. Notably, mediation analysis corrected for the RDR (Tables 3, 4) showed that the proportion of the effect of BMI on PCa death risk mediated through the TyG index was underestimated by 10% to 15% in uncorrected analysis (Table S4), in line with previous studies [35, 36, 55].
In summary, in PCa-case only analyses the TyG index was positively associated with PCa-specific death, and more than a quarter of the effect of BMI on PCa death was mediated through the TyG index. The contribution of the TyG index as a mediator to the effect of BMI on PCa-specific death in the full cohort was much smaller, because, in contrast to PCa death, the TyG index was slightly negatively associated with PCa incidence. As the TyG index is indicative of insulin resistance, our findings support a role for insulin in promoting PCa progression. Our results provide further evidence of the importance of avoiding excess weight and maintaining a healthy metabolic profile, and adds to the rationale for investigating novel treatment strategies for PCa targeting insulin resistance as an adjuvant therapy for PCa.
Data availability
The data that support the findings of this study are available from cohort committees and national registers of the cohorts and countries involved. Restrictions apply to the availability of these data, which were used under license for this study. Data are available after contact with the corresponding author conditional on permission from the involved cohort committees and national registers.
References
Allott EH, Masko EM, Freedland SJ. Obesity and prostate cancer: weighing the evidence. Eur Urol. 2013;63:800–9.
Fang X, Wei J, He X, Lian J, Han D, An P, et al. Quantitative association between body mass index and the risk of cancer: a global Meta-analysis of prospective cohort studies. Int J Cancer. 2018;143:1595–603.
Jochems SHJ, Stattin P, Häggström C, Järvholm B, Orho-Melander M, Wood AM, et al. Height, body mass index and prostate cancer risk and mortality by way of detection and cancer risk category. Int J Cancer. 2020;147:3328–38.
Shi J, Zhao L, Gao Y, Niu M, Yan M, Chen Y, et al. Associating the risk of three urinary cancers with obesity and overweight: an overview with evidence mapping of systematic reviews. Syst Rev. 2021;10:58.
Genkinger JM, Wu K, Wang M, Albanes D, Black A, van den Brandt PA, et al. Measures of body fatness and height in early and mid-to-late adulthood and prostate cancer: risk and mortality in the pooling project of prospective studies of diet and cancer. Ann Oncol. 2020;31:103–14.
Kyrgiou M, Kalliala I, Markozannes G, Gunter MJ, Paraskevaidis E, Gabra H, et al. Adiposity and cancer at major anatomical sites: umbrella review of the literature. BMJ. 2017;356:j477.
Davies NM, Gaunt TR, Lewis SJ, Holly J, Donovan JL, Hamdy FC, et al. The effects of height and BMI on prostate cancer incidence and mortality: a Mendelian randomization study in 20,848 cases and 20,214 controls from the PRACTICAL consortium. Cancer Causes Control. 2015;26:1603–16.
Cantarutti A, Bonn SE, Adami H-O, Grönberg H, Bellocco R, Bälter K. Body mass index and mortality in men with prostate cancer. Prostate. 2015;75:1129–36.
Zhong S, Yan X, Wu Y, Zhang X, Chen L, Tang J, et al. Body mass index and mortality in prostate cancer patients: a dose-response meta-analysis. Vol. 19, Prostate cancer and prostatic diseases. Nature Publishing Group; 2016. p. 122–31.
Troeschel AN, Hartman TJ, Jacobs EJ, Stevens VL, Gansler T, Flanders WD, et al. Postdiagnosis body mass index, weight change, and mortality from prostate cancer, cardiovascular disease, and all causes among survivors of nonmetastatic prostate cancer. J Clin Oncol. 2020;38:2018.
Rivera-Izquierdo M, Pérez de Rojas J, Martínez-Ruiz V, Pérez-Gómez B, Sánchez M-J, Khan KS, et al. Obesity as a risk factor for prostate cancer mortality: a systematic review and dose-response meta-analysis of 280,199 patients. Cancers. 2021;13:4169.
Hu MB, Xu H, Bai PD, Jiang HW, Ding Q. Obesity has multifaceted impact on biochemical recurrence of prostate cancer: a dose-response meta-analysis of 36,927 patients. Med Oncol. 2014;31:89.
Chalfin HJ, Lee SB, Jeong BC, Freedland SJ, Alai H, Feng Z, et al. Obesity and long-term survival after radical prostatectomy. J Urol. 2014;192:1100–4.
Vidal AC, Howard LE, Sun SX, Cooperberg MR, Kane CJ, Aronson WJ, et al. Obesity and prostate cancer-specific mortality after radical prostatectomy: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. Prostate Cancer Prostatic Dis. 2017;20:72–8.
Rodriguez C, Patel AV, Calle EE, Jacobs EJ, Chao A, Thun MJ. Body mass index, height, and prostate cancer mortality in two large cohorts of adult men in the United States. Cancer Epidemiol Biomark Prev. 2001;10:345–53.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl J Med. 2003;348:1625–38.
Cao Y, Ma J. Body mass index, prostate cancer-specific mortality, and biochemical recurrence: a systematic review and meta-analysis. Cancer Prev Res Cancer Prev Res (Philos). 2011;4:486–501.
Abufaraj M, Mari A, Mansy K, Sievert K. Obesity and its implications on oncological urological surgery. Curr Opin Urol. 2017;27:446–55. Sep 1
Knipper S, Mazzone E, Mistretta F, Palumbo C, Tian Z, Briganti A, et al. Impact of obesity on perioperative outcomes at robotic-assisted and open radical prostatectomy: results from the national inpatient sample. Urology. 2019;133:135–44.
Freedland S, Mucci L. Prostate cancer: Is active surveillance safe for obese patients? Nat Rev Urol. 2014;11:489–90.
Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4:579–91.
Renehan AG, Zwahlen M, Egger M. Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer. 2015;15:484–98.
Bhindi B, Kulkarni G, Finelli A, Alibhai S, Hamilton R, Toi A, et al. Obesity is associated with risk of progression for low-risk prostate cancers managed expectantly. Eur Urol. 2014;66:841–8.
Guo ZL, Weng XT, Chan FL, Gong LL, Xiang ST, Gan S, et al. Serum C-peptide concentration and prostate cancer: a meta-analysis of observational studies. Medicine. 2018;97:e11771.
Saboori S, Rad EY, Birjandi M, Mohiti S, Falahi E .Serum insulin level, HOMA-IR and prostate cancer risk: a systematic review and meta-analysis. Vol. 13, Diabetes and metabolic syndrome: clinical research and reviews. Elsevier Ltd; 2019. p. 110–5.
Ma J, Li H, Giovannucci E, Mucci L, Qiu W, Nguyen P, et al. Prediagnostic body-mass index, plasma C-peptide concentration, and prostate cancer-specific mortality in men with prostate cancer: a long-term survival analysis. Lancet Oncol. 2008;9:1039–47.
Hammarsten J, Högstedt B. Hyperinsulinaemia: a prospective risk factor for lethal clinical prostate cancer. Eur J Cancer. 2005;41:2887–95.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6:299–304.
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MG, Hernández-González SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95:3347–51.
Er L-K, Wu S, Chou H-H, Hsu L-A, Teng M-S, Sun Y-C, et al. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS One. 2016;11:e0149731.
Fritz J, Bjørge T, Nagel G, Manjer J, Engeland A, Häggström C, et al. The triglyceride-glucose index as a measure of insulin resistance and risk of obesity-related cancers. Int J Epidemiol. 2020;49:193–204.
VanderWeele TJ. Causal mediation analysis with survival data. Epidemiology. 2011;22:582–5.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Hernán MA. The C-word: scientific euphemisms do not improve causal inference from observational data. Am J Public Health. 2018;108:616–9.
Studies Collaboration Fibrinogen. Regression dilution methods for meta-analysis: assessing long-term variability in plasma fibrinogen among 27 247 adults in 15 prospective studies. Int J Epidemiol. 2006;35:1570–8.
Wood AM, Thompson SG, Kostis JB, Wilson AC, Wu K, Benderly M, et al. Correcting for multivariate measurement error by regression calibration in meta-analyses of epidemiological studies. Stat Med. 2009;28:1067–92.
Cespedes Feliciano EM, Prentice RL, Aragaki AK, Neuhouser ML, Banack HR, Kroenke CH, et al. Methodological considerations for disentangling a risk factor’s influence on disease incidence versus postdiagnosis survival: the example of obesity and breast and colorectal cancer mortality in the Women’s Health Initiative. Int J Cancer. 2017;141:2281–90.
Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15:615–25.
Banack HR, Kaufman JS. The “Obesity Paradox” Explained. Epidemiology. 2013;24:461–2.
Wallner LP, Morgenstern H, McGree ME, Jacobson DJ, St Sauver JL, Jacobsen SJ, et al. The effects of body mass index on changes in prostate-specific antigen levels and prostate volume over 15 years of follow-up: implications for prostate cancer detection. Cancer Epidemiol Biomark Prev. 2011;20:501–8.
Cox M, Gleave M, Zakikhani M, Bell R, Piura E, Vickers E, et al. Insulin receptor expression by human prostate cancers. Prostate. 2009;69:33–40.
Perks C, Zielinska H, Wang J, Jarrett C, Frankow A, Ladomery M, et al. Insulin receptor isoform variations in prostate cancer cells. Front Endocrinol. 2016;7:132.
Venkateswaran V, Haddad AQ, Fleshner NE, Fan R, Sugar LM, Nam R, et al. Association of diet-induced hyperinsulinemia with accelerated growth of prostate cancer (LNCaP) xenografts. J Natl Cancer Inst. 2007;99:1793–800.
Sarkar PL, Lee W, Williams ED, Lubik AA, Stylianou N, Shokoohmand A, et al. Insulin enhances migration and invasion in prostate cancer cells by up-regulation of FOXC2. Front Endocrinol. 2019;10:481.
Schnoeller T, Jentzmik F, Rinnab L, Cronauer M, Damjanoski I, Zengerling F, et al. Circulating free testosterone is an independent predictor of advanced disease in patients with clinically localized prostate cancer. World J Urol. 2013;31:253–9.
Michaud JE, Billups KL, Partin AW. Testosterone and prostate cancer: an evidence-based review of pathogenesis and oncologic risk. Ther Adv Urol. 2015;7:378–87.
Li H, Stampfer MJ, Mucci L, Rifai N, Qiu W, Kurth T, et al. A 25-year prospective study of plasma adiponectin and leptin concentrations and prostate cancer risk and survival. Clin Chem. 2010;56:34–43.
Stark J, Li H, Kraft P, Kurth T, Giovannucci E, Stampfer M, et al. Circulating prediagnostic interleukin-6 and C-reactive protein and prostate cancer incidence and mortality. Int J cancer. 2009;124:2683–9.
Afzal S, Tybjærg-Hansen A, Jensen GB, Nordestgaard BG. Change in body mass index associated with lowest mortality in Denmark, 1976-2013. JAMA. 2016;315:1989.
Smith GI, Mittendorfer B, Klein S. Metabolically healthy obesity: facts and fantasies. J Clin Invest. 2019;129:3978–89.
Barlow L, Westergren K, Holmberg L, Tälback M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48:27–33.
Larsen IK, Småstuen M, Johannesen TB, Langmark F, Parkin DM, Bray F, et al. Data quality at the Cancer Registry of Norway: an overview of comparability, completeness, validity and timeliness. Eur J Cancer. 2009;45:1218–31.
Hackl M, Waldhoer T. Estimation of completeness of case ascertainment of Austrian cancer incidence data using the flow method. Eur J Public Health. 2013;23:889–93.
Tomic K, Sandin F, Wigertz A, Robinson D, Lambe M, Stattin P. Evaluation of data quality in the National Prostate Cancer Register of Sweden. Eur J Cancer. 2015;51:101–11.
Wormser D, Wood AM, Di Angelantonio E, Thompson SG, Danesh J. Metabolic mediators of body-mass index and cardiovascular risk. Lancet. 2014;383:2042–3.
Acknowledgements
We thank all participants of the cohorts. We thank the Biobank Research Unit at Umeå University, the Västerbotten Intervention Programme, the Northern Sweden MONICA study and the County Council of Västerbotten for providing data, and acknowledge the contribution of Biobank Sweden, supported by the Swedish Research Council (VR 2017- 00650). We also thank Anders Dahlin, database manager of the MDCS and MPP cohorts. In Norway, we thank the screening team of the former National Health Screening Service of Norway, now the Norwegian Institute of Public Health. In the VHM&PP, we thank Elmar Stimpfl and Karin Parschalk for excellent technical support as well as Markus Wallner, Christian Bernhard and Gabriela Dür from the Vorarlberg State Government. Finally, we also thank the NPCR steering group: PS (chairman), Ingela Franck Lissbrant (co-chair), Camilla Thellenberg, Johan Styrke, Hampus Nugin, Stefan Carlsson, David Robinson, Mats Andén, Jon Kindblom, Olof Ståhl, Tomas Jiborn, Maria Nyberg, and Fredrik Sandin.
Funding
Funding for IIG_FULL_2020_025 was obtained from Wereld Kanker Onderzoek Fonds (WKOF), as part of the World Cancer Research Fund International grant programme. Furthermore, this work was supported by the Swedish Cancer Society (20 1033 PjF and CAN 2017/1019), the Swedish Research Council (2018-02825), the Swedish Prostate Cancer Federation, the Crafoord Foundation (20200546) and the Märta Winkler Foundation. Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
JF, conceptualisation, formal analysis, investigation, and writing–original draft; SHJJ, conceptualisation, data curation, investigation, and writing–review and editing; TB, data curation, investigation, and writing–review and editing; AMW, formal analysis, investigation, and writing–review and editing; CH, data curation, investigation, and writing–review and editing; HU, data curation, investigation, and writing–review and editing; GN, data curation, investigation, and writing–review and editing; EZ, investigation, and writing–review and editing; AE, investigation, and writing–review and editing; SH, investigation, and writing–review and editing; ID, investigation, and writing–review and editing; PS, investigation, and writing–review and editing; TS, conceptualisation, data curation, funding acquisition, investigation, and writing–original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The study was approved by research ethics committees in the respective countries (Norway: Regional Committee for Medical and Health Research Ethics, no 2012/2271/REC South-East, Sweden: EPN Umeå, no 2012-354-31M and no 2015-7-32M, and EPN Lund, no 2016/564 and 2020-01571, Austria: Ethics Committee of the province of Vorarlberg, no 2006-6/2). Individual informed consent for this analysis was waived since we only used de-identified data routinely collected during the health screening process.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fritz, J., Jochems, S.H.J., Bjørge, T. et al. Body mass index, triglyceride-glucose index, and prostate cancer death: a mediation analysis in eight European cohorts. Br J Cancer 130, 308–316 (2024). https://doi.org/10.1038/s41416-023-02526-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02526-1