Abstract
In the UK, the National Institute for Health and Care Excellence (NICE) recommends that women at moderate or high risk of breast cancer be offered risk-reducing medication and enhanced breast screening/surveillance. In June 2022, NICE withdrew a statement recommending assessment of risk in primary care only when women present with concerns. This shift to the proactive assessment of risk substantially changes the role of primary care, in effect paving the way for a primary care-based screening programme to identify those at moderate or high risk of breast cancer. In this article, we review the literature surrounding proactive breast cancer risk assessment within primary care against the consolidated framework for screening. We find that risk assessment for women under 50 years currently satisfies many of the standard principles for screening. Most notably, there are large numbers of women at moderate or high risk currently unidentified, risk models exist that can identify those women with reasonable accuracy, and management options offer the opportunity to reduce breast cancer incidence and mortality in that group. However, there remain a number of uncertainties and research gaps, particularly around the programme/system requirements, that need to be addressed before these benefits can be realised.
Similar content being viewed by others
Background
Breast cancer is the most common cancer worldwide and accounts for ~25% of cancers and 15% of cancer deaths in women [1]. Population-based screening programmes inviting women from age 50 for mammographic screening have been shown to reduce breast cancer mortality [2].
In the UK, the National Institute for Health and Care Excellence (NICE) recommends that women at moderate or high risk of breast cancer (Table 1) be offered additional breast screening/surveillance from younger ages and risk-reducing medication. It is estimated that more than 250,000 UK women are at moderate or high risk and so eligible for such interventions [3].
Women with high-risk pathogenic genetic variants (e.g., in BRCA 1/2) are identified through cascade testing led through specialist genetics clinics. How women at moderate or high risk but without known high-risk genetic variants within their family are best identified is less clear. Considerable work has been done [4, 5], and is ongoing [6], around the inclusion of breast cancer risk assessment to identify these women at the time of mammographic screening. However, this will miss younger women eligible for screening and preventative options. Primary care provides a potential route through which to identify these women.
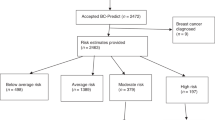
In the initial version of the current guidance [3], published in November 2019, NICE recommended that the role of primary care was limited to identifying women at moderate or high risk when they present with concerns. Research has shown that this opportunistic approach leads to only a small fraction of those at moderate or high risk being identified: in one survey among screening attendees it was estimated that 8.8% of women in their forties would be eligible for additional screening/surveillance and risk-reducing medication [7], but only 17.5% of that group had been seen in family history or clinical genetics services. Relying on women to self-present with concerns may also exacerbate existing health inequalities or disadvantage groups who have lower levels of health literacy.
In June 2022, following a stakeholder consultation, the NICE statement recommending identification of women only when they present with concerns was withdrawn to allow the proactive identification of women at increased risk of breast cancer within primary care. This shift to proactive identification substantially changes the role of primary care, in effect paving the way for a primary care-based screening programme to identify those at moderate or high risk of breast cancer. Any such programme will require establishing processes for identifying women at increased risk, pathways for offering them appropriate information and management, and robust assessments of likely benefits and costs.
In this article, we review the current literature surrounding the proactive identification of women at increased risk of breast cancer within primary care. We use the principles of the consolidated framework for screening [8] to establish whether the process meets the conditions for a screening programme and to identify key challenges, uncertainties and research gaps. Our focus is on the UK given the recent change in NICE guidance but the principles apply to the introduction of similar programmes internationally.
Disease/condition principles
Epidemiology of the disease/condition
Increasing age is the most common risk factor for breast cancer with incidence rates rising sharply until menopause and more slowly thereafter [9]. Other known risk factors that can be used to identify women at elevated risk include: family history of breast cancer [10], lifestyle and anthropometric factors such as alcohol consumption [11], height [12] and body mass index [13], hormone-related risk factors such as ages at menarche and menopause [14], oral contraceptive use [15] and menopausal hormone replacement therapy use [16], reproductive factors such as parity and age at first live birth [17] and breast density [18]. In addition, genetic susceptibility to breast cancer is conferred by rare pathogenic variants in high- and moderate-risk genes (including BRCA1, BRCA2, PALB2, CHEK2, ATM, BARD1, RAD51C and RAD51D) [19] and common low-penetrance alleles which combine multiplicatively and can be represented as polygenic scores (PGS) [20].
Based on distributions of known risk factors in the UK, it is estimated that approximately 17% of women are at above population-level risk and 48% of cases of breast cancers occur in that group [21]. Studies at breast cancer screening have similarly identified around 18.5% of women over age 50 at moderate or high risk [22]. In the only study in primary care, 11% of women were at above population-level risk [23]. That study had a response rate of only 16.1% though and risk was assessed using family history alone. The risk distribution based on multifactorial risk assessment in a population identified through primary care is, therefore, unknown.
Natural history of the disease/condition
In recent years the biology of breast cancer has become better understood, including increasing knowledge of the histological and molecular characteristics and drivers for cell proliferation [24]. There is also clear evidence of benefits and opportunities for early detection, with the typical breast cancer tumour volume doubling time estimated to be 150 days [25] and 5-year survival 97.9% at Stage I and falling to 26.2% at Stage IV [26]. The relationship between the natural history of the disease and breast cancer risk is less well understood. It is known that variants in several of the high-risk genes are more strongly associated with oestrogen receptor (ER)-negative or triple-negative breast cancer, while polygenic scores are more strongly associated with ER-positive disease [20, 27]. Several lifestyle factors also show differential risks by subtype, pointing to differences in the natural history and hence potentially screening efficacy. Studies are ongoing among those women attending mammographic screening that will hopefully inform this [28].
Target population
As described above, there is considerable work being conducted to evaluate the potential for offering risk assessment alongside mammography to identify women attending screening who are above near-population risk [4,5,6]. The principal target population for proactive identification in primary care is, therefore, those women who would potentially benefit from interventions but are not yet eligible to be invited for population-based screening. In the UK, this is women under 50.
Identifying this target group is straightforward using electronic healthcare records. A much greater challenge is being able to reach these women. A number of potential strategies exist. These include postal or text message invitations and invitations at the time of other healthcare delivery. All of these approaches have the potential to exacerbate existing health inequalities through low engagement. For example, in the context of breast cancer screening, uptake of risk assessment questionnaires at the time of mammography was significantly lower in areas with higher deprivation [22]; and in the only study to date to proactively seek to identify high-risk women within UK primary care, only 16.1% of women (n = 1127/7012) returned family history questionnaires [23], with those from minority ethnic communities and those with low literacy underrepresented. More active strategies for engagement, including tailored approaches with underrepresented populations, will therefore be needed [29]. These might include working with patient navigators or community health champions alongside text message primers, computer prompts, behaviourally informed messaging and targeted telephone outreach that have been associated with greater uptake of NHS Health Checks within primary care [30].
Test/intervention principles
Screening test performance characteristics
In the context of breast cancer risk assessment, the test is the estimation of an individual’s risk of breast cancer. Several risk prediction models exist. Table 2 summarises the risk factors included in some of the most recently developed and widely used models [21, 31,32,33,34,35].
It is important that risk prediction models are well calibrated (i.e., the predicted risks agree with the observed risks within different risk categories), and that they have good discriminatory ability for distinguishing between those who will develop the disease and unaffected women in the target population. Studies assessing the performance of these models have consistently shown that model performance is maximised when the joint effects of risk factors are considered in multifactorial breast cancer risk prediction [21, 36, 37]. Population-based studies of multifactorial risk models that include polygenic scores in pre-menopausal women or those under the age of 50 have shown that the BOADICEA and Tyrer–Cuzick models have moderate-to-good discrimination with AUCs or c-indices of 0.68–0.69 [38, 39] and the iCARE model an AUC of 0.64. BOADICEA and iCARE are also well calibrated with a ratio of expected to observe the number of cases (E/O) of 0.97 [39] and 0.9 [36], respectively, while the Tyrer–Cuzick model shows evidence of overestimating risk amongst those in the highest-risk decile (E/O: 1.54) [39].
The benefits of multifactorial risk assessment are particularly seen when considering the effects on risk classification. For example, a population aged 40 with unknown family history would without risk assessment be considered at near-population risk. Using the full set of risk factors within the BOADICEA model, 86.4% of women in the population would be classified at near-population risk of developing breast cancer and 13.6% at moderate or high risk. Using questionnaire-based risk factors alone would classify only 1.8% of those women at moderate risk and none as high risk [21]. The absolute numbers, however, differ between risk models [40]. A further major limitation at present of these risk models, particularly those incorporating PGS, is that to date they have all been developed using data primarily from individuals of European ancestry. As a result, they perform less well in other ancestral groups [41] and have the potential to increase inequalities in care. Further research to develop or adapt risk models for use within other ancestral groups is needed before breast cancer risk assessment can be offered to the population at large.
Whichever risk prediction model is chosen, obtaining accurate estimates requires accurate data on relevant risk factors. Many of the risk factors included in multifactorial risk models, particularly those relating to genetic/familial risk and reproductive factors, are not routinely available within primary care. With the exception of the QCancer10 model, all the risk models in Table 2 require additional data collection. Mechanisms to collect this additional data are, therefore, needed. Several tools have been designed to support this [42,43,44,45,46]. Each varies in the time they take to complete due to variations in the complexity of the family history required and different user interfaces. Models including genetic risk factors also require biological samples. Currently, almost all germline cancer genetic testing in the NHS is done using blood samples. However, saliva is an equally good alternative for most testing and has the advantage of allowing the sample to be taken at home, making it more acceptable for women [47], and is more straightforward to transport. Incorporating breast density is more challenging in this age group as most women will not have had breast imaging. Research is ongoing to define the magnitude of breast cancer risk associated with mammographic density in young women and the acceptability of low-dose mammography for risk assessment in this group [48]. However, this introduces significant additional challenges in terms of clinical workflow and the service model.
Interpretation of screening test results
There are existing well-defined, evidence-based and agreed risk thresholds that are set by NICE (Table 1) [3]. The categorisation of women following risk assessment is, therefore, straightforward. The challenge is communicating the results of the risk assessment and how these risks relate to recommended management options in such a way that they are clearly interpretable and support informed decision-making. As highlighted in a recent review [49], this is not straightforward as risk is a multidimensional concept, with lay perceptions often being resistant to change, dominated by family history and appraised differently from how healthcare professionals communicate risk. Developing ways to explain breast cancer risk information in a way that is intelligible to the general population is therefore important. Tailored communication strategies may be needed for those with low literacy. Ideally, these would be based on evidence-based approaches to communicating risk [50] and tested in the specific context of breast cancer risk assessment in primary care.
Post-screening test options
The post-screening management options are already well-defined by NICE guidelines [3]. All women, independent of risk, should receive lifestyle advice, with all those at moderate or high risk of breast cancer offered risk-reducing medication and enhanced breast cancer screening/surveillance dependent on age and risk level (Table 3). Women at very high risk due to known genetic variants are also eligible for risk-reducing surgery. Currently, most very high-risk women will be identified through cascade testing within secondary care, meaning that risk-reducing medication and enhanced screening/surveillance are the two main management options for women identified through primary care.
The evidence for enhanced screening/surveillance among these women largely comes from population-based trials offering women aged 40–49 earlier mammography. From these trials, it is estimated that annual mammography would reduce mortality from breast cancer by 12–29%, with a 0.1% risk of over-diagnosis, a false-positive recall every 10 years and fatal radiation-induced breast cancer on average once every 76,000–97,000 years [51]. There is also low-quality evidence to suggest that mammographic screening specifically in women aged 50 years or less with a family history of breast cancer reduces mortality and that invasive breast cancers diagnosed in the screened group are significantly smaller than those diagnosed in unscreened women of similar age and less likely to have spread to lymph nodes [52, 53].
There is high-quality evidence that tamoxifen reduces breast cancer incidence in pre-menopausal women who do not have a diagnosis of breast cancer [54, 55]. Based on NICE eligibility and assuming a 25% uptake, over 50 years it is estimated that 11 cases of breast cancer could be avoided per 1000 women who are offered risk-reducing medication [3]. Tamoxifen has been associated with a small increase in the risk of endometrial cancer (RR 2.13; 95% CI, 1.36–3.32) and venous thromboembolisms (RR 1.93; 95% CI, 1.41–2.64) [55]. However, the risk of venous thromboembolisms is largely confined to the active treatment period [54] and, where sub-group analyses have been performed, significant increases in the risk of endometrial cancer have not been seen in women under 50 [56].
Programme/system principles
Screening programme infrastructure
As with the introduction of any new service within primary care, the introduction of a proactive breast cancer risk assessment would require additional funding to account for the additional time for the work undertaken by primary care [57,58,59,60,61]. This is particularly important given the recent increasing demands on primary care. In the UK, potential routes for such funding include the Quality and Outcomes Framework, Directed Enhanced Services and central models of payment as used for the NHS Health Check Programme.
There is also a need for risk assessment tools that are integrated within the electronic health records to enable collection, recording and sharing of risk information between patients, professionals and care settings [45, 61,62,63] and streamlining of the collection of risk factor information through the use of patient-facing tools. Of the available breast cancer risk assessment tools, only the QCancer10 model [35] is currently available as a software development kit to build it within electronic health records but this does not incorporate many of the well-established breast cancer risk factors. Other risk prediction models rely on external web-based applications that require primary care professionals to enter data manually, substantially adding to the time required for conducting risk assessments. Primary care is leading the way in terms of implementing interoperable electronic health records within the UK and this has been further expedited by the COVID-19 pandemic. However, the challenges of integrating new risk assessment tools into the NHS [64], and primary care specifically [65], are likely to remain and are made more complex by how, currently, IT digital services are commissioned, adopted and maintained through individual local Integrated Care Systems rather than nationally.
Alongside these digital tools, additional training for primary care healthcare professionals will be required if discussions around multifactorial risk are to take place in primary care. Previous studies have consistently identified primary care providers’ lack of knowledge about breast cancer risk assessment, particularly genetic testing, and lack of confidence and access to referral guidance as significant barriers to engagement [45, 61, 63, 66,67,68,69]. Initiatives to provide such training are ongoing and include resources across relevant NHS and professional colleges websites [70, 71]. Evaluation of these training resources is needed.
More generally, there will also need to be updates to the current referral pathways for those at moderate or high risk of breast cancer, and sufficient capacity and funding within the wider healthcare system to provide additional screening/surveillance and consultations to discuss risk-reducing medication for those women identified as being at moderate or high risk. Providing this additional screening/surveillance will likely require the commissioning of new services: a survey of all cancer genetics leads covering 22 regional centres in the UK in 2019 showed that 15 years after the original NICE guidance was published, 10.4 million women (16.4% of the total population) were still living in regions not supplying appropriate moderate-risk surveillance and up to 42% of the population were living in areas not covered by the recommended high-risk surveillance [72]. There will also need to be sufficient laboratory capacity to process saliva or blood samples for polygenic risk score assessment and gene panel testing. As the NHS Genomic Medicine Service covers the whole range of genetic tests (not only cancer), any change would need to be modelled to assess the potential impact on other services.
Screening programme co-ordination and integration
One of the biggest challenges raised by healthcare professionals in a focus group study of incorporating cancer risk within primary care was finding the best time and place for risk assessment [61]. Several studies in the US have shown that risk assessment is feasible in primary care waiting rooms prior to annual health check or new patient visits [73,74,75,76]. However, until genetic testing is widespread within mainstream healthcare settings, this does not allow for genetic testing to be incorporated in the risk assessment prior to discussion with the primary care professional. In a recent interview study exploring the barriers and facilitators to implementing CanRisk in UK general practice, GPs and practice nurses cited appointments around the prescription/review of contraception and hormone replacement therapy as being potentially the most appropriate opportunities, due to standard discussion around the impact of these medications on breast cancer risk [paper in preparation: SA, FSD, Carver, Yue, Cunningham, Ficorella, MT, DFE, ACA, JE, JUS, FMW. Exploring the barriers and facilitators of implementing CanRisk in primary care: a qualitative thematic framework analysis]. Some suggested that a risk assessment could also be conducted or mentioned during cervical cancer screening appointments, but there were concerns about adding additional stress and/or anxiety to these already challenging healthcare appointments. There is also evidence that women prefer information by email or online rather than during GP consultations [47]. Research evaluating different implementation strategies and the impact on primary care and uptake is needed.
It is also unclear how frequently breast cancer risk assessment should be repeated. The current NICE guidance suggests reassessment if a woman’s family history changes [3]. However, with the inclusion of modifiable lifestyle and hormonal factors in a risk assessment, changes in these risk factors, or the development of more predictive PGS over time, could potentially result in reclassification of woman’s risk category. How any such changes in risk would be handled also needs to be considered, particularly for women moving from a higher-risk category to a lower-risk category.
Screening programme acceptability and ethics
A recent systematic review showed that primary care providers are likely to accept an increased role in breast cancer risk assessment as they already collect family history information regularly and readily perceive it as their responsibility [63]. However, if the risk assessment were to be conducted within a consultation there are concerns about how that may change the dynamic of the consultation [45] and about the depth and intrusive nature of some of the questions required for risk assessment, particularly around pregnancy and baby loss. Other concerns include the ethical justification of discussing breast cancer risk if little can be done by the woman to reduce her risk [57, 77], as well as concerns about the accuracy of risk estimates derived from models, particularly when information about risk factors is incomplete [45, 76]. The provision of training targeted at increasing knowledge about risk management strategies and risk calculation would address these concerns.
Healthcare professionals have also identified a number of ethical implications that would need to be considered in any future programme [66]. These include potential issues around autonomy, distributive justice, privacy, stigma, storage and access to genetic material and information, discrimination from employers and healthcare systems or insurers and the potential to increase inequalities as a result of the differential performance of polygenic risk scores in non-European ancestries described above.
Breast cancer risk assessment itself has been shown to be widely acceptable to the public [78,79,80,81,82,83,84,85]. Women are optimistic about receiving individualised breast cancer risk estimates, with studies reporting that 85% women consider risk assessment to be a good idea [86] and most are comfortable providing the information for the risk assessment, whether personal information, a blood sample, or a mammogram [79, 80]. Importantly, no women found to be high risk in one study regretted finding out their risk [87] and all appear to understand the principles/purpose of risk stratification [84]. The acceptability of the risk assessment taking place within primary care is limited to two studies in the US [75, 88]. These studies suggest that risk assessment, without genetic risk factors, is both acceptable and feasible to the public in the primary care context. The potential acceptability of incorporating polygenic risk scores has been demonstrated in a recent study reporting 84% uptake of a primary care-based polygenic risk assessment for colorectal cancer [89]. Additionally, evidence suggests that a risk assessment endorsed and performed by a familiar individual or institution, such as general practice, may be more acceptable to women and that uptake may be improved by easier access [83].
As the main benefit from risk assessment arises through those women who are identified as being at moderate or high risk being offered, and subsequently taking up, earlier screening/surveillance and/or risk-reducing medication, the acceptability of these management options is key. Numerous studies have demonstrated widespread reticence by primary care practitioners to discuss and prescribe risk-reducing medication for women at high risk of breast cancer [63, 90,91,92]. Lack of familiarity with and knowledge of preventive therapy has been identified as a contributing factor [91]. In addition, primary care providers do not perceive the initiation of risk-reducing medication as their responsibility [90]. However, general practitioners have reported greater willingness to continue a prescription if it has been started in secondary care [92]. This suggests that primary care would be more accepting of involvement in prescribing risk-reducing medication if shared-care agreements were in place.
The acceptability of risk-reducing medication amongst women is also generally low, with uptake outside trial settings only 8.7% [93]. A number of factors have been shown to contribute to poor uptake and compliance, including knowledge of the harms and benefits, and side effects [94,95,96,97]. Decisions are also influenced by age, socioeconomic status, race and ethnicity, family history, education, numeracy, psychological well-being, risk level, communication format and trust in healthcare professionals [98,99,100]. Access to tailored patient education materials to support informed decisions will, therefore, be needed [63].
In contrast, the offer of enhanced screening/surveillance appears to be generally acceptable to women, with one study amongst women attending familial cancer clinics reporting that 77% of women aged 30–39 and 96% aged 40–49 were vigilant with respect to mammography recommendations [101]. There are, however, persistent inequalities in access, and uptake of enhanced screening/surveillance policies for women from ethnic minorities and deprived areas who are at moderate and high risk of developing breast cancer is lower [72, 102]. There is little research exploring reasons for this and no studies recruiting women from primary care.
Screening programme benefits and harms
The main rationale for breast cancer risk assessment is the offer of enhanced screening/surveillance and/or risk-reducing medications for women who are at increased risk but currently unaware of this. As described above, increased screening/surveillance or uptake of cancer-preventing drugs in this group would be expected to lead to reductions in cancer incidence, cancer-related morbidity and mortality. No studies, however, have been conducted in primary care to assess the impact of risk assessment on these “downstream” benefits [103] or the potential harms of over-diagnosis and overtreatment. To detect such effects would require a very large trial or observational study, in line with the generally small effects that population-based cancer screening has on these outcomes [2].
In addition to these “downstream” benefits, the risk assessment process itself potentially also has more “upstream” benefits and harms. These include the impact on future uptake of national screening, change in health-related behaviours and psychological outcomes. Quantifying these more “upstream” effects is important as any potential reduction in cancer incidence for a small proportion of the population needs to be balanced against the potential for possible net harms among the majority who will be at near-population risk, particularly if uptake of risk-reducing interventions is low amongst those at moderate or high risk.
No studies have been conducted in primary care to assess the impact of breast cancer risk assessment on these more “upstream” effects. The best available evidence comes from national screening programmes. In this setting, women in receipt of risk estimates are no less likely to attend future rounds of screening [104], while women who are told they are at high risk are considerably more likely to attend future rounds of screening [105]. This is in line with the intended purpose of identifying women at higher risk, and provides direct evidence that these intended benefits are likely to be accrued. There is also some evidence that women in receipt of estimates of higher breast cancer risk are more willing to take up, and persist with, interventions to promote healthier behaviours [106]. However, there is now good direct evidence that the provision of breast cancer risk estimates does not have a major impact on health-related behaviours such as increased physical activity or healthier eating at a population level [107]. These findings are in line with systematic reviews of the wider literature, which suggest limited population-level effects of personalised risk information [108] or personalised information derived from genetic sources [109].
With respect to psychological outcomes, although there are no data from primary care or in the age group targeted for proactive risk assessment in primary care, there are now considerable data on the effects of providing estimates of breast cancer risk to women aged 47–73 recruited via the NHS Breast Screening Programme. These data indicate that women who were told they were at higher risk were more worried about cancer, but there was no evidence of an overall effect on worry or adverse effects on anxiety [107]. Similarly, there was no evidence of low-risk estimates producing false reassurance [107], in line with systematic review evidence that concerns about false reassurance following screening test results is unfounded [110]. There is a need to show no such adverse effects when setting up a new programme with younger women. The impact of being identified as at higher risk has potentially greater implications for younger women when considering, for example, plans for a family. It is also important to note that there is a complete absence of evidence on the impact of providing risk estimates on some other outcomes, such as informed decision-making [111]. This is especially important as promoting informed decision-making surrounding screening decisions is an explicit aim of most screening programmes.
Economic evaluation of the screening programme
A number of analyses have assessed the cost-effectiveness of earlier mammography breast cancer screening in high-risk groups. These have shown that biennial screening from age 40 onwards in women at increased risk of breast cancer is cost-effective [112] and results in a similar ratio of false-positive findings and life-years gained as biennial screening in average-risk women between age 50 and 74 [113], and having a lower starting age for women at higher risk would increase screening benefit and reduce over-diagnosis, but at a relatively higher increase in false-positive findings [114, 115].
No full cost-effectiveness analysis has been conducted on risk-reducing medication in pre-menopausal women. A cost-consequences analysis performed by the NICE guideline development panel estimated that offering risk-reducing medication in accordance with the recommendations would be cost-effective at a threshold of £20,000 per QALY if there was a gain of at least 1.71 QALYs per 1000 eligible women. In women over 50, it is estimated that 11 cases of breast cancer could be avoided per 1000 women who are offered risk-reducing medication and so the panel were confident that the costs of preventing a case of breast cancer were likely to be considered acceptable from an NHS perspective. The costs in women under 50 are not known.
To our knowledge, no economic evaluation has been conducted of proactively offering breast cancer risk assessment within primary care.
Screening programme quality and performance management
If proactive risk assessment for breast cancer risk were to be implemented on a large scale there would need to be a clear specification and set of quality assurance standards and resources for delivering and monitoring the programme. This would include protocols for who should be tested, requirements for specimens and laboratory analysis of relevant risk assessment parameters (e.g., polygenic risk scores), and clinical follow-up of those identified as moderate or high risk, as well as expected internal quality control and performance criteria and published laboratory and clinical guidelines and standards. Quality assurance will also be needed with respect to the data used in risk assessment. This includes clinical accreditation of any discrete tests such as genotyping to obtain a polygenic score, and any risk tools or models used for this purpose.
Developing such a programme would also require dialogue with policymakers to determine what parameters are important to monitor for quality assurance and who would be responsible for the programme oversight. Given the existence of mechanisms for monitoring existing breast cancer screening programmes, these can be used as a starting point to achieve alignment with any existing standards and guidance.
Conclusion
Proactive breast cancer risk assessment within primary care for women under 50 years currently satisfies many of the key principles of screening. Most notably, there are large numbers of women at moderate or high risk currently unidentified, there are risk models available that are able to identify those women with reasonable accuracy, and management options exist that offer the opportunity to reduce breast cancer incidence, morbidity and mortality in that group. However, there remain a number of uncertainties and research gaps that need to be addressed before these benefits can be realised (Table 4). These include the evaluation of different implementation strategies, including how to best reach women without exacerbating health inequalities, research to develop or adapt risk models for non-European groups and to develop and evaluate evidence-based approaches to communicating risk and the benefits and harms of management options to women, trials to assess the outcomes of risk assessment among women identified through primary care, and economic evaluations.
Data availability
Not applicable.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M. The benefits and harms of breast cancer screening: an independent review. Br J Cancer. 2013;108:2205–40.
National Institute for Health and Care Excellence. Familial breast cancer: classification, care and managing breast cancer and related risks in people with a family history of breast cancer. CG164. 2017. https://www.nice.org.uk/guidance/cg164.
Gray E, Donten A, Karssemeijer N, van Gils C, Evans DG, Astley S, et al. Evaluation of a stratified national breast screening program in the united kingdom: an early model-based cost-effectiveness analysis. Value Heal. 2017;20:1100–9.
Evans DGR, Donnelly LS, Harkness EF, Astley SM, Stavrinos P, Dawe S, et al. Breast cancer risk feedback to women in the UK NHS breast screening population. Br J Cancer. 2016;114:1045–52.
French DP, Astley S, Astley S, Brentnall AR, Cuzick J, Dobrashian R, et al. What are the benefits and harms of risk stratified screening as part of the NHS breast screening Programme? Study protocol for a multi-site non-randomised comparison of BC-predict versus usual screening (NCT04359420). BMC Cancer. 2020;20:1–14.
Evans DG, Brentnall AR, Harvie M, Dawe S, Sergeant JC, Stavrinos P, et al. Breast cancer risk in young women in the national breast screening programme: Implications for applying NICE guidelines for additional screening and chemoprevention. Cancer Prev Res. 2014;7:993–1001.
Dobrow MJ, Hagens V, Chafe R, Sullivan T, Rabeneck L. Consolidated principles for screening based on a systematic review and consensus process. Can Med Assoc J. 2018;190:E422–E429.
Cancer Research UK. Breast cancer incidence statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer/incidence-invasive. Accessed 27 Aug 2022.
Beral V, Bull D, Doll R, Peto R, Reeves G, Skegg D, et al. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet. 2001;358:1389–99.
Hamajima N, Hirose K, Tajima K, Rohan T, Calle EE, Heath CW, et al. Alcohol, tobacco and breast cancer-collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer. 2002;87:1234–45.
Green J, Cairns BJ, Casabonne D, Wright FL, Reeves G, Beral V. Height and cancer incidence in the Million Women Study: prospective cohort, and meta-analysis of prospective studies of height and total cancer risk. Lancet Oncol. 2011;12:785–94.
Nelson HD, Zakher B, Cantor A, Fu R, Griffin J, O’Meara ES, et al. Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis. Ann Intern Med. 2012;156:635–48.
Hamajima N, Hirose K, Tajima K, Rohan T, Friedenreich CM, Calle EE, et al. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13:1141–51.
Hunter DJ, Colditz GA, Hankinson SE, Malspeis S, Spiegelman D, Chen W, et al. Oral contraceptive use and breast cancer: a prospective study of young women. Cancer Epidemiol Biomark Prev. 2010;19:2496–502.
Beral V, Reeves G, Bull D, Green J. Breast cancer risk in relation to the interval between menopause and starting hormone therapy. J Natl Cancer Inst. 2011;103:296–305.
Reeves GK, Pirie K, Green J, Bull D, Beral V. Comparison of the effects of genetic and environmental risk factors on in situ and invasive ductal breast cancer. Int J Cancer. 2012;131:930–7.
McCormack VA, Dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev. 2006;15:1159–69.
Dorling L, Carvalho S, Allen J, González-Neira A, Luccarini C, Wahlström C, et al. Breast cancer risk genes— association analysis in more than 113,000 women. N Engl J Med. 2021;384:428–39.
Mavaddat N, Michailidou K, Dennis J, Lush M, Fachal L, Lee A, et al. Polygenic risk scores for prediction of breast cancer and breast cancer subtypes. Am J Hum Genet. 2019;104:21–34.
Lee A, Mavaddat N, Wilcox AN, Cunningham AP, Carver T, Hartley S, et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21:1708–18.
Evans DGR, Warwick J, Astley SM, Stavrinos P, Sahin S, Ingham S, et al. Assessing individual breast cancer risk within the U.K. National Health Service Breast Screening Program: a new paradigm for cancer prevention. Cancer Prev Res. 2012;5:943–51.
Qureshi N, Dutton B, Weng S, Sheehan C, Chorley W, Robertson JFR, et al. Improving primary care identification of familial breast cancer risk using proactive invitation and decision support. Fam Cancer. 2021;20:13–21.
Harbeck N, Penault-Llorca F, Cortes J, Gnant M, Houssami N, Poortmans P, et al. Breast Cancer. 2019; https://doi.org/10.1038/s41572-019-0111-2.
Pashayan BN, Pharoah PDP. The challenge of early detection in cancer. Science. 2020;368:589–90.
Cancer Research UK. Breast cancer survival statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer/survival. Accessed 27 Aug 2022.
Mavaddat N, Dorling L, Carvalho S, Allen J, González-Neira A, Keeman R, et al. Pathology of tumors associated with pathogenic germline variants in 9 breast cancer susceptibility genes. JAMA Oncol. 2022;8:1–11.
University of Cambridge Centre for Cancer Genetic Epidemiology. SEARCH study. 2022.https://ccge.medschl.cam.ac.uk/search-study/risk-stratified-screening-for-breast-cancer/. Accessed 2 Sep 2022.
Sasieni P. Equality and equity in medical screening: what is fair? Lancet Gastroenterol Hepatol. 2019;4:4–6.
Public Health England. Top tips for increasing uptake of NHS Health Checks. https://www.gov.uk/government/publications/nhs-health-checks-increasing-uptake/top-tips-for-increasing-the-uptake-of-nhs-health-checks. Accessed 2 Aug 2022.
Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111–30.
Choudhury PP, Maas P, Wilcox A, Wheeler W, Brook M, Check D, et al. iCARE: an R package to build, validate and apply absolute risk models. PLoS ONE. 2020;15:e0228198 https://doi.org/10.1371/JOURNAL.PONE.0228198.
Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K. Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Ann Intern Med. 2008;148:337–47.
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–86.
Hippisley-Cox J, Coupland C. Development and validation of risk prediction algorithms to estimate future risk of common cancers in men and women: prospective cohort study. BMJ Open. 2015;5:e007825.
Hurson AN, Pal Choudhury P, Gao C, Hüsing A, Eriksson M, Shi M, et al. Prospective evaluation of a breast-cancer risk model integrating classical risk factors and polygenic risk in 15 cohorts from six countries. Int J Epidemiol. 2021;50:1897–911.
Ho PJ, Ho WK, Khng AJ, Yeoh YS, Tan BKT, Tan EY, et al. Overlap of high-risk individuals predicted by family history, and genetic and non-genetic breast cancer risk prediction models: implications for risk stratification. BMC Med. 2022;20:1–11.
Yang X, Eriksson M, Czene K, Lee A, Leslie G, Luch M, et al. Prospective validation of the BOADICEA multifactorial breast cancer risk prediction model in a large prospective study. J Med Genet. 2022;59:1196–205.
Pal Choudhury P, Brook MN, Hurson AN, Lee A, Mulder CV, Coulson P, et al. Comparative validation of the BOADICEA and Tyrer-Cuzick breast cancer risk models incorporating classical risk factors and polygenic risk in a population-based prospective cohort of women of European ancestry. Breast Cancer Res. 2021;23:1–5.
Schonberg MA, Karamourtopoulos M, Pinheiro A, Davis RB, Sternberg SB, Mehta TS, et al. Variation in breast cancer risk model estimates among women in their 40s seen in primary care. J women’s Heal. 2022;31:495–502.
Evans DG, van Veen EM, Byers H, Roberts E, Howell A, Howell SJ, et al. The importance of ethnicity: are breast cancer polygenic risk scores ready for women who are not of White European origin? Int J Cancer. 2021;150:73–79.
Collins IM, Bickerstaffe A, Ranaweera T, Maddumarachchi S, Keogh L, Emery J, et al. iPrevent®: a tailored, web-based, decision support tool for breast cancer risk assessment and management. Breast Cancer Res Treat. 2016;156:171–82.
Lo LL, Collins IM, Bressel M, Butow P, Emery J, Keogh L, et al. The iPrevent online breast cancer risk assessment and risk management tool: usability and acceptability testing. JMIR Form Res. 2018;2:1–11.
Ozanne EM, Howe R, Omer Z, Esserman LJ. Development of a personalized decision aid for breast cancer risk reduction and management. BMC Med Inf Decis Mak. 2014;14:4 https://doi.org/10.1186/1472-6947-14-4.
Archer S, De Villiers CB, Scheibl F, Carver T, Hartley S, Lee A, et al. Evaluating clinician acceptability of the prototype CanRisk tool for predicting risk of breast and ovarian cancer: a multi-methods study. PLoS ONE. 2020;15:1–19.
Carver T, Hartley S, Lee A, Cunningham AP, Archer S, de Villiers CB, et al. Canrisk tool—a web interface for the prediction of breast and ovarian cancer risk and the likelihood of carrying genetic pathogenic variants. Cancer Epidemiol Biomark Prev. 2021;30:469–73.
Wheeler JCW, Keogh L, Sierra MA, Devereux L, Jones K, IJzerman MJ, et al. Heterogeneity in how women value risk-stratified breast screening. Genet Med. 2022;24:146–56.
Howell SJ. Breast CANcer risk assessment in younger women: BCAN-RAY (BCAN-RAY). 2022. https://clinicaltrials.gov/ct2/show/NCT05305963. Accessed 5 Sep 2022.
Woof VG, Howell A, Mcwilliams L, Evans DG, French DP. How do women who are informed that they are at increased risk of breast cancer appraise their risk? A systematic review of qualitative research. Br J Cancer. 2022;127:1916–24.
Zipkin DA, Umscheid CA, Keating NL, Allen E, Aung K, Beyth R, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161:270–80.
Grimm LJ, Avery CS, Hendrick E, Baker JA. Benefits and risks of mammography screening in women ages 40 to 49 years. J Prim Care Community Heal. 2022;13:1–6.
Maurice A, Evans DGR, Shenton A, Ashcroft L, Baildam A, Barr L, et al. Screening younger women with a family history of breast cancer—does early detection improve outcome? Eur J Cancer. 2006;42:1385–90.
Duffy SW. Mammographic surveillance in women younger than 50 years who have a family history of breast cancer: tumour characteristics and projected effect on mortality in the prospective, single-arm, FH01 study. Lancet Oncol. 2010;11:1127–34.
Cuzick J, Sestak I, Bonanni B, Costantino JP, Cummings S, DeCensi A, et al. Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data. Lancet. 2013;381:1827–34.
Nelson HD, Fu R, Griffin JC, Nygren P, Smith B, Humphrey L. Systematic review: comparative effectiveness of medications to reduce risk for primary breast cancer. Ann Intern Med. 2009;151:703–15.
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 2005;97:1652–62.
Collins IM, Steel E, Mann GB, Emery JD, Bickerstaffe A, Trainer A, et al. Assessing and managing breast cancer risk: clinicians’ current practice and future needs. Breast. 2014;23:644–50.
Francis NA, Hood K, Simpson S, Wood F, Nuttall J, Butler CC. The effect of using an interactive booklet on childhood respiratory tract infections in consultations: study protocol for a cluster randomised controlled trial in primary care. BMC Fam Pract. 2008;9:23.
Fairfield KM, Emmons KM, Rigotti NA, Colditz GA. Use of a computerized risk-appraisal instrument for cancer prevention education of medical students. J Cancer Educ. 2002;17:183–5.
Fairfield KM, Chen WY, Colditz GA, Emmons KM, Fletcher SW. Colon cancer risk counseling by health-care providers: perceived barriers and response to an internet-based cancer risk appraisal instrument. J Cancer Educ. 2004;19:95–97.
Usher-smith JA, Silarova B, Ward A, Youell J, Muir KR. Incorporating cancer risk information into general practice: a qualitative study using focus groups with healthcare professionals. BJGP. 2017;67:e218–e226.
Dickfos M, King D, Parekh S, Boyle FM, Vandelanotte C. General practitioners’ perceptions of and involvement in health behaviour change: can computer-tailored interventions help? Prim Health Care Res Dev. 2015;16:316–21.
Bellhouse S, Hawkes RE, Howell SJ, Gorman L, French DP. Breast cancer risk assessment and primary prevention advice in primary care: a systematic review of provider attitudes and routine behaviours. Cancers. 2021;13:1–23.
Asthana S, Jones R, Sheaff R. Why does the NHS struggle to adopt eHealth innovations? A review of macro, meso and micro factors. BMC Health Serv Res. 2019;19:1–7.
Young AJ. New technologies and general practice. Br J Gen Pract. 2016;66:601–2.
Rainey L, van der Waal D, Jervaeus A, Wengström Y, Evans DG, Donnelly LS, et al. Are we ready for the challenge of implementing risk-based breast cancer screening and primary prevention? Breast. 2018;39:24–32.
Nippert I, Julian-Reynier C, Harris H, Evans G, Van Asperen CJ, Tibben A, et al. Cancer risk communication, predictive testing and management in France, Germany, the Netherlands and the UK: general practitioners’ and breast surgeons’ current practice and preferred practice responsibilities. J Community Genet. 2014;5:69–79.
Suther S, Goodson P. Barriers to the provision of genetic services by primary care physicians: a systematic review of the literature. Genet Med. 2003;5:70–6.
Smit AK, Sharman AR, Espinoza D, Wallingford C, Young MA, Dunlop K, et al. Knowledge, views and expectations for cancer polygenic risk testing in clinical practice: a cross-sectional survey of health professionals. Clin Genet. 2021;100:430–9.
Health Education England. GeNotes: genomics notes for clinicatians. 2022. https://www.genomicseducation.hee.nhs.uk/about-us/genotes-genomic-notes-for-clinicians/. Accessed 27 Aug 2022.
QGenome. https://qgenome.co.uk/. Accessed 20 Sep 2022.
Evans DG, Edwards M, Duffy SW, Adlard J, Ahmed M, Barwell J, et al. Sporadic implementation of UK familial mammographic surveillance guidelines 15 years after original publication. Br J Cancer. 2020;122:329–32.
Kaplan CP, Livaudais-Toman J, Tice JA, Kerlikowske K, Gregorich SE, Perez-Stable EJ, et al. A randomized, controlled trial to increase discussion of breast cancer in primary care. Cancer Epidemiol Biomark Prev. 2014;23:1245–53.
Hoskins KF, Tejeda S, Vijayasiri G, Chukwudozie IB, Remo M, Shah H, et al. A feasibility study of breast cancer genetic risk assessment in a federally qualified health center. Cancer. 2018;124:3733–41.
Anderson EE, Tejeda S, Childers K, Stolley MR, Warnecke RB, Hoskins KF. Breast cancer risk assessment among low-income women of color in primary care: a pilot study. J Oncol Pract. 2015;11:e460–e467.
Owens WL, Gallagher TJ, Kincheloe MJ, Ruetten VL. Implementation in a large health system of a program to identify women at high risk for breast cancer. J Oncol Pract. 2011;7:85–88.
Phillips KA, Steel EJ, Collins I, Emery J, Pirotta M, Mann GB, et al. Transitioning to routine breast cancer risk assessment and management in primary care: what can we learn from cardiovascular disease? Aust J Prim Health. 2016;22:255–61.
Ghanouni A, Waller J, Stoffel ST, Vlaev I, von Wagner C. Acceptability of risk-stratified breast screening: effect of the order of presenting risk and benefit information. J Med Screen. 2020;27:52–56.
Mbuya-Bienge C, Pashayan N, Brooks JD, Dorval M, Chiquette J, Eloy L, et al. Women’s views on multifactorial breast cancer risk assessment and risk-stratified screening: a population-based survey from four Provinces in Canada. J Pers Med. 2021;11:1–17.
Rainey L, Van Der Waal D, Broeders MJM. Dutch women’s intended participation in a risk-based breast cancer screening and prevention programme: a survey study identifying preferences, facilitators and barriers. BMC Cancer. 2020;20:1–14.
Koitsalu M, Sprangers MAG, Eklund M, Czene K, Hall P, Grönberg H, et al. Public interest in and acceptability of the prospect of risk-stratified screening for breast and prostate cancer. Acta Oncol. 2016;55:45–51.
Woof VG, Ruane H, French DP, Ulph F, Qureshi N, Khan N, et al. The introduction of risk stratified screening into the NHS breast screening Programme: views from British-Pakistani women. BMC Cancer. 2020;20:1–9.
Sierra MA, Wheeler JCW, Devereux L, Trainer AH, Keogh L. Exploring implementation of personal breast cancer risk assessments. J Pers Med. 2021;11:992.
Kelley‐jones C, Scott S, Waller J. Uk women’s views of the concepts of personalised breast cancer risk assessment and risk‐stratified breast screening: a qualitative interview study. Cancers. 2021;13:1–18.
Rainey L, van der Waal D, Wengström Y, Jervaeus A, Broeders MJM. Women’s perceptions of the adoption of personalised risk-based breast cancer screening and primary prevention: a systematic review. Acta Oncol. 2018;57:1275–83.
Ghanouni A, Sanderson SC, Pashayan N, Renzi C, von Wagner C, Waller J. Attitudes towards risk-stratified breast cancer screening among women in England: a cross-sectional survey. J Med Screen. 2019;27:138–45.
Rainey L, Jervaeus A, Donnelly LS, Evans DG, Hammarström M, Hall P, et al. Women’s perceptions of personalized risk-based breast cancer screening and prevention: an international focus group study. Psychooncology. 2019;28:1056–62.
Kaplan CP, Karliner L, Lee A, Livaudais-Toman J, Tice JA, Ozanne E. Acceptability of an mHealth breast cancer risk-reduction intervention promoting risk assessment, education, and discussion of risk in the primary care setting. mHealth. 2021;7:54.
Saya S, McIntosh JG, Winship IM, Clendenning M, Milton S, Oberoi J, et al. A genomic test for colorectal cancer risk: is this acceptable and feasible in primary care? Public Health Genomics. 2020;23:110–21.
Sabatino SA, McCarthy EP, Phillips RS, Burns RB. Breast cancer risk assessment and management in primary care: provider attitudes, practices, and barriers. Cancer Detect Prev. 2007;31:375–83.
Smith SG, Foy R, McGowan JA, Kobayashi LC, DeCensi A, Brown K, et al. Prescribing tamoxifen in primary care for the prevention of breast cancer: a national online survey of GPs’ attitudes. Br J Gen Pract. 2017;67:e414–e427.
Smith SG, Side L, Meisel SF, Horne R, Cuzick J, Wardle J. Clinician-reported barriers to implementing breast cancer chemoprevention in the UK: a qualitative investigation. Public Health Genomics. 2016;19:239–49.
Smith SG, Sestak I, Forster A, Partridge A, Side L, Wolf MS, et al. Factors affecting uptake and adherence to breast cancer chemoprevention: a systematic review and meta-analysis. Ann Oncol. 2016;27:575–90.
Thorneloe RJ, Hall LH, Walter FM, Side L, Lloyd KE, Adamson V, et al. Knowledge of potential harms and benefits of tamoxifen among women considering breast cancer preventive therapy. Cancer Prev Res. 2020;13:411–22.
Thorneloe RJ, Horne R, Side L, Wolf MS, Smith SG, Adamson V, et al. Beliefs about medication and uptake of preventive therapy in women at increased risk of breast cancer: results from a multicenter prospective study. Clin Breast Cancer. 2019;19:e116–e126.
Hackett J, Thorneloe R, Side L, Wolf M, Horne R, Cuzick J, et al. Uptake of breast cancer preventive therapy in the UK: results from a multicentre prospective survey and qualitative interviews. Breast Cancer Res Treat. 2018;170:633–40.
Wernli KJ, Knerr S, Li T, Leppig K, Ehrlich K, Farrell D, et al. Effect of personalized breast cancer risk tool on chemoprevention and breast imaging: ENGAGED-2 trial. JNCI Cancer Spectr. 2021;5:1–9.
Padamsee TJ, Wills CE, Yee LD, Paskett ED. Decision making for breast cancer prevention among women at elevated risk. Breast Cancer Res. 2017;19:1–12.
McIntosh JG, Minshall J, Saya S, Bickerstaffe A, Hewabandu N, Qama A, et al. Benefits and harms of selective oestrogen receptor modulators (SERMs) to reduce breast cancer risk: a cross-sectional study of methods to communicate risk in primary care. Br J Gen Pract. 2019;69:e836–e842.
Holmberg C, Bandos H, Fagerlin A, Bevers TB, Battaglia TA, Wickerham DL, et al. NRG oncology/national surgical adjuvant breast and bowel project decision-making project-1 results: decision-making in breast cancer risk reduction HHS public access. Cancer Prev Res. 2017;10:625–34.
Meiser B, Butow P, Barratt A, Friedlander M, Kirk J, Gaff C, et al. Breast cancer screening uptake in women at increased risk of developing hereditary breast cancer. Breast Cancer Res Treat. 2000;59:101–11.
Smith D, Thomson K, Bambra C, Todd A. The breast cancer paradox: a systematic review of the association between area-level deprivation and breast cancer screening uptake in Europe. Cancer Epidemiol. 2019;60:77–85.
Lee SI, Patel M, Dutton B, Weng S, Luveta J, Qureshi N. Effectiveness of interventions to identify and manage patients with familial cancer risk in primary care: a systematic review. J Community Genet. 2020;11:73–83.
Usher-Smith J, Silarova B, Sharp SJ, Mills K, Griffin SJ. Effect of interventions incorporating personalised cancer risk information on intentions and behaviour: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2018;8:e017717.
French DP, McWilliams L, Howell A, Evans DG. Does receiving high or low breast cancer risk estimates produce a reduction in subsequent breast cancer screening attendance? Cohort study. Breast. 2022;64:47–49.
Harvie M, Pegington M, French D, Cooper G, McDiarmid S, Howell A, et al. Breast cancer risk status influences uptake, retention and efficacy of a weight loss programme amongst breast cancer screening attendees: two randomised controlled feasibility trials. BMC Cancer. 2019;19:1–9.
French DP, Southworth J, Howell A, Harvie M, Stavrinos P, Watterson D, et al. Psychological impact of providing women with personalised 10-year breast cancer risk estimates. Br J Cancer. 2018;118:1648–57.
French DP, Cameron E, Benton JS, Deaton C, Harvie M. Can communicating personalised disease risk promote healthy behaviour change? a systematic review of systematic reviews. Ann Behav Med. 2017;51:718–29.
Hollands GJ, French DP, Griffin SJ, Prevost AT, Sutton S, King S, et al. The impact of communicating genetic risks of disease on risk-reducing health behaviour: systematic review with meta-analysis. BMJ. 2016;352:i1102.
Cooper GC, Harvie MN, French DP. Do negative screening test results cause false reassurance? A systematic review. Br J Health Psychol. 2017;22:958–77.
French DP, Howell A, Evans DG. Psychosocial issues of a population approach to high genetic risk identification: behavioural, emotional and informed choice issues. Breast. 2018;37:148–53.
Schousboe J, Kerlikowske K, Loh A, Cummings S. Personalizing mammography by breast density and other risk factors for breast cancer: analysis of health benefits and cost-effectiveness. Ann Intern Med. 2011;155:10–20.
Van Ravesteyn NT, Miglioretti DL, Stout NK, Lee SJ, Schechter CB, Buist DSM, et al. What level of risk tips the balance of benefits and harms to favor screening mammography starting at age 40: a comparative modeling study of risk. Ann Intern Med. 2012;156:609–17.
Vilaprinyo E, Forné C, Carles M, Sala M, Pla R, Castells X, et al. Cost-effectiveness and harm-benefit analyses of risk-based screening strategies for breast cancer. PLoS ONE. 2014;9:e86858.
Sankatsing VDV, van Ravesteyn NT, Heijnsdijk EAM, Broeders MJM, de Koning HJ. Risk stratification in breast cancer screening: cost-effectiveness and harm-benefit ratios for low-risk and high-risk women. Int J Cancer. 2020;147:3059–67.
Funding
JAU-S and RAD are funded by an Advanced Fellowship from the National Institute for Health and Social Care Research (NIHR300861). SH is funded by a Manchester Cancer Research Centre PhD studentship. DPF is supported by the NIHR Manchester Biomedical Research Centre (IS-BRC-1215-20007). MT was supported by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014). FMW is Director and JE is the Associate Director of the multi-institutional CanTest Collaborative, which is funded by Cancer Research UK (C8640/A23385). SA and FS are funded by a Cancer Research UK programme grant (PPRPGM-Nov20\100002).). JE is supported by an NHMRC Investigator grant (APP1195302). The University of Cambridge has received salary support for DFE from the NHS in the East of England through the Clinical Academic Reserve. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
JAU-S conceived the review and wrote the first draft of the manuscript. All authors contributed to drafting and revising the manuscript and have approved the final version.
Corresponding author
Ethics declarations
Competing interests
DFE and ACA are listed as creators of the BOADICEA v.5 model which has been licensed by Cambridge Enterprise (University of Cambridge).
Ethics approval and consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Usher-Smith, J.A., Hindmarch, S., French, D.P. et al. Proactive breast cancer risk assessment in primary care: a review based on the principles of screening. Br J Cancer 128, 1636–1646 (2023). https://doi.org/10.1038/s41416-023-02145-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02145-w
This article is cited by
-
Multicancer screening test based on the detection of circulating non haematological proliferating atypical cells
Molecular Cancer (2024)
-
Patterns of referrals to regional clinical genetics services for women potentially at above-population level risk of breast cancer
BJC Reports (2024)
-
Understanding the contribution of lifestyle in breast cancer risk prediction: a systematic review of models applicable to Europe
BMC Cancer (2023)
-
“I don’t know what I’m feeling for”: young women’s beliefs about breast cancer risk and experiences of breast awareness
BMC Women's Health (2023)