Abstract
Background
While the 5-year survival rate for local and regional prostate cancer is nearly 100%, it decreases dramatically for advanced tumours. Accessibility to health care is an important factor for cancer prognosis. The U.S. Military Health System (MHS) provides universal health care to its beneficiaries, reducing financial barriers to medical care. However, whether the universal care translates into improved survival among patients with advanced prostate cancer in the MHS is unknown. In this study, we compared the MHS and the U.S. general population in survival of patients with advanced prostate cancer (stages III and IV).
Methods
The MHS patients (N = 5379) were identified from the Department of Defense’s (DoD) Automated Central Tumor Registry (ACTUR). Patients in the U.S. general population (N = 21,516) were identified from the Surveillance, Epidemiology, and End Results (SEER) programme. The two populations were matched on age, race, and diagnosis year.
Results
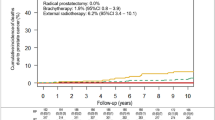
The ACTUR patients exhibited longer 5-year survival than the matched SEER patients (HR = 0.74, 95% CI = 0.67–0.83), after adjustment for the potential confounders. The improved survival was observed for ages 50 years or older, both White patients and Black patients, all tumour stages and grades. This was also demonstrated despite the receipt of surgery or radiation treatment.
Conclusions
MHS beneficiaries with advanced prostate cancer had longer survival than their counterparts in the U.S. general population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data sets generated during and/or analysed during the current study are not publicly available following DoD MHS regulations.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
American Cancer Society. Survival rates for prostate cancer. 2021. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html. Accessed 12 May 2021.
Walker GV, Grant SR, Guadagnolo BA, Hoffman KE, Smith BD, Koshy M, et al. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J Clin Oncol. 2014;32:3118–25.
Lee JM, Wang X, Ojha RP. The effect of health insurance on childhood cancer survival in the United States. Cancer. 2017;123:4878–85.
Aizer AA, Falit B, Mendu ML, Chen MH, Choueiri TK, Hoffman KE, et al. Cancer-specific outcomes among young adults without health insurance. J Clin Oncol. 2014;32:2025–30.
Amini A, Yeh N, Jones BL, Bedrick E, Vinogradskiy Y, Rusthoven CG, et al. Perioperative mortality in nonelderly adult patients with cancer: a population-based study evaluating health care disparities in the United States according to insurance status. J Clin Oncol. 2018;41:476–84.
Ward EM, Fedewa SA, Cokkinides V, Virgo K. The association of insurance and stage at diagnosis among patients aged 55 to 74 years in the national cancer database. Cancer J. 2010;16:614–21.
Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9:222–31.
Slatore CG, Au DH, Gould MK. An official American Thoracic Society systematic review: insurance status and disparities in lung cancer practices and outcomes. Am J Respir Crit Care Med. 2010;182:1195–205.
Wu XC, Lund MJ, Kimmick GG, Richardson LC, Sabatino SA, Chen VW, et al. Influence of race, insurance, socioeconomic status, and hospital type on receipt of guideline-concordant adjuvant systemic therapy for locoregional breast cancers. J Clin Oncol. 2012;30:142–50.
Krimphove MJ, Cole AP, Fletcher SA, Harmouch SS, Berg S, Lipsitz SR, et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:125–36.
Mahal AR, Mahal BA, Nguyen PL, Yu JB. Prostate cancer outcomes for men aged younger than 65 years with Medicaid versus private insurance. Cancer. 2018;124:752–9.
Mahal BA, Aizer AA, Ziehr DR, Hyatt AS, Lago-Hernandez C, Chen YW, et al. The association between insurance status and prostate cancer outcomes: implications for the Affordable Care Act. Prostate Cancer Prostatic Dis. 2014;17:273–9.
Evaluation of the TRICARE program: fiscal year 2020 report to Congress. 2021. https://health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/Annual-Evaluation-of-the-TRICARE-Program. Accessed 13 Apr 2021.
Lin J, Kamamia C, Brown D, Shao S, McGlynn KA, Nations JA, et al. Survival among lung cancer patients in the U.S. Military Health System: a comparison with the SEER population. Cancer Epidemiol Biomark Prev. 2018;27:673–9.
Ru Y, Liu J, Fantacone-Campbell JL, Zhu K, Kovatich AJ, Hooke JA, et al. Comparative survival analysis of invasive breast cancer patients treated by a U.S. Military Medical Center and matched patients from the U.S. general population. Mil Med. 2017;182:e1851–8.
Lin J, McGlynn KA, Shriver CD, Zhu K. Comparison of survival among colon cancer patients in the U.S. Military Health System and patients in the Surveillance, Epidemiology, and End Results (SEER) Program. Cancer Epidemiol Biomark Prev. 2021;30:1359–65.
Lin J, Bytnar JA, Theeler BJ, McGlynn KA, Shriver CD, Zhu K. Survival among patients with glioma in the US Military Health System: a comparison with patients in the Surveillance, Epidemiology, and End Results program. Cancer. 2020;126:3053–60.
Negoita S, Feuer EJ, Mariotto A, Cronin KA, Petkov VI, Hussey SK, et al. Annual Report to the Nation on the Status of Cancer, part II: recent changes in prostate cancer trends and disease characteristics. Cancer. 2018;124:2801–14.
Wong AT, Rineer J, Schwartz D, Becker D, Safdieh J, Osborn V, et al. Effect of thoracic radiotherapy timing and fractionation on survival in nonmetastatic small cell lung carcinoma. Clin Lung Cancer. 2017;18:207–12.
Registry groupings in SEER data and statistics. 2021. https://seer.cancer.gov/registries/terms.html. Accessed 12 Apr 2021.
National Cancer Institute. Prostate cancer treatment - health professional version. Pathology. 2021. https://www.cancer.gov/types/prostate/hp/prostate-treatment-pdq#_1686_toc. Accessed 28 Jun 2021.
World Health Organization. International classification of diseases for oncology, 3rd edition (ICD-O-3). 2021. https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf. Accessed 13 Apr 2021.
American Joint Committee on Cancer. AJCC cancer staging manual, sixth edition. In: Greene FL, Page DL, Flemming ID, et al. editors. Chicago, IL: Springer; 2002.
American Cancer Society. Screening tests for prostate cancer: prostate-specific antigen (PSA) blood test. 2022. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/tests.html. Accessed 19 Jan 2022.
Barry MJ. Clinical practice. Prostate-specific-antigen testing for early diagnosis of prostate cancer. N Engl J Med. 2001;344:1373–7.
Wang M, Spiegelman D, Kuchiba A, Lochhead P, Kim S, Chan AT, et al. Statistical methods for studying disease subtype heterogeneity. Stat Med. 2016;35:782–800.
Mahal BA, Ziehr DR, Aizer AA, Hyatt AS, Sammon JD, Schmid M, et al. Getting back to equal: The influence of insurance status on racial disparities in the treatment of African American men with high-risk prostate cancer. Urol Oncol. 2014;32:1285–91.
Niu X, Roche LM, Pawlish KS, Henry KA. Cancer survival disparities by health insurance status. Cancer Med. 2013;2:403–11.
Fossati N, Nguyen DP, Trinh QD, Sammon J, Sood A, Larcher A, et al. The impact of insurance status on tumor characteristics and treatment selection in contemporary patients with prostate cancer. J Natl Compr Canc Netw. 2015;13:1351–8.
Fedewa SA, Etzioni R, Flanders WD, Jemal A, Ward EM. Association of insurance and race/ethnicity with disease severity among men diagnosed with prostate cancer, National Cancer Database 2004-2006. Cancer Epidemiol Biomark Prev. 2010;19:2437–44.
Liu W, Goodman M, Filson CP. Association of state-level Medicaid expansion with treatment of patients with higher-risk prostate cancer. JAMA Netw Open. 2020;3:e2015198.
Beebe-Dimmer JL, Ruterbusch JJ, Cooney KA, Bolton A, Schwartz K, Schwartz AG, et al. Racial differences in patterns of treatment among men diagnosed with de novo advanced prostate cancer: a SEER-Medicare investigation. Cancer Med. 2019;8:3325–35.
Potosky AL, Merrill RM, Riley GF, Taplin SH, Barlow W, Fireman BH, et al. Prostate cancer treatment and ten-year survival among group/staff HMO and fee-for-service Medicare patients. Health Serv Res. 1999;34:525–46.
Sadetsky N, Elkin EP, Latini DM, DuChane J, Carroll PR. Prostate cancer outcomes among older men: insurance status comparisons results from CaPSURE database. Prostate Cancer Prostatic Dis. 2008;11:280–7.
Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, Davidson KW, et al. Screening for prostate cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319:1901–13.
The evaluation of the TRICARE program: fiscal year 2019 report to Congress. 2019. https://health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/Annual-Evaluation-of-the-TRICARE-Program. Accessed 24 Jul 2019.
Prostate cancer exams. TRICARE Covered Services. 2021. https://www.tricare.mil/CoveredServices/IsItCovered/ProstateCancerExams. Accessed 12 May 2021.
Optenberg SA, Thompson IM, Friedrichs P, Wojcik B, Stein CR, Kramer B. Race, treatment, and long-term survival from prostate cancer in an equal-access medical care delivery system. JAMA. 1995;274:1599–605.
Riviere P, Luterstein E, Kumar A, Vitzthum LK, Deka R, Sarkar RR, et al. Survival of African American and non-Hispanic white men with prostate cancer in an equal-access health care system. Cancer. 2020;126:1683–90.
Graham-Steed T, Uchio E, Wells CK, Aslan M, Ko J, Concato J. ‘Race’ and prostate cancer mortality in equal-access healthcare systems. Am J Med. 2013;126:1084–8.
Daskivich TJ, Kwan L, Dash A, Litwin MS. Racial parity in tumor burden, treatment choice and survival outcomes in men with prostate cancer in the VA healthcare system. Prostate Cancer Prostatic Dis. 2015;18:104–9.
Alexander M, Zhu K, Cullen J, Byrne C, Brown D, Shao S, et al. Race and overall survival in men diagnosed with prostate cancer in the Department of Defense Military Health System, 1990-2010. Cancer Causes Control. 2019;30:627–35.
Acknowledgements
The authors thank the Joint Pathology Center and the Surveillance, Epidemiology, and End Results (SEER) programme for the use of the cancer registry data.
Funding
This project was supported by John P. Murtha Cancer Center Research Program, Uniformed Services University of the Health Sciences under the auspices of the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc.
Author information
Authors and Affiliations
Contributions
Each of the authors (JL, DN, JJ, GTC, CDS, and KZ) significantly contributed to the project conception that led to data acquisition and results interpretation. All authors contributed to manuscript drafting, revision, and final approval. The corresponding author (KZ) confirmed that he had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was based on the non-identifiable ACTUR data and SEER de-identified public use data. The study was approved by the institutional review board of Walter Reed National Military Medical Center. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, J., Nousome, D., Jiang, J. et al. Five-year survival of patients with late-stage prostate cancer: comparison of the Military Health System and the U.S. general population. Br J Cancer 128, 1070–1076 (2023). https://doi.org/10.1038/s41416-022-02136-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-02136-3
This article is cited by
-
Inducing apoptosis by using microRNA in radio-resistant prostate cancer: an in-silico study with an in-vitro validation
Molecular Biology Reports (2023)