Abstract
Transgender individuals represent 0.55% of the US population, equivalent to 1.4 million transgender adults. In transgender women, feminisation can include a number of medical and surgical interventions. The main goal is to deprive the phenotypically masculine body of androgens and simultaneously provide oestrogen therapy for feminisation. In gender-confirming surgery (GCS) for transgender females, the prostate is usually not removed. Due to limitations of existing cohort studies, the true incidence of prostate cancer in transgender females is unknown but is thought to be less than the incidence among cis-gender males. It is unclear how prostate cancer develops in androgen-deprived conditions in these patients. Six out of eleven case reports in the literature presented with metastatic disease. It is thought that androgen receptor-mediated mechanisms or tumour-promoting effects of oestrogen may be responsible. Due to the low incidence of prostate cancer identified in transgender women, there is little evidence to drive specific screening recommendations in this patient subpopulation. The treatment of early and locally advanced prostate cancer in these patients warrants an individualised thoughtful approach with input from patients’ reconstructive surgeons. Both surgical and radiation treatment for prostate cancer in these patients can profoundly impact the patient’s quality of life. In this review, we discuss the evidence surrounding screening and treatment of prostate cancer in transgender women and consider the current gaps in our knowledge in providing evidence-based guidance at the molecular, genomic and epidemiological level, for clinical decision-making in the management of these patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Not applicable.
References
Cooper K, Russell A, Mandy W, Butler C. The phenomenology of gender dysphoria in adults: a systematic review and meta-synthesis. Clin Psychol Rev. 2020;80:101875.
Baker KE. Findings from the behavioral risk factor surveillance system on health-related quality of life among US transgender adults, 2014-2017. JAMA Intern Med. 2019;179:1141–4.
Flores AR, Brown TN, Herman J. Race and ethnicity of adults who identify as transgender in the United States. CA: Williams Institute, UCLA School of Law Los Angeles; 2016.
James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi, M. The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality, Washington, DC. 2016.
Badgett MV, Choi SK, Wilson BDM. LGBT poverty in the United States: a study of differences between sexual orientation and gender identity groups (2019). https://williamsinstitute.law.ucla.edu/wp-content/uploads/National-LGBT-Poverty-Oct-2019.pdf.
Jackson SS, Han X, Mao Z, Nogueira L, Suneja G, Jemal A, et al. Cancer stage, treatment, and survival among transgender patients in the United States. J Natl Cancer Inst. 2021;113:1221–7.
Rosser BRS, Capistrant B, Torres B, Konety B, Merengwa E, Mitteldorf D, et al. The effects of radical prostatectomy on gay and bisexual men’s mental health, sexual identity and relationships: qualitative results from the restore study. Sex Relatsh Ther. 2016;31:446–61.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA: A Cancer J Clin. 2021;71:7–33.
Viale PH. The American Cancer Society’s facts & figures: 2020 edition. J Adv Pr Oncol. 2020;11:135–6.
American Cancer Society. Cancer Facts & Figures 2021. Atlanta: American Cancer Society. 2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf.
Pritzlaff M, Tian Y, Reineke P, Stuenkel AJ, Allen K, Gutierrez S, et al. Diagnosing hereditary cancer predisposition in men with prostate cancer. Genet Med. 2020;22:1517–23.
Thurston AV. Carcinoma of the prostate in a transsexual. Br J Urol. 1994;73:217.
van Haarst EP, Newling DW, Gooren LJ, Asscheman H, Prenger DM. Metastatic prostatic carcinoma in a male-to-female transsexual. Br J Urol. 1998;81:776.
Miksad RA, Bubley G, Church P, Sanda M, Rofsky N, Kaplan I, et al. Prostate cancer in a transgender woman 41 years after initiation of feminization. J Am Med Assoc. 2006;296:2316–7.
Dorff TB, Shazer RL, Nepomuceno EM, Tucker SJ. Successful treatment of metastatic androgen-independent prostate carcinoma in a transsexual patient. Clin Genitourin Cancer. 2007;5:344–6.
Turo R, Jallad S, Prescott S, Cross WR. Metastatic prostate cancer in transsexual diagnosed after three decades of estrogen therapy. Can Urol Assoc J. 2013;7:E544–546.
Ellent E, Matrana MR. Metastatic prostate cancer 35 years after sex reassignment surgery. Clin Genitourin Cancer. 2016;14:e207–209.
Deebel NA, Morin JP, Autorino R, Vince R, Grob B, Hampton LJ. Prostate cancer in transgender women: incidence, etiopathogenesis, and management challenges. Urology. 2017;110:166–71.
Sharif A, Malhotra NR, Acosta AM, Kajdacsy-Balla AA, Bosland M, Guzman G, et al. The development of prostate adenocarcinoma in a transgender male to female patient: could estrogen therapy have played a role? Prostate. 2017;77:824–8.
Ingham MD, Lee RJ, MacDermed D, Olumi AF. Prostate cancer in transgender women. Urol Oncol. 2018;36:518–25.
Bertoncelli Tanaka M, Sahota K, Burn J, Falconer A, Winkler M, Ahmed HU, et al. Prostate cancer in transgender women: what does a urologist need to know? BJU Int. 2022;129:113–22.
Gooren L, Morgentaler A. Prostate cancer incidence in orchidectomised male-to-female transsexual persons treated with oestrogens. Andrologia. 2014;46:1156–60.
Silverberg MJ, Nash R, Becerra-Culqui TA, Cromwell L, Getahun D, Hunkeler E, et al. Cohort study of cancer risk among insured transgender people. Ann Epidemiol. 2017;27:499–501.
Nash R, Ward KC, Jemal A, Sandberg DE, Tangpricha V, Goodman M. Frequency and distribution of primary site among gender minority cancer patients: an analysis of U.S. national surveillance data. Cancer Epidemiol. 2018;54:1–6.
Braun H, Nash R, Tangpricha V, Brockman J, Ward K, Goodman M. Cancer in transgender people: evidence and methodological considerations. Epidemiol Rev. 2017;39:93–107.
de Nie I, de Blok CJM, van der Sluis TM, Barbé E, Pigot GLS, Wiepjes CM, et al. Prostate cancer incidence under androgen deprivation: nationwide cohort study in trans women receiving hormone treatment. J Clin Endocrinol Metab. 2020;105:e3293–e3299.
Siegel DA, O’Neil ME, Richards TB, Dowling NF, Weir HK. Prostate cancer incidence and survival, by stage and race/ethnicity—United States, 2001–2017. Morbidity Mortal Wkly Rep. 2020;69:1473.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Gooren L. Hormone treatment of the adult transsexual patient. Horm Res. 2005;64:31–36.
Moore E, Wisniewski A, Dobs A. Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab. 2003;88:3467–73.
Stroumsa D, Crissman HP, Dalton VK, Kolenic G, Richardson CR. Insurance coverage and use of hormones among transgender respondents to a national survey. Ann Fam Med. 2020;18:528.
Huggins C, Hodges CV. Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. 1941. J Urol. 2002;168:9–12.
Tsukamoto S, Akaza H, Onozawa M, Shirai T, Ideyama Y. A five-alpha reductase inhibitor or an antiandrogen prevents the progression of microscopic prostate carcinoma to macroscopic carcinoma in rats. Cancer. 1998;82:531–7.
Wibowo E, Schellhammer P, Wassersug RJ. Role of estrogen in normal male function: clinical implications for patients with prostate cancer on androgen deprivation therapy. J Urol. 2011;185:17–23.
Dal Pra A, Cury F, Souhami L. Combining radiation therapy and androgen deprivation for localized prostate cancer—a critical review. Curr Oncol. 2010;17:28–38.
Crowley F, Sterpi M, Buckley C, Margetich L, Handa S, Dovey Z. A review of the pathophysiological mechanisms underlying castration-resistant prostate cancer. Res Rep. Urol. 2021;13:457–72.
Citrin DL, Resnick MI, Guinan P, al-Bussam N, Scott M, Gau TC, et al. A comparison of Zoladex and DES in the treatment of advanced prostate cancer: results of a randomized, multicenter trial. Prostate. 1991;18:139–46.
Bosland MC. The role of estrogens in prostate carcinogenesis: a rationale for chemoprevention. Rev Urol. 2005;7:S4–S10.
Nelles JL, Hu W-Y, Prins GS. Estrogen action and prostate cancer. Expert Rev Endocrinol Metab. 2011;6:437–51.
Bosland MC. A perspective on the role of estrogen in hormone-induced prostate carcinogenesis. Cancer Lett. 2013;334:28–33.
Kruithof-Dekker IG, Têtu B, Janssen PJ, Van der Kwast TH. Elevated estrogen receptor expression in human prostatic stromal cells by androgen ablation therapy. J Urol. 1996;156:1194–7.
Lundon DJ, Boland A, Prencipe M, Hurley G, O’Neill A, Kay E, et al. The prognostic utility of the transcription factor SRF in docetaxel-resistant prostate cancer: in-vitro discovery and in-vivo validation. BMC Cancer. 2017;17:1–13.
Takizawa I, Lawrence MG, Balanathan P, Rebello R, Pearson HB, Garg E, et al. Estrogen receptor alpha drives proliferation in PTEN-deficient prostate carcinoma by stimulating survival signaling, MYC expression and altering glucose sensitivity. Oncotarget. 2015;6:604–16.
Megas G, Chrisofos M, Anastasiou I, Tsitlidou A, Choreftaki T, Deliveliotis C. Estrogen receptor (alpha and beta) but not androgen receptor expression is correlated with recurrence, progression and survival in post prostatectomy T3N0M0 locally advanced prostate cancer in an urban Greek population. Asian J Androl. 2015;17:98–105.
Prins GS, Korach KS. The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids. 2008;73:233–44.
Di Zazzo E, Galasso G, Giovannelli P, Di Donato M, Bilancio A, Perillo B, et al. Estrogen receptors in epithelial-mesenchymal transition of prostate cancer. Cancers. 2019;11:1418.
Landstrom M, Damber JE, Bergh A. Estrogen treatment postpones the castration-induced dedifferentiation of Dunning R3327-PAP prostatic adenocarcinoma. Prostate. 1994;25:10–18.
Langley RE, Gilbert DC, Duong T, Clarke NW, Nankivell M, Rosen SD, et al. Transdermal oestradiol for androgen suppression in prostate cancer: long-term cardiovascular outcomes from the randomised prostate adenocarcinoma transcutaneous hormone (PATCH) trial programme. Lancet. 2021;397:581–91.
Langley RE, Kynaston HG, Alhasso AA, Duong T, Paez EM, Jovic G, et al. A randomised comparison evaluating changes in bone mineral density in advanced prostate cancer: luteinising hormone-releasing hormone agonists versus transdermal oestradiol. Eur Urol. 2016;69:1016–25.
Geier R, Adler S, Rashid G, Klein A. The synthetic estrogen diethylstilbestrol (DES) inhibits the telomerase activity and gene expression of prostate cancer cells. Prostate. 2010;70:1307–12.
Dobbs RW, Malhotra NR, Greenwald DT, Wang AY, Prins GS, Abern MR. Estrogens and prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:185–94.
Manikandan R, Srirangam SJ, Pearson E, Brown SC, O’Reilly P, Collins GN. Diethylstilboestrol versus bicalutamide in hormone refractory prostate carcinoma: a prospective randomized trial. Urol Int. 2005;75:217–21.
Byar DP, Corle DK. Hormone therapy for prostate cancer: results of the Veterans Administration Cooperative Urological Research Group studies. NCI Monogr. 1988;7:165–70.
Veterans Administration Co-operative Urological Research Group. Treatment and survival of patients with cancer of the prostate. Surg Gynecol Obstet. 1967;124:1011–7.
Di Zazzo E, Galasso G, Giovannelli P, Di Donato M, Castoria G. Estrogens and their receptors in prostate cancer: therapeutic implications. Front Oncol. 2018;8:2.
Bergan RC, Reed E, Myers CE, Headlee D, Brawley O, Cho H-K, et al. A Phase II study of high-dose tamoxifen in patients with hormone-refractory prostate cancer. Clin Cancer Res. 1999;5:2366–73.
Stein S, Zoltick B, Peacock T, Holroyde C, Haller D, Armstead B, et al. Phase II trial of toremifene in androgen-independent prostate cancer: a Penn cancer clinical trials group trial. Am J Clin Oncol. 2001;24:283–5.
Fujimura T, Takahashi S, Kume H, Urano T, Takayama K, Yamada Y, et al. Toremifene, a selective estrogen receptor modulator, significantly improved biochemical recurrence in bone metastatic prostate cancer: a randomized controlled phase II a trial. BMC Cancer. 2015;15:1–8.
Ho TH, Nunez-Nateras R, Hou Y-X, Bryce AH, Northfelt DW, Dueck AC, et al. A study of combination bicalutamide and raloxifene for patients with castration-resistant prostate cancer. Clin Genitourin Cancer. 2017;15:196–202. e191
Shang Y, Brown M. Molecular determinants for the tissue specificity of SERMs. Science. 2002;295:2465–8.
Martinkovich S, Shah D, Planey SL, Arnott JA. Selective estrogen receptor modulators: tissue specificity and clinical utility. Clin Inter Aging. 2014;9:1437–52.
Bosland MC, Huang J, Schlicht MJ, Enk E, Xie H, Kato I. Impact of 18-month soy protein supplementation on steroid hormones and serum biomarkers of angiogenesis, apoptosis, and the growth hormone/IGF-1 axis: results of a randomized, placebo-controlled trial in males following prostatectomy. Nutr Cancer. 2022;74:110–21.
Bonkhoff H. Estrogen receptor signaling in prostate cancer: implications for carcinogenesis and tumor progression. Prostate. 2018;78:2–10.
Harris WP, Mostaghel EA, Nelson PS, Montgomery B. Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol. 2009;6:76–85.
Koochekpour S. Androgen receptor signaling and mutations in prostate cancer. Asian J Androl. 2010;12:639.
Montgomery RB, Mostaghel EA, Vessella R, Hess DL, Kalhorn TF, Higano CS, et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 2008;68:4447.
Pernigoni N, Zagato E, Calcinotto A, Troiani M, Mestre RP, Calì B, et al. Commensal bacteria promote endocrine resistance in prostate cancer through androgen biosynthesis. Science. 2021;374:216–24.
Fixemer T, Remberger K, Bonkhoff H. Differential expression of the estrogen receptor beta (ERbeta) in human prostate tissue, premalignant changes, and in primary, metastatic, and recurrent prostatic adenocarcinoma. Prostate. 2003;54:79–87.
Bonkhoff H, Fixemer T, Hunsicker I, Remberger K. Estrogen receptor expression in prostate cancer and premalignant prostatic lesions. Am J Pathol. 1999;155:641–7.
Bonkhoff H, Fixemer T, Hunsicker I, Remberger K. Progesterone receptor expression in human prostate cancer: correlation with tumor progression. Prostate. 2001;48:285–91.
Shaw GL, Whitaker H, Corcoran M, Dunning MJ, Luxton H, Kay J, et al. The early effects of rapid androgen deprivation on human prostate cancer. Eur Urol. 2016;70:214–8.
Balk SP, Ko YJ, Bubley GJ. Biology of prostate-specific antigen. J Clin Oncol. 2003;21:383–91.
Schröder FH, Carter HB, Wolters T, van den Bergh RC, Gosselaar C, Bangma CH, et al. Early detection of prostate cancer in 2007. Part 1: PSA and PSA kinetics. Eur Urol. 2008;53:468–77.
Merriel SWD, Pocock L, Gilbert E, Creavin S, Walter FM, Spencer A, et al. Systematic review and meta-analysis of the diagnostic accuracy of prostate-specific antigen (PSA) for the detection of prostate cancer in symptomatic patients. BMC Med. 2022;20:54.
Force USPST. Screening for prostate cancer: US preventive services task force recommendation statement. J Am Med Assoc. 2018;319:1901–13.
Carter HB, Albertsen PC, Barry MJ, Etzioni R, Freedland SJ, Greene KL, et al. Early detection of prostate cancer: AUA guideline. J Urol. 2013;190:419–26.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29.
Naji L, Randhawa H, Sohani Z, Dennis B, Lautenbach D, Kavanagh O, et al. Digital rectal examination for prostate cancer screening in primary care: a systematic review and meta-analysis. Ann Fam Med. 2018;16:149–54.
Butler SS, Muralidhar V, Zhao SG, Sanford NN, Franco I, Fullerton ZH, et al. Prostate cancer incidence across stage, NCCN risk groups, and age before and after USPSTF Grade D recommendations against prostate-specific antigen screening in 2012. Cancer. 2020;126:717–24.
Fleshner K, Carlsson SV, Roobol MJ. The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat Rev Urol. 2017;14:26–37.
Catalona William J, Richie Jerome P, Ahmann Frederick R, Hudson M’Liss A, Scardino Peter T, Flanigan Robert C, et al. Comparison of digital rectal examination and serum prostate specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 men. J Urol. 1994;151:1283–90.
Richie JP, Catalona WJ, Ahmann FR, Hudson MA, Scardino PT, Flanigan RC, et al. Effect of patient age on early detection of prostate cancer with serum prostate-specific antigen and digital rectal examination. Urology. 1993;42:365–74.
Okotie OT, Roehl KA, Han M, Loeb S, Gashti SN, Catalona WJ. Characteristics of prostate cancer detected by digital rectal examination only. Urology. 2007;70:1117–20.
Gosselaar C, Roobol MJ, Roemeling S, Schröder FH. The role of the digital rectal examination in subsequent screening visits in the European randomized study of screening for prostate cancer (ERSPC), Rotterdam. Eur Urol. 2008;54:581–8.
Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab. 2017;102:3869–903.
Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13:165–232.
Weyers S, De Sutter P, Hoebeke S, Monstrey G, G TS, Verstraelen H, et al. Gynaecological aspects of the treatment and follow-up of transsexual men and women. Facts Views Vis Obgyn. 2010;2:35–54.
Rastrelli G, Corona G, Vignozzi L, Maseroli E, Silverii A, Monami M, et al. Serum PSA as a predictor of testosterone deficiency. J Sex Med. 2013;10:2518–28.
Trum HW, Hoebeke P, Gooren LJ. Sex reassignment of transsexual people from a gynecologist’s and urologist’s perspective. Acta Obstet Gynecol Scand. 2015;94:563–7.
Ahmed HU, Bosaily AE-S, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22.
Drost FJH, Osses DF, Nieboer D, Steyerberg EW, Bangma CH, Roobol MJ, et al. Prostate MRI, with or without MRI‐targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst Rev. 2019;4. https://doi.org/10.1002/14651858.CD012663.pub2.
Eldred-Evans D, Burak P, Connor MJ, Day E, Evans M, Fiorentino F, et al. Population-based prostate cancer screening with magnetic resonance imaging or ultrasonography: the IP1-PROSTAGRAM study. JAMA Oncol. 2021;7:395–402.
Stowell JT, Grimstad FW, Kirkpatrick DL, Brown ER, Santucci RA, Crane C, et al. Imaging findings in transgender patients after gender-affirming surgery. RadioGraphics. 2019;39:1368–92.
Jin B, Turner L, Walters WA, Handelsman DJ. The effects of chronic high dose androgen or estrogen treatment on the human prostate [corrected]. J Clin Endocrinol Metab. 1996;81:4290–5.
Starobinets O, Kurhanewicz J, Noworolski SM. Improved multiparametric MRI discrimination between low-risk prostate cancer and benign tissues in a small cohort of 5α-reductase inhibitor treated individuals as compared with an untreated cohort. NMR Biomed. 2017;30:e3696.
Gormley GJ, Ng J, Cook T, Stoner E, Guess H, Walsh P. Effect of finasteride on prostate-specific antigen density. Urology. 1994;43:53–58.
Parsi M, Desai MH, Desai D, Singhal S, Khandwala PM, Potdar RR. PSMA: a game changer in the diagnosis and treatment of advanced prostate cancer. Med Oncol. 2021;38:89.
Eder M, Schäfer M, Bauder-Wüst U, Hull WE, Wängler C, Mier W, et al. 68Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug Chem. 2012;23:688–97.
FDA approves first PSMA-targeted PET drug. J Nucl Med. 2021;62:11N. https://jnm.snmjournals.org/content/62/2/11N.2.long.
Emmett L, Buteau J, Papa N, Moon D, Thompson J, Roberts MJ, et al. The additive diagnostic value of prostate-specific membrane antigen positron emission tomography computed tomography to multiparametric magnetic resonance imaging triage in the diagnosis of prostate cancer (PRIMARY): a prospective multicentre study. Eur Urol. 2021;80:682–9.
Starobinets O, Kurhanewicz J, Noworolski SM. Improved multiparametric MRI discrimination between low-risk prostate cancer and benign tissues in a small cohort of 5alpha-reductase inhibitor treated individuals as compared with an untreated cohort. NMR Biomed. 2017;30:e3696.
Diao W, Cai H, Chen L, Jin X, Liao X, Jia Z. Recent advances in prostate-specific membrane antigen-based radiopharmaceuticals. Curr Top Med Chem. 2019;19:33–56.
Li JZ, Tu HYV, Avram R, Pinthus J, Bordeleau L, Hodgson N. Cancer prevention and screening in a BRCA2-positive male to female transgender patient. Breast J. 2018;24:1112–3.
Colebunders B, T’Sjoen G, Weyers S, Monstrey S. Hormonal and surgical treatment in trans-women with BRCA1 mutations: a controversial topic. J Sex Med. 2014;11:2496–9.
Nyberg T, Frost D, Barrowdale D, Evans DG, Bancroft E, Adlard J, et al. Prostate cancer risks for male BRCA1 and BRCA2 mutation carriers: a prospective cohort study. Eur Urol. 2020;77:24–35.
Forbes C, Fayter D, de Kock S, Quek RG. A systematic review of international guidelines and recommendations for the genetic screening, diagnosis, genetic counseling, and treatment of BRCA-mutated breast cancer. Cancer Manag Res. 2019;11:2321.
Clarke CN, Cortina CS, Fayanju OM, Dossett LA, Johnston FM, Wong SL. Breast cancer risk and screening in transgender persons: a call for inclusive care. Ann Surgical Oncol. 2022;29:2176–80.
D’Andrea S, Pallotti F, Senofonte G, Castellini C, Paoli D, Lombardo F, et al. Polymorphic cytosine-adenine-guanine repeat length of androgen receptor gene and gender incongruence in trans women: a systematic review and meta-analysis of case-control studies. J Sex Med. 2020;17:543–50.
Bostwick DG, Qian J, Civantos F, Roehrborn CG, Montironi R. Does finasteride alter the pathology of the prostate and cancer grading? Clin Prostate Cancer. 2004;2:228–35.
Mohler JL, Antonarakis ES, Armstrong AJ, D’Amico AV, Davis BJ, Dorff T, et al. Prostate cancer, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17:479–505.
McClintock TR, von Landenberg N, Cole AP, Lipsitz SR, Gild P, Sun M, et al. Neoadjuvant androgen deprivation therapy prior to radical prostatectomy: recent trends in utilization and association with postoperative surgical margin status. Ann Surg Oncol. 2019;26:297–305.
Ginsburg KB, Curtis GL, Timar RE, George AK, Cher ML. Delayed radical prostatectomy is not associated with adverse oncologic outcomes: implications for men experiencing surgical delay due to the COVID-19 pandemic. J Urol. 2020;204:720–5.
Berli JU, Knudson G, Fraser L, Tangpricha V, Ettner R, Ettner FM, et al. What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg. 2017;152:394–400.
Grigsby PW, Russell A, Bruner D, Eifel P, Koh W-J, Spanos W, et al. Late injury of cancer therapy on the female reproductive tract. Int J Radiat Oncol* Biol* Phys. 1995;31:1281–99.
Mayadev J, Merrick GS, Reed JR, Butler WM, Galbreath RW, Allen ZA, et al. Permanent prostate brachytherapy in prostate glands <20 cm(3). Int J Radiat Oncol Biol Phys. 2010;76:1450–5.
Chung E, Stenmark MH, Evans C, Narayana V, McLaughlin PW. Greater postimplant swelling in small-volume prostate glands: implications for dosimetry, treatment planning, and operating room technique. Int J Radiat Oncol Biol Phys. 2012;82:1944–8.
Kovtun KA, Wolfsberger L, Niedermayr T, Sugar EN, Graham PL, Murciano-Goroff Y, et al. Dosimetric quality and evolution of edema after low-dose-rate brachytherapy for small prostates: implications for the use of newer isotopes. Brachytherapy. 2014;13:152–6.
Sanguineti G, Marcenaro M, Franzone P, Tognoni P, Barra S, Vitale V. Is there a “curative” role of radiotherapy for clinically localized hormone refractory prostate cancer? Am J Clin Oncol. 2004;27:264–8.
Jackson WC, Hartman HE, Dess RT, Birer SR, Soni PD, Hearn JWD, et al. Addition of androgen-deprivation therapy or brachytherapy boost to external beam radiotherapy for localized prostate cancer: a network meta-analysis of randomized trials. J Clin Oncol. 2020;38:3024–31.
Almazan AN, Keuroghlian AS. Association between gender-affirming surgeries and mental health outcomes. JAMA Surg. 2021;156:611–8.
Chen YC, Lin PH, Jou YY, Lin VC. Surgical treatment for urinary incontinence after prostatectomy: a meta-analysis and systematic review. PLoS ONE. 2017;12:e0130867.
Purohit R, Blaivas Jerry G, Kalkan S. V12-03 autologous rectus fascial pubovaginal sling after vaginoplasty: an old trick for a new problem. J Urol. 2019;201:e1205–e1205.
Schaeffer E, Srinivas S, Antonarakis ES, Armstrong AJ, Bekelman JE, Cheng H, et al. NCCN guidelines insights: prostate cancer, version 1.2021: featured updates to the NCCN guidelines. J Natl Compr Cancer Netw. 2021;19:134–43.
Sweeney CJ, Chen Y-H, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737–46.
Smith MR, Hussain M, Saad F, Fizazi K, Sternberg CN, Crawford ED, et al. Darolutamide and survival in metastatic, hormone-sensitive prostate cancer. New Engl J Med. 2022; https://doi.org/10.1056/NEJMoa2119115.
Clarke NW, Ali A, Ingleby FC, Hoyle A, Amos CL, Attard G, et al. Addition of docetaxel to hormonal therapy in low- and high-burden metastatic hormone sensitive prostate cancer: long-term survival results from the STAMPEDE trial. Ann Oncol. 2019;30:1992–2003.
Markland C. Transexual surgery. Obstet Gynecol Annu. 1975;4:309–30.
Sada YH. A Dozen Eggs. J Clin Oncol. 2021;39:3645–6.
Molokwu CN, Appelbaum JS, Miksad RA. Detection of prostate cancer following gender reassignment. BJU Int. 2008;101:259; author reply 259–60.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
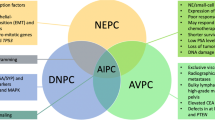
The manuscript was conceptualised and designed by NK, RSP and DJL. Literature review was performed by FC, MM, SG and DJL. Tables and figures were prepared by FC, MM, SG and DJL. FC, MM, SG, NK and DJL wrote and prepared the initial draft. AKT, CT, MD, NK, RSJ and DJL reviewed, edited and revised the manuscript at all points. All authors read and approved the final version of the manuscript. Figure 1 was created with BioRender.com.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
AKT certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g., employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received or pending), are the following: AKT has served as a site PI on pharma/industry-sponsored clinical trials from Kite Pharma Inc., Lumicell, Inc., Dendron Pharmaceuticals, LLC, Oncovir Inc., Blue Earth Diagnostics Ltd., RhoVac ApS., Bayer HealthCare Pharmaceuticals Inc., and Janssen Research and Development, LLC; has received research funding (grants) to his institution from DOD, NIH, Axogen, Intuitive Surgical, AMBF and other philanthropy; has served as an unpaid consultant to Roivant Biosciences and advisor to Promaxo; and owns equity in Promaxo. The remaining authors declare no competing interests in relation to the work described.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Crowley, F., Mihalopoulos, M., Gaglani, S. et al. Prostate cancer in transgender women: considerations for screening, diagnosis and management. Br J Cancer 128, 177–189 (2023). https://doi.org/10.1038/s41416-022-01989-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01989-y
This article is cited by
-
Cancer surveillance for transgender and gender diverse patients with Lynch syndrome: a practice resource of the Collaborative Group of the Americas on Inherited Gastrointestinal Cancer
Familial Cancer (2023)
-
Prostate Cancer in Transgender Women: Epidemiology, Clinical Characteristics, and Management Challenges
Current Oncology Reports (2023)