Abstract
Background
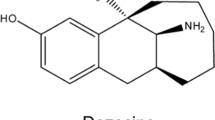
It has been considered that activation of peripheral μ-opioid receptors (MORs) induces side effects of opioids. In this study, we investigated the possible improvement of the immune system in tumour-bearing mice by systemic administration of the peripheral MOR antagonist naldemedine.
Methods
The inhibitory effect of naldemedine on MOR-mediated signalling was tested by cAMP inhibition and β-arrestin recruitment assays using cultured cells. We assessed possible changes in tumour progression and the number of splenic lymphocytes in tumour-bearing mice under the repeated oral administration of naldemedine.
Results
Treatment with naldemedine produced a dose-dependent inhibition of both the decrease in the cAMP level and the increase in β-arrestin recruitment induced by the MOR agonists. Repeated treatment with naldemedine at a dose that reversed the morphine-induced inhibition of gastrointestinal transport, but not antinociception, significantly decreased tumour volume and prolonged survival in tumour-transplanted mice. Naldemedine administration significantly decreased the increased expression of immune checkpoint-related genes and recovered the decreased level of toll-like receptor 4 in splenic lymphocytes in tumour-bearing mice.
Conclusions
The blockade of peripheral MOR may induce an anti-tumour effect through the recovery of T-cell exhaustion and promotion of the tumour-killing system.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data presented within the article are available upon request from the corresponding author.
References
Trang T, Al-Hasani R, Salvemini D, Salter MW, Gutstein H, Cahill CM. Pain and poppies: the good, the bad, and the ugly of opioid analgesics. J Neurosci. 2015;35:13879–88.
Peng J, Sarkar S, Chang SL. Opioid receptor expression in human brain and peripheral tissues using absolute quantitative real-time RT-PCR. Drug Alcohol Depend. 2012;124:223–8.
Machelska H, Celik MO. Opioid Receptors in immune and glial cells-implications for pain control. Front Immunol. 2020;11:300.
Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroenterol Motil. 2014;26:1386–95.
Corder G, Tawfik VL, Wang D, Sypek EI, Low SA, Dickinson JR, et al. Loss of mu opioid receptor signaling in nociceptors, but not microglia, abrogates morphine tolerance without disrupting analgesia. Nat Med. 2017;23:164–73.
Mathew B, Lennon FE, Siegler J, Mirzapoiazova T, Mambetsariev N, Sammani S, et al. The novel role of the mu opioid receptor in lung cancer progression: a laboratory investigation. Anesth Analg. 2011;112:558–67.
Janku F, Johnson LK, Karp DD, Atkins JT, Singleton PA, Moss J. Treatment with methylnaltrexone is associated with increased survival in patients with advanced cancer. Ann Oncol. 2018;29:1076.
Kanemasa T, Koike K, Arai T, Ono H, Horita N, Chiba H, et al. Pharmacologic effects of naldemedine, a peripherally acting mu-opioid receptor antagonist, in in vitro and in vivo models of opioid-induced constipation. Neurogastroenterol Motil. 2019;31:e13563.
Watari R, Matsuda A, Ohnishi S, Hasegawa H. Minimal contribution of P-gp on the low brain distribution of naldemedine, a peripherally acting mu-opioid receptor antagonist. Drug Metab Pharmacokinet. 2019;34:126–33.
Doi, S, Mori, T, Uzawa, N, Arima, T, Takahashi, T, Uchida, M et al. Characterization of methadone as a beta-arrestin-biased mu-opioid receptor agonist. Mol Pain 2016;12:1744806916654146.
Suda Y, Kuzumaki N, Sone T, Narita M, Tanaka K, Hamada Y, et al. Down-regulation of ghrelin receptors on dopaminergic neurons in the substantia nigra contributes to Parkinson’s disease-like motor dysfunction. Mol Brain. 2018;11:6.
Watkins LR, Wang X, Mustafa S, Hutchinson MR. In vivo veritas: (+)-Naltrexone’s actions define translational importance: a letter in response to Skolnick et al. ‘Translational potential of naloxone and naltrexone as TLR4 antagonists’. Trends Pharm Sci. 2014;35:432–3.
Chan HCS, McCarthy D, Li J, Palczewski K, Yuan S. Designing safer analgesics via mu-opioid receptor pathways. Trends Pharm Sci. 2017;38:1016–37.
Zylla D, Gourley BL, Vang D, Jackson S, Boatman S, Lindgren B, et al. Opioid requirement, opioid receptor expression, and clinical outcomes in patients with advanced prostate cancer. Cancer. 2013;119:4103–10.
Zhang H, Sun M, Zhou D, Gorur A, Sun Z, Zeng W, et al. Increased mu-opioid receptor expression is associated with reduced disease-free and overall survival in laryngeal squamous cell carcinoma. Br J Anaesth. 2020;125:722–9.
Okazaki T, Chikuma S, Iwai Y, Fagarasan S, Honjo T. A rheostat for immune responses: the unique properties of PD-1 and their advantages for clinical application. Nat Immunol. 2013;14:1212–8.
Schietinger A, Greenberg PD. Tolerance and exhaustion: defining mechanisms of T cell dysfunction. Trends Immunol. 2014;35:51–60.
Trapani JA, Smyth MJ. Functional significance of the perforin/granzyme cell death pathway. Nat Rev Immunol. 2002;2:735–47.
Rossaint J, Zarbock A. Perioperative inflammation and its modulation by anesthetics. Anesth Analg. 2018;126:1058–67.
Zhang P, Yang M, Chen C, Liu L, Wei X, Zeng S. Toll-like receptor 4 (TLR4)/opioid receptor pathway crosstalk and impact on opioid analgesia, immune function, and gastrointestinal motility. Front Immunol. 2020;11:1455.
Franchi S, Moretti S, Castelli M, Lattuada D, Scavullo C, Panerai AE, et al. Mu opioid receptor activation modulates Toll like receptor 4 in murine macrophages. Brain Behav Immun. 2012;26:480–8.
Yang X, Jiang X, Chen G, Xiao Y, Geng S, Kang C, et al. T cell Ig mucin-3 promotes homeostasis of sepsis by negatively regulating the TLR response. J Immunol. 2013;190:2068–79.
Souza-Fonseca-Guimaraes F, Parlato M, Philippart F, Misset B, Cavaillon JM, Adib-Conquy M, et al. Toll-like receptors expression and interferon-gamma production by NK cells in human sepsis. Crit Care. 2012;16:R206.
Acknowledgements
The authors thank Ms. Kana Morita, Ms. Arisa Gina, Ms. Anna Hori, Mr. Shoki Matsumura, Mr. Takuya Kurimura, Ms. Natsumi Kawamura and Ms. Mayu Takagi for their help with the experiments.
Funding
This work was supported in part by grants from the MEXT-Supported Program for the Strategic Research Foundation at Private Universities, 2014–2018, S1411019. This research was also supported by Hoshi University.
Author information
Authors and Affiliations
Contributions
EG, YH, TM and Minoru N wrote the manuscript. NK and Minoru N edited the manuscript. Michiko N, YS, KM and NK conducted in vitro studies. YH, YI, AS, DS, MT, SY, KT and KY conducted in vivo studies. HT provided technical support. HA, TY and KH synthesised naldemedine. EG, KA, MI and EI provided medical comments. NK and Minoru N supervised the overall project. All of the authors discussed the results and commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All animal studies were conducted in accordance with the Guiding Principles for the Care and Use of Laboratory Animals at Hoshi University, as adopted by the Committee on Animal Research of Hoshi University.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gondoh, E., Hamada, Y., Mori, T. et al. Possible mechanism for improving the endogenous immune system through the blockade of peripheral μ-opioid receptors by treatment with naldemedine. Br J Cancer 127, 1565–1574 (2022). https://doi.org/10.1038/s41416-022-01928-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01928-x