Abstract
Background
In England, bivalent vaccination (Cervarix) against high-risk human papillomavirus (HR-HPV) genotypes 16/18 was offered in a population-based catch-up campaign in 2008–2010 to girls aged 14–17 years. These women are now entering the national cervical screening programme. We determined the impact of catch-up bivalent vaccination on their screening outcomes.
Methods
We studied the overall and genotype-specific screening outcomes in 108,138 women aged 24–25 (offered vaccination) and 26–29 years (not offered vaccination) included in the English HPV screening pilot between 2013 and 2018.
Results
At 24–25 years, the detection of high-grade cervical intraepithelial neoplasia (CIN2+) associated with HPV16/18 decreased from 3 to 1% (p < 0.001), with estimated vaccine effectiveness of 87% (95% CI: 82–91%). The detection of any CIN2+ halved from 6 to 3% (p < 0.001), with an estimated vaccine effectiveness of 72% (95% CI: 66–77%). The positive predictive value of a colposcopy for CIN2+ decreased for both low-grade (p < 0.001) and high-grade (p = 0.02) abnormalities on triage cytology. The decreases in screen-detected abnormalities at age 26-29 were of a substantially smaller magnitude.
Conclusions
These data confirm high effectiveness of bivalent HPV vaccination delivered through a population-based catch-up campaign in England. These findings add to the rationale for extending screening intervals for vaccinated cohorts.
Similar content being viewed by others
Introduction
Approximately 70% [1] of cervical cancers (and >80% [2] in the UK) are caused by persistent infection with high-risk human papillomavirus (HR-HPV) genotypes 16 and 18. Vaccination targeting these two genotypes is highly effective in the prevention of persistent infections and associated cervical abnormalities including high-grade cervical intraepithelial lesions (CIN) and cancer [3], particularly when administered before sexual debut. The vaccine is still effective when administered later in adolescence and beyond, with somewhat reduced effectiveness due to infections acquired before vaccination [4, 5]. Since September 2008, the HPV vaccine has been routinely administered throughout England, through the national adolescent HPV vaccination programme to girls aged 12–13 years born on or after 1 September 1995 (Supplementary Information, Fig. S1). The delivery of this programme has been largely school-based. A catch-up campaign was also run during the period of 2008–2010, targeting girls aged 14–17 years born between 1 September 1990 and 31 August 1995. The catch-up campaign was provided by a mixture of general practice and school-based delivery. In September 2012, the programme changed from using the bivalent vaccine (Cervarix; GSK, Brentford, UK) to using the quadrivalent vaccine (Gardasil; Merck, Kenilworth, NJ), which also provides protection against genital warts [6]. Both vaccines have been shown to provide some protection against certain other HR-HPV genotypes such as 31 and 45 through cross-protection. The recommended vaccination schedule was originally three doses and changed to two doses in September 2014. All doses are administered free of charge. Vaccination uptake has been consistently high at 80–90% for the routine programme, while the catch-up campaign reached 40–75% of girls, depending on the birth cohort [7].
The National Health Service Cervical Screening Programme (NHS CSP) invites women for their first cervical screening 6 months before their 25th birthday. This means that the first cohorts in the catch-up campaign eligible for vaccination were invited for screening in March 2015. In 2013, a national pilot of primary screening with HR-HPV testing, followed by cytology if HR-HPV positive, was launched in six CSP laboratories. The pilot included ~1.3 million women whose primary screening test was either a HR-HPV test or liquid-based cytology (LBC) [8]. In routine screening, the pilot confirmed that primary screening with HR-HPV testing is more effective than primary screening with LBC in detecting underlying high-grade CIN (CIN2+ and CIN3+), reducing the development of invasive cervical cancer, and allowing longer screening intervals for women who test HR-HPV negative [8]. These data represent the most complete documentation of CSP outcomes in both unvaccinated women and the oldest women who were eligible for catch-up vaccination and who received cervical screening with HR-HPV as the primary test at age 25 years.
The aim of this study was to determine the impact of the catch-up vaccination programme with the bivalent vaccine administered at the age of 14 years and older on screening outcomes in the CSP pilot of HR-HPV testing for primary cervical screening. We report (a) the prevalence of all HR-HPV and, for a subset where this is known, of genotype-specific 16/18 infections, (b) the proportion of women referred to colposcopy, (c) the proportion of women diagnosed with CIN1, CIN2+, CIN3+, and cervical cancer detected by screening, and (d) the positive predictive value (PPV) of colposcopy for CIN2+.
Methods
The pilot has been described in detail [8,9,10]. In summary, the pilot was launched in April 2013 and was embedded in the English CSP, which routinely recalls women aged between 25 and 49 years every 3 years (the first invitation is sent at 24.5 years) and women between 50 and 64 years every 5 years. The laboratories used either ThinPrep (Hologic, Marlborough, MA) or SurePath (BD, Sparks, MD) systems for LBC and APTIMA (Hologic, Manchester, UK), cobas 4800/6800 (Roche, Rotkreuz, Switzerland, or Branchburg, NJ) or RealTime (Abbott, Wiesbaden, Germany) HR-HPV assays. The cobas and RealTime assays were used in four laboratories. These two assays allow partial HR-HPV genotyping by detecting HPV 16 and HPV 18 DNA separately and reporting the detection of the DNA of the “other” 12 HR-HPV genotypes (31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68) in combination. APTIMA, used in two pilot laboratories, reports the detection of mRNA from the same 14 HR-HPV genotypes in combination.
Women screened with HR-HPV tests were returned to routine recall if they tested negative. Samples found to be HR-HPV positive were sent for cytology triage. Women with non-negative cytology were referred to colposcopy at baseline. Non-negative cytology was defined as borderline changes in squamous or endocervical cells or worse, which is approximately consistent with atypical squamous or glandular cells of undetermined significance or worse in the Bethesda 2014 classification. Women with negative cytology had early recalls at 12 and 24 months, although those results could not yet be included in the analysis owing to few women who had undergone early recall after having been first screened in 2016 or later.
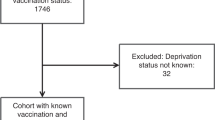
Data from the first (prevalence) round of primary screening by HR-HPV testing were retrieved from the laboratory information systems. These data were available until 31 December 2016 for women screened at 26 years of age or older, and until 31 December 2018 for women screened at 24–25 years of age. For all women with positive HR-HPV tests regardless of their age, follow-up histology diagnoses were available until December 2018. All diagnoses were reported as assigned by the routine services. It was assumed that tests were performed for primary screening if the laboratory had no record of an LBC or HR-HPV test within the previous 2 years and/or the test itself was not marked as a response to a recent abnormality. All other tests were excluded from the analysis. Women were also categorised according to the decile of the Index of Multiple Deprivation (IMD). The IMD is an area-based standard measure of deprivation in England (information on deprivation at the individual level is not routinely collected). In order to determine a woman’s IMD, her postcode at the time of screening was linked to the Lower Layer Super Output Area code in conjunction with the government’s English indices of deprivation report from 2015 [11]. A small number of women with an unknown IMD were excluded from the analysis.
Patient and public involvement
Neither screened women nor the public was involved in the conduct of this study. A study to evaluate women’s psychological responses to HR-HPV testing was embedded in the pilot and its findings have been separately reported [12,13,14].
Statistical analysis
The last of the six laboratories began reporting data to the pilot in August 2013, and women were included in the analysis if they were screened in September 2013 or later. We reported the annual proportions of women (with 95% exact binomial confidence intervals [CI]) with HR-HPV infections detected at baseline screening, HR-HPV infections in combination with non-negative cytology (a proxy for the number of referrals to colposcopy at baseline screening), diagnosis of CIN1, CIN2+, CIN3+ or cervical cancer, either squamous or glandular, after referral to colposcopy at baseline (for all referrals made until 30 June 2018, to give women time to attend the colposcopy), and the PPV of colposcopy for a CIN2+ diagnosis on histology. For the subset of the data from the four genotyping laboratories, we stratified these outcomes according to whether the infecting HR-HPV genotypes were those included in the vaccine (HPV 16/18) or not (12 “other” HR-HPV genotypes). Infections with “other” genotypes were counted independently of any co-infections with HPV 16/18; however, for the analyses of CIN2+ and CIN3+ associated with these “other” HR-HPV genotypes, cases of 16/18 co-infections were excluded, as the latter were the more likely drivers for the development of a CIN lesion. The PPV of colposcopy for CIN2+ was calculated as the proportion of women who underwent a colposcopy because of an HR-HPV-positive baseline test with non-negative triage cytology, with a diagnosis of CIN2+.
The annual trends in the proportions of screened women who had abnormalities detected by screening were tested using log-binomial regression using the glm command with binomial family and log link in Stata 15.0. These models included year as a continuous predictor. All models were adjusted for (a) IMD decile, because women from more deprived backgrounds are known to be more likely to develop CIN and cervical cancer [15, 16], and (b) laboratory, in order to take account of unmeasured local characteristics associated with screening outcomes, to obtain adjusted prevalence ratios (PRadj). Analyses were reported separately for women aged 24–25, 26–27, and 28–29 years at screening.
The observed time trends in screening abnormalities at the age of 24–25 years were compared with the increasing vaccination coverage in the population. Data on the individual vaccination status of women included in the pilot were not available for analysis. As before [17], the age and calendar-year specific probability that a woman was vaccinated was estimated from the official national statistics for vaccination with three doses in the general population, available by school cohort (Supplementary Information, Table S1). To estimate the vaccination coverage in the population of women undergoing screening, we calculated a weighted average of the assigned age and calendar-year specific probabilities for women aged 24 vs. 25 years who participated in screening in the pilot in each calendar year.
The reported time trends in screening outcomes describe the differences between a population to which vaccination had not been offered (earlier years), and a population with an increasing proportion of women who received the vaccination as part of the catch-up campaign and a decreasing proportion of women who were eligible for this vaccination but did not obtain it (later years). As the information on the individual women’s vaccination status was not available, we could not estimate the relative differences in screening outcomes between vaccinated and unvaccinated women (i.e. the vaccine effectiveness) directly. Instead, we used log-binomial regression models that included a continuous variable for the assigned vaccination coverage (as a proportion, see above) to estimate prevalence ratios [18] adjusted for IMD decile and laboratory. These PRadj provided an estimate of the relative differences in the prevalence of screening abnormalities between a fully vaccinated population (100% vaccination coverage) and an unvaccinated population (0% vaccination coverage) for all years combined (2013–2018). The vaccine effect was then estimated by subtracting the PRadj for the vaccination coverage from 1 (i.e. 1 − PRadj) to estimate the reduction in the risk due to vaccination for women who were screened at age 24–25 years. An example of this calculation is presented in the Supplementary Information. To test the robustness of this model, we separately estimated vaccine effectiveness by assuming that the proportion of vaccinated women among those screened was 20% higher than in the analysis described above (see Supplementary Information, Table S1, for absolute values).
Stata version 15 and RStudio version 1.1.463 were used for the analyses.
Results
Screening outcomes at the age of 24–25 years for birth cohorts that were offered vaccination
As part of the pilot, 64,274 women aged 24–25 years were screened using HR-HPV testing between September 2013 and December 2018 (Table 1). During this period, the proportion of women who reached this age and received three doses of the bivalent HPV vaccine increased from 0% to just under 55%, as estimated from population-based statistics (Fig. 1). These women became eligible for vaccination at ages 14–17 years, although for the majority this would be at ages 15–17 years (Supplementary Information, Table S1).
In this age group, the proportion of screened women who had a positive HR-HPV test decreased from 34% in 2013–2014 to 26% in 2018 (Table 1 and Fig. 1; p for trend, adjusted for IMD and laboratory: <0.001). The decrease in the proportion was more pronounced for vaccine genotypes 16/18, where the prevalence in 2018 decreased by about three-quarters compared with the prevalence observed in 2013–2014 (from 13 to 3%; p < 0.001, Fig. 2). HPV genotypes 16 and 18 were less likely to occur in co-infections in cohorts offered vaccination: the proportion of HPV 16/18 infections accounted for almost 40% of all infections in 2013–2014 but fell to just over 10% by 2018 (data not tabulated). The extent of the decrease in overall HR-HPV positivity in the screening population applied similarly to both types 16 and 18 and was similar in those laboratories using DNA assays and those using mRNA assays (Supplementary Information, Figs. S2 and S3, respectively). The change in the population prevalence of the “other” HR-HPV genotypes was much less marked and the proportion with such infections oscillated between 25 and 27% (p = 0.06). The estimated effectiveness of the vaccine (i.e. the estimated relative difference between vaccinated and unvaccinated women) was around 40% against HR-HPV infections overall, and around 90% against HPV 16/18 infections (Table 1).
The proportion of women aged 24–25 years with a HR-HPV-positive screening test and abnormal triage cytology (i.e. those that were referred to colposcopy at baseline) decreased from 13% in 2013–2014 to 9% in 2018 (p < 0.001). The observed proportion of women with CIN1 among those screened oscillated around 2% (p = 0.03). The proportion of those with CIN2+ approximately halved from 6 to 3% (p < 0.001), as did the proportion with CIN3+, which halved from 4 to 2% (p < 0.001). The degree of protection exerted by the vaccine (i.e. the effectiveness) was estimated to be 70–80% for all high-grade CIN lesions (Table 1), while for CIN2+ and CIN3+ associated with HPV 16/18, the vaccine effectiveness was estimated at nearly 90%. For high-grade CIN associated with “other” HR-HPV genotypes, the decrease in the detection was smaller (e.g., CIN2+ associated with these genotypes continued to be detected in 1–2% of the screened population), and the estimated vaccine effectiveness was less than that seen for genotypes 16/18: about 30% for CIN2+ and 60% for CIN3+ (with broad 95% CIs).
Although the unadjusted observed detection of cervical cancer at screening decreased by about 75% between 2013 and 2018 (from >0.1% to <0.05%), the trend did not reach statistical significance. The p value was 0.14, based on 32 cases diagnosed in 2013–2018, and vaccine effectiveness was estimated to be 64% (95% confidence interval (CI): −91 to 93%).
Figure 3 shows that at the age of 24–25 years, the observed time trends were similar for women with more vs. less deprived backgrounds (IMD deciles 1–5 vs. 6–10, respectively). The difference in HR-HPV positivity was small in birth cohorts that were not offered vaccination and remained small even in birth cohorts that were offered catch-up vaccination. Detection of CIN2+ and CIN3+ was higher in women from more deprived backgrounds throughout the observation period. In cohorts offered vaccination, however, the difference in the detection of high-grade CIN between more and less deprived backgrounds became smaller than it was in older cohorts.
The PPV, for CIN2+, of a colposcopy after a positive HR-HPV primary screening test with non-negative triage cytology decreased from 46% in 2013–2014 to 32% in 2018 (Fig. 4). The decreasing trend was observed, particularly after year 2015, in both low-grade (p < 0.001) and high-grade (p = 0.02) cytological abnormalities.
Additional analyses assuming that the proportion of vaccinated women among those who were screened was 20% higher than estimated from the general population data produced slightly lower estimates of vaccine effectiveness (not tabulated). For prevention of HPV 16/18 infections, for example, the estimate decreased from 90% (95% CI: 89–92) to 86% (95% CI: 84–88); for prevention of CIN2+ associated with HPV 16/18 infections, it decreased from 87% (95% CI: 82–91) to 82% (95% CI: 76–86). Similarly, time trends adjusted for IMD and site without specifying any assumption on vaccine effectiveness exhibited, in general, highly statistically significant decreases in the proportions of women with screen-detected abnormalities.
Screening outcomes at the age of 26–29 years for birth cohorts that were not offered vaccination
Between September 2013 and December 2016, 16,864 women aged 26–27 years had a primary screening test, as did 27,000 women aged 27–28 years (Supplementary Information, Tables S2 and S3). Practically none of these women had been offered HPV vaccination (Supplementary Information, Table S1).
In both age groups, decreases in overall HR-HPV prevalence were small, if observed at all (p = 0.20 and p = 0.89, respectively; Fig. 5). Nevertheless, the prevalence of HPV 16/18 decreased by about one-quarter (from 12% in 2013–2014 to 9% in 2018, p < 0.001) in the age group 26–27 years and by about one-seventh (from 8 to 7%, p = 0.01) in the age group 28–29 years, while it decreased by three-quarters in the age group 24–25 years (as shown above). The prevalence of “other” 12 HR-HPV genotypes (in combination) remained stable throughout the observation period (at around 22%, p = 0.88, at age 26–27 years, and at around 17%, p = 0.96, at age 28–29 years).
The proportion with high-grade CIN associated with HPV 16/18 decreased by about one-third in the age group 26–27 years (p = 0.01 for both CIN2+ (from just <4% to just >2%) and CIN3+ (from 3 to 2%)). The decreases were less pronounced at 28–29 years of age (from just >2% to just <2%, p = 0.05, for CIN2+, and from around 2% to around 1%, p = 0.10, for CIN3+). At 26–27 years of age, there was a suggestion of an increase in CIN2+ (from 2 to 3%, p = 0.01) and CIN3+ (from 1 to 2%, p = 0.05) associated with “other” HR-HPV genotypes (using, as explained above, the definition of “other” infections that excluded co-infections with HPV 16/18).
Discussion
Principal findings
This large study of data from a pilot of routine primary screening with HR-HPV testing in England contributes to the body of international studies that show that HPV 16/18 vaccination significantly reduces the risk of high-grade CIN lesions and cervical cancer. The data cover the first 4 years of screening of birth cohorts that were eligible for bivalent Cervarix vaccination through a catch-up campaign at the start of the English HPV vaccination programme. As the average age at sexual debut in the UK is around 16 years, with about 30% of women having their first sexual intercourse before the age of 16 years [19], the “real-life” effectiveness of vaccination was expected to be somewhat less than the efficacy of close to 100% reported in female volunteers who were naive to vaccine genotypes when they entered randomised trials [20]. Nevertheless, the frequency of high-grade CIN diagnoses in the English CSP decreased significantly, with diagnoses related to HPV 16/18 decreasing by about two-thirds, we believe as a direct consequence of the vaccination programme. Overall, these trends implied a protective effect of approximately 90% from the bivalent vaccine administered at 14–17 years of age on high-grade CIN associated with HPV 16/18 infections, and of 30–60% on high-grade CIN associated with infections with “other” HR-HPV genotypes.
When interpreting the causal role of the vaccine in this ecological study, possible independent concurrent factors such as changes in sexual behaviour and background risk should be considered. Increasingly younger age at sexual initiation [21] and an increasing number of sexual partners [19] suggest that it is unlikely that the background risk of HR-HPV infections has decreased among younger birth cohorts. The CSP screening and colposcopy protocols were unchanged throughout the pilot in terms of the selection of women to be invited for screening, as well as the HR-HPV testing protocols and the clinical investigation of the detected infections. The national screening coverage of women aged 25–29 years remained virtually unchanged between 2013 and 2018 [22]. Indeed, the patterns observed in the pilot showed characteristics of dose-response relationships that would be expected for vaccination as a causal factor. The patterns showed specificity in that the decreases were most pronounced for vaccine genotypes. These decreases were first observed when the first cohorts that were offered vaccination entered the CSP and grew as cohorts with higher vaccination coverage and younger age at vaccination started entering the programme.
The ultimate goal of HPV vaccination is to prevent cervical cancer. Recently published data from Sweden confirmed a lower incidence of cervical cancer in women vaccinated with the quadrivalent vaccine [3], while cancer registry data from England confirmed a lower incidence of cervical cancer in women vaccinated with the bivalent vaccine [23]. Our data were consistent with these findings. We observed fewer cases of cancer detected after the first screening invitation at the age of 24–25 years, although our data from this initial period lacks power for cervical cancer outcomes.
Strengths and limitations of the study
The greatest strength of these data is that they were derived from a prospective, large-scale, and real-life pilot study, fully embedded in a highly effective CSP with national quality assurance guidelines and monitoring. It involved successive, unselected women who attended the screening in different areas throughout England. The English CSP, within which this pilot was performed, is one of the few programmes that incorporates HR-HPV testing for primary screening from the age of 25 onwards, so the value of our data stands out in the global context.
Previous real-world studies have had to rely on samples from volunteers, from women seeking health care for other reasons, or from women undergoing cytological screening where HR-HPV infections were determined from archived samples, often using highly sensitive epidemiological HPV assays [5]. In contrast to these earlier studies, all HR-HPV tests in the pilot were performed using the same clinically validated assays that had been selected for the national programme. It can therefore be expected that these data offer reliable predictions for the CSP and other similar programmes.
The estimated vaccine effectiveness against high-grade CIN and HR-HPV infections must be interpreted with caution, as it was established in women who chose to undergo screening and we had no information about their individual vaccination status. Our estimates of vaccination coverage were taken from official national statistics for England. Early Scottish data from the catch-up campaign (from a screening programme that invited women for the first time at the age of 20 years) showed that, regardless of the level of deprivation, fully vaccinated women were more likely to be screened [24]. If the same pattern of screening participation was true in the six pilot areas in England, our regression analyses may have overestimated the differences between vaccinated and unvaccinated women. As shown in sensitivity analyses, however, the findings of high vaccine effectiveness remained robust.
Our study relied on routinely reported diagnoses and high-grade CIN histology was not tested to confirm aetiological associations with specific HR-HPV genotypes. By default, for women with genotyped results, we assumed that CIN was associated with “other” HR-HPV infections if no HPV 16/18 infections were detected in the same screening sample. The apparently increasing trend of high-grade CIN in cohorts not offered vaccination (at ages 26–27 years) may be a consequence of this definition in the context of changing epidemiology of multiple infections involving HPV 16/18, as co-infections of HPV 16/18 and “other” HR-HPV genotypes were more frequent before vaccination [25]. On the other hand, our study also provided an apparently inconsistent finding in cohorts offered vaccination (in our analysis, this refers to women aged 24–25 years), since the vaccine did not affect infections with “other” HR-HPV genotypes, but did have an effect on the high-grade CIN associated with these genotypes. This finding might be explained by cross-protection. Partial cross-protection by the vaccine has been well demonstrated for genotypes 31, 33, and 45 [26]. In unvaccinated populations, these three genotypes were among the genotypes most likely to produce high-grade CIN lesions, which can now be partly prevented by the vaccine [27], but overall they represented a small number compared with all other “other” HR-HPV infections, a majority of which are not prevented by the vaccine [25]. Genotype-specific cross-protection, however, could not be studied, as the available routinely reported HR-HPV test outcomes do not differentiate between the individual 12 “other” HR-HPV genotypes.
Comparison with other studies
As far as the study designs can be compared, the patterns observed in the English pilot in cohorts that were offered vaccination between the ages of 14–17 years were consistent with those observed in previous studies. [5, 26, 28,29,30,31,32] In the PATRICIA randomised controlled trial, the efficacy of the bivalent vaccine against HPV 16/18-related high-grade CIN was close to 100% in women who were naive to HR-HPV before vaccination, but fell to 61% for CIN2+ and 46% for CIN3+ when all vaccinated women were included in the analysis [33]. The latter is lower than our estimates of around 90%, but in the trial, vaccination was administered between the ages of 15 and 25 years, with an average age of 20 years. Some degree of herd protection may have also played a part in making our estimates higher than were efficacy estimates from the trial. In the Scottish CSP, where until recently women received their first invitation for LBC screening at age 20 (as opposed to 24.5 in the English CSP) and individual vaccination status could be obtained from administrative records, it was estimated that bivalent catch-up vaccination administered at 14–17 years of age was about 70% effective against high-grade CIN [28].
Before our analysis, English data were only available from settings such as chlamydia screening or from sexual health clinics. There, the effect of the bivalent vaccine administered at 15–17 years of age against HPV 16/18 infections was estimated to be a 49% reduction [18]. Although this is lower than estimated in our analysis, women participating in chlamydia screening are probably not fully representative of the general population targeted by the CSP. They may have a higher risk of contracting an HR-HPV infection, an earlier age at sexual debut and lower-than-average vaccination uptake, instead of the likely higher-than-average uptake in women attending for cervical screening.
Policy implications
These data indicate an impact of the HPV vaccine both beyond the vaccinated cohorts and beyond the vaccine genotypes. The decrease in high-grade CIN associated with non-vaccine genotypes indicated the presence of partial cross-protection against “other” HR-HPV genotypes, while a decrease in the prevalence of HPV 16/18 infections in older women not included in the catch-up campaign probably indicates some degree of herd protection to those older women. Both effects have already been observed in other routine settings [5, 26, 28]. It is expected that the screening of cohorts that were offered vaccination at the age of 12 or 13 years scheduled to begin in England in 2020, will have an added effect in reducing the incidence of cervical cancer precursor lesions [28]. This in turn will require a national reconsideration of screening target age ranges and intervals, leading to significantly fewer screening rounds during a woman’s lifetime in order to continue to deliver the CSP in a cost-effective manner [34]. More evidence on the safety of extended screening intervals is expected from the reporting of the Finnish randomised controlled trial in women who were vaccinated at either age 13–15 or 18 and thereafter screened in their twenties, where data from the baseline testing has already shown promising results [32].
Several years ago, concern was expressed about the use of cytology for screening vaccinated women, fearing that a decreasing prevalence of cervical lesions would lead to a deterioration in the PPV for CIN2+ [35]. Such decreases have subsequently been demonstrated in real-life settings, for example in Scotland and Sweden [36, 37]. Unlike in these two countries where LBC was used as the primary screening test, women in the English pilot were screened with HR-HPV testing, with LBC reserved for triage of HR-HPV-positive samples. Although the criteria for assessing LBC remained unchanged throughout the pilot, a decline in the PPV was also here observed in both low- and high-grade abnormal, HR-HPV-positive cytology. Among women who were referred to colposcopy in the pilot, the proportion of those with HPV 16/18 infections decreased over time as a consequence of vaccination; in parallel, the proportion referred with infections with “other” HR-HPV genotypes increased from around 50% to around 70% (not tabulated). Colposcopies in women with “other” HR-HPV infections had a lower PPV for CIN2+ (around 30% in women with concurrent abnormal cytology) than did colposcopies with HPV 16/18 infections (around 60%; not tabulated). This difference in the PPV between the two groups of genotypes was consistent with observations from Denmark, where the existing “other” HR-HPV infections, even if they persisted for several years, were less likely to lead to high-grade CIN than did HPV 16/18 [38]. Other potential factors such as differential ascertainment at colposcopy, e.g. due to a lower visibility of non-16/18 CIN lesions, may have also led to a lower PPV associated with “other” HR-HPV infections. In all, the changes in the PPV observed so far at 24–25 years of age, from 46 to 32%, mean that 3.1 (100/32) colposcopies were performed to detect a case of CIN2+ after (catch-up) vaccination, whereas in cohorts that were not offered vaccination this was 2.2 (100/46). The observed reductions in the number of women referred for colposcopy, and in the PPV of those colposcopies, will represent a highly significant change for colposcopy services as nearly half of all colposcopies in the CSP used to be performed in women under 30 years of age [8].
Other programme services that can be expected to be affected by vaccination are those related to cytological evaluation in the triage of HR-HPV infections. While the need for cytology capacity decreased by about 85% when the programme substituted LBC with HR-HPV testing [8], our data showed a further ~20% decrease in HR-HPV positivity at the age of 24–25 years by 2018. This decrease is expected to be even more pronounced once routinely vaccinated women enter the CSP.
Neither our data nor the data from Scotland [16] showed a widening of socioeconomic disparities in terms of the detection of cervical abnormalities at screening. Nevertheless, there are still a number of unvaccinated women, including those from socially disadvantaged backgrounds, who are also less likely to participate in screening [39, 40]. It should be noted that these women will have a lower absolute risk than prior to vaccination, due to partial herd protection [41]. Even higher levels of herd protection can be expected from the vaccination of males as well as females [42, 43], which several countries have adopted relatively recently, including England. Nevertheless, continued monitoring of the incidence of cervical cancer, which is already being carried out [2, 23], will remain crucial in assessing changes in relative social disparities.
In conclusion, our data provide further evidence that the impact of vaccination against HPV 16/18 delivered through a catch-up campaign is impressive. Within the English CSP, these findings add to the rationale for a review of the case for extended screening intervals for cohorts offered vaccination.
References
Munoz N, Bosch FX, Castellsague X, Díaz M, de Sanjose S, Hammouda D, et al. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int J Cancer. 2004;111:278–85.
Mesher D, Cuschieri K, Hibbitts S, Jamison J, Sargent A, Pollock KG, et al. Type-specific HPV prevalence in invasive cervical cancer in the UK prior to national HPV immunisation programme: baseline for monitoring the effects of immunisation. J Clin Pathol. 2015;68:135–40.
Lei J, Ploner A, Elfstrom KM, Wang J, Roth A, Fang F, et al. HPV vaccination and the risk of invasive cervical cancer. N. Engl J Med. 2020;383:1340–8.
Szarewski A, Poppe WA, Skinner SR, Wheeler CM, Paavonen J, Naud P, et al. Efficacy of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine in women aged 15-25 years with and without serological evidence of previous exposure to HPV-16/18. Int J Cancer. 2012;131:106–16.
Drolet M, Benard E, Perez N, Brisson M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. 2019;394:497–509.
Garland SM, Steben M, Sings HL, James M, Lu S, Railkar R, et al. Natural history of genital warts: analysis of the placebo arm of 2 randomized phase III trials of a quadrivalent human papillomavirus (types 6, 11, 16, and 18) vaccine. J Infect Dis. 2009;199:805–14.
Department of Health. Annual HPV vaccine coverage in England in 2010/2011: routine programme for school year 8 females (12 to 13 years old). 2020. https://webarchive.nationalarchives.gov.uk/20130104163933/http://immunisation.dh.gov.uk/annual-hpv-vaccine-coverage-in-england-in-201011-report/. Accessed 1 Dec 2020.
Rebolj M, Rimmer J, Denton K, Tidy T, Mathews C, Ellis K, et al. Primary cervical screening with high risk human papillomavirus testing: observational study. BMJ. 2019;364:l240.
Rebolj M, Brentnall AR, Mathews C, Denton K, Holbrook M, Levine T, et al. 16/18 genotyping in triage of persistent human papillomavirus infections with negative cytology in the English cervical screening pilot. Br J Cancer. 2019;121:455–63.
Green LI, Mathews CS, Waller J, Kitchener H, Rebolj M. Attendance at early recall and colposcopy in routine cervical screening with human papillomavirus testing. Int J Cancer. 2021;148:1850–7.
Department for Communities and Local Government. The English Index of Multiple Deprivation (IMD) 2015 – Guidance. 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/464430/English_Index_of_Multiple_Deprivation_2015_-_Guidance.pdf. Accessed 30 Oct 2018.
McBride E, Marlow L, Forster AS, Moss S, Myles J, Kitchener H, et al. Psychological Impact of Primary Screening (PIPS) for HPV: a protocol for a cross-sectional evaluation within the NHS cervical screening programme. BMJ Open. 2016;6:e014356.
McBride E, Marlow LAV, Forster AS, Ridout D, Kitchener H, Patnick J, et al. Anxiety and distress following receipt of results from routine HPV primary testing in cervical screening: The psychological impact of primary screening (PIPS) study. Int J Cancer. 2020;146:2113–21.
Bennett KF, Waller J, McBride E, Forster AS, Di Gessa G, Kitchener H, et al. Psychosexual distress following routine primary human papillomavirus testing: a longitudinal evaluation within the English Cervical Screening Programme. BJOG. 2021;128:745–54.
Cancer Research UK. Cervical cancer incidence statistics. 2018. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/incidence#heading-Two. Accessed 18 Mar 2018.
Cameron RL, Kavanagh K, Cameron Watt D, Robertson C, Cuschieri K, Ahmed S, et al. The impact of bivalent HPV vaccine on cervical intraepithelial neoplasia by deprivation in Scotland: reducing the gap. J Epidemiol Community Health. 2017;71:954–60.
Checchi M, Mesher D, Mohammed H, Soldan K. Declines in anogenital warts diagnoses since the change in 2012 to use the quadruvalent vaccine in England: data to end 2017. Sex Transm Infect. 2019;95:368–73.
Mesher D, Panwar K, Thomas SL, Edmundson C, Choi YH, Beddows S, et al. The impact of the National HPV Vaccination Program in England using the bivalent HPV vaccine: surveillance of type-specific HPV in young females, 2010-6. J Infect Dis. 2018;218:911–21.
Mercer CH, Tanton C, Prah P, Erens B, Sonnenberg P, Clifton S, et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet. 2013;382:1781–94.
Schiller JT, Castellsague X, Garland SM. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine. 2012;30(Suppl 5):F123–38.
Lewis R, Tanton C, Mercer CH, Mitchell KR, Palmer M, Macdowall W, et al. Heterosexual practices among young people in britain: evidence from three national surveys of sexual attitudes and lifestyles. J Adolesc Health. 2017;61:694–702.
NHS Digital. Cervical Screening Programme, England - 2018-19 [NS]. 2020. https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-annual/england---2018-19. Accessed 5 Sep 2020.
Falcaro M, Castañon A, Ndlela B, Checchi M, Soldan K, Lopez-Bernal J, et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet. 2016;114:576–81.
Palmer TJ, McFadden M, Pollock KG, Kavanagh K, Cuschieri K, Cruickshank M, et al. HPV immunisation and increased uptake of cervical screening in Scottish women; observational study of routinely collected national data. Br J Cancer. 2021;398:2084–92.
Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al. ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening. Health Technol Assess. 2009;13:1–150.
Kavanagh K, Pollock KG, Cuschieri K, Palmer T, Cameron RL, Watt C, et al. Changes in the prevalence of human papillomavirus following a national bivalent human papillomavirus vaccination programme in Scotland: a 7-year cross-sectional study. Lancet Infect Dis. 2017;17:1293–302.
Franceschi S, Clifford GM. Re: A study of the impact of adding HPV types to cervical cancer screening and triage tests. J Natl Cancer Inst. 2005;97:938–9.
Palmer T, Wallace L, Pollock KG, Cuschieri K, Robertson C, Kavanagh K, et al. Prevalence of cervical disease at age 20 after immunisation with bivalent HPV vaccine at age 12-13 in Scotland: retrospective population study. BMJ. 2019;365:l1161.
Bhatia R, Kavanagh K, Cubie HA, Serrano I, Wennington H, Hopkins M, et al. Use of HPV testing for cervical screening in vaccinated women-Insights from the SHEVa (Scottish HPV Prevalence in Vaccinated Women) study. Int J Cancer. 2016;138:2922–31.
Cameron RL, Kavanagh K, Pan J, Love J, Cuschieri K, Robertson C, et al. Human papillomavirus prevalence and herd immunity after introduction of vaccination program, Scotland, 2009-13. Emerg Infect Dis. 2016;22:56–64.
Brotherton JM, Gertig DM, May C, Chappell G, Saville M. HPV vaccine impact in Australian women: ready for an HPV-based screening program. Med J Aust. 2016;204:184–184e1.
Louvanto K, Eriksson T, Gray P, Apter D, Baussano I, Bly A, et al. Baseline findings and safety of infrequent vs. frequent screening of human papillomavirus vaccinated women. Int J Cancer. 2020;147:440–7.
Lehtinen M, Paavonen J, Wheeler CM, Jaisamrarn U, Garland SM, Castellsagué X, et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13:89–99.
Landy R, Windridge P, Gillman MS, Sasieni PD. What cervical screening is appropriate for women who have been vaccinated against high risk HPV? A simulation study. Int J Cancer. 2018;142:709–18.
Franco EL, Cuzick J, Hildesheim A, de Sanjosé S. Chapter 20: Issues in planning cervical cancer screening in the era of HPV vaccination. Vaccine. 2006;24(Suppl 3):S3/171–7.
Palmer TJ, McFadden M, Pollock KG, Kavanagh K, Cuschieri K, Cruickshank M, et al. HPV immunisation and cervical screening-confirmation of changed performance of cytology as a screening test in immunised women: a retrospective population-based cohort study. Br J Cancer. 2016;114:582–9.
Lei J, Ploner A, Lehtinen M, Sparén P, Dillner J, Elfström KM. Impact of HPV vaccination on cervical screening performance: a population-based cohort study. Br J Cancer. 2020;123:155–60.
Sand FL, Munk C, Frederiksen K, Junge J, Iftner T, Dehlendorff C, et al. Risk of CIN3 or worse with persistence of 13 individual oncogenic HPV types. Int J Cancer. 2019;144:1975–82.
Bowyer HL, Dodd RH, Marlow LA, Waller J. Association between human papillomavirus vaccine status and other cervical cancer risk factors. Vaccine. 2014;32:4310–6.
Tanton C, Soldan K, Beddows S, Mercer CH, Waller J, Field N, et al. High-risk human papillomavirus (HPV) infection and cervical cancer prevention in Britain: evidence of differential uptake of interventions from a probability survey. Cancer Epidemiol Biomark Prev. 2015;24:842–53.
Johnson HC, Lafferty EI, Eggo RM, Louie K, Soldan K, Waller J, et al. Effect of HPV vaccination and cervical cancer screening in England by ethnicity: a modelling study. Lancet Public Health. 2018;3:e44–51.
Gray P, Kann H, Pimenoff VN, Eriksson T, Luostarinen T, Vänskä S, et al. Human papillomavirus seroprevalence in pregnant women following gender-neutral and girls-only vaccination programs in Finland: a cross-sectional cohort analysis following a cluster randomized trial. PLoS Med. 2021;18:e1003588.
Vänskä S, Luostarinen T, Baussano I, Apter D, Eriksson T, Natunen K, et al. Vaccination with moderate coverage eradicates oncogenic human papillomaviruses if a gender-neutral strategy is applied. J Infect Dis. 2020;222:948–56.
Acknowledgements
Data for this study are based on information collected and quality assured by the Public Health England Population Screening Programmes. Access to the data was facilitated by the Public Health England Office for Data Release.
Funding
The English HPV pilot was funded by Public Health England. Public Health England had a role in designing the pilot; in the collection of the data; and commented on the manuscript. MR was supported by Cancer Research UK (reference: C8162/A27047). CM was supported by Cancer Research UK (reference: C8162/A27047) and Public Health England (reference: ODR 1718_428). FP was supported by Cancer Research UK (reference: C8162/A25356). Cancer Research UK had no role in designing the study, in the collection of the data, and in the writing of the manuscript. The authors made the decision to submit.
Author information
Authors and Affiliations
Contributions
Design of the study in this manuscript: MR, DM. Data management: CM. Data analysis: FP. Interpretation of the results: all authors. First draft: MR. Critical comment: all authors. Decision to submit: all authors.
Corresponding author
Ethics declarations
Competing interests
MR: funding from Public Health England for the epidemiological evaluation of the HPV primary screening pilot; attended meetings with various HPV assay manufacturers; fee for lecture from Hologic paid to employer (2018); member of various groups convened by Public Health England providing advice to the English Cervical Screening Programme. CM: held an honorary appointment at Public Health England to process the data for the pilot. FP: declares no conflict of interest. DM and KS: The Blood Safety, Hepatitis, Sexually Transmitted Infections (STI) and HIV Service has provided GSK with post-marketing surveillance reports on HPV infections; a cost recovery charge is made for these reports. HK: Former chair of the Advisory Committee for Cervical Screening (Public Health England), but the views expressed in this manuscript are those of the author and do not represent the view of Public Health England.
Ethics approval and consent to participate
The study was considered the first stage in national implementation, so it was referred to as an implementation pilot and therefore exempt from ethics approval. Women participating in the HPV primary screening pilot were invited to make an informed choice on participating in the cervical screening programme. A decision is made to accept or decline a screening test based on access to accurate and up-to-date information on the condition being screened for, the testing process and potential outcomes. Specific information was provided at the invitation stage allowing for personalised informed choice. There was further opportunity to reflect on what the test and its results might mean when they attended the screening with the clinician taking the sample. Regulation 5, Health Service Regulations 2002, Confidentiality Advisory Group Reference 15/CAG/0207, was the legal basis to process the data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rebolj, M., Pesola, F., Mathews, C. et al. The impact of catch-up bivalent human papillomavirus vaccination on cervical screening outcomes: an observational study from the English HPV primary screening pilot. Br J Cancer 127, 278–287 (2022). https://doi.org/10.1038/s41416-022-01791-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01791-w
This article is cited by
-
Predictable changes in the accuracy of human papillomavirus tests after vaccination: review with implications for performance monitoring in cervical screening
British Journal of Cancer (2024)
-
An Updated Analysis of the Impact of HPV Vaccination Based on Long-term Effectiveness in the Netherlands
Infectious Diseases and Therapy (2023)
-
Supporting the implementation of new healthcare technologies by investigating generalisability of pilot studies using area-level statistics
BMC Health Services Research (2022)